Abstract
Background
The increase in cannabis potency may have treatment implications for cannabis use disorder (CUD). Given the reported increase in prevalence of cannabis use among adults, there is a need to understand substance use treatment needs for CUD.
Methods
We examined demographics and behavioral health indicators of adults aged ≥18 years that met criteria for past-year CUD (n=10,943) in the 2005–2013 National Surveys on Drug Use and Health. We determined prevalence and correlates of past-year treatment use for alcohol/drug, any drug, and cannabis use related problems, to inform treatment efforts for CUD.
Results
The majority of adults with past-year CUD were young adults aged 18-25 or men, had low income, and did not attend college. Two-thirds of adults with CUD met criteria for cannabis dependence, which was comparatively common among younger adults, women, low-income or publicly insured adults, and college-educated adults. Nicotine dependence (40.92%) and alcohol (44.07%) or other drug use disorder (19.70%) were prevalent among adults with CUD. Overall, less than 13% of adults with CUD had received alcohol/drug use treatment the past year; only 7.8% received cannabis-specific treatment. There was no significant yearly variation in treatment use prevalence over 9 years. In particular, Asian-Americans, women, and college-educated adults underutilized cannabis-specific treatment.
Conclusions
This large sample of adults with CUD reveals pervasive underutilization of cannabis-related treatment, especially in women, married adults, and those with college education, despite a high proportion of comorbid behavioral health problems.
Keywords: Asian American, Black, Cannabis use disorder, Hispanic, Mixed race, Native American, Substance use treatment
1. Introduction
Various sources suggest that cannabis potency-levels have progressively increased (Office of National Drug Control Policy [ONDCP], 2015; Drug Enforcement Administration [DEA], 2016). The average THC potency of traditional leafy marijuana seizures was 12% in 2014, compared with 4% in 1995; and the average THC content of marijuana concentrate seizures (“hash-oil”) increased from 13% in 1995 to 55% in 2014 (DEA, 2016). The higher potency of cannabis preparation raises concerns of potential adverse effects associated with problem cannabis use (CU) (cannabis-related disorders, motor-vehicle accidents, medical complications) and support the opportunity to monitor cannabis-related treatment needs (Copeland and Pokorski, 2016; Freeman and Swift, 2016; Volkow et al., 2014).
An estimated 32.9 million adults (13.6% of Americans aged ≥18 years) used cannabis in the past year in 2015 (Center for Behavioral Health Statistics and Quality [CBHSQ], 2016a). Cannabis use disorder (CUD) is the most prevalent illicit/nonmedical drug use disorder, affecting approximately 4.0 million Americans in 2015 or 52% of individuals with an illicit/nonmedical drug use disorder (CBHSQ, 2016a). Current CU prevalence among adults has increased: from 16-17.0% in the early 2000s to 19.8% in 2015 among those aged 18-25 years; and from 4.0% to 6.5% among adults 26 year old or older (CBHSQ, 2016b). While the overall CUD prevalence appeared to remain stable in recent years (CBHSQ, 2016b), an analysis of 340,456 adults suggested an increased trend in monthly and weekly CU, especially among minority groups (Wu et al., 2016). In the total adult sample, the odds of weekly CU and monthly CU were greater among blacks, native-Americans, and mixed-race adults than whites; and among cannabis users, the odds of CUD were greater among blacks, native-Americans, and Hispanics than whites (Wu et al., 2016). Young adults, men and less-educated adults also showed elevated odds of CUD, reinforcing the suggestion to monitor CUD treatment needs (Wu et al., 2014, 2016).
According to data from the Treatment Episode Data Set (TEDS), primary cannabis abuse accounted for 15% of all substance use treatment admissions in 2014 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2016). The average age of cannabis-related treatment admission was 26 years, and minority groups accounted for 56% of primary cannabis-involved admissions (SAMHSA, 2016). Given the large number of cannabis users, a significant increase in CU coupled with an elevated cannabis preparation potency may generate an impact on healthcare resource utilization (CBHSQ, 2016b; Freeman and Swift, 2016). For example, findings from Drug Abuse Warning Network data reveal an increased trend in cannabis-involved emergency department (ED) visits, and the prevalent ED visits were noted among blacks/African-Americans (Zhu and Wu, 2016). Moreover, cannabis-involved ED visits among adults (especially older adults) were associated with increased odds of inpatient hospitalizations relative to adolescents (Zhu and Wu, 2016).
Seven states recently have legalized recreational CU among adults; 28 states and Washington D.C. have approved medical cannabis use; and 16 states consider cannabidiol use legal, suggesting that over 80% of states approve some form of cannabis use in the United States (DEA, 2016). The generalized changes in cannabis laws (legalization, decriminalization) may have unintended effects on CU and cannabis-related problems (Volkow et al., 2014, 2016). An analysis of national survey data showed that adult respondents in states with medical marijuana laws had higher odds of CU and CUD than adult respondents in states without such laws (Cerdá et al., 2012). Although absolute medical harms associated with extensive shifts in cannabis policy are difficult to quantify due to inherent confounding factors and data limitations, recent reports suggest an increase in demand for cannabis-related treatment (Colorado Department of Public Safety [CDPS], 2016; Compton and Baler, 2016). Mair et al. (2015) found that the density of local cannabis dispensaries was positively associated with cannabis-related hospitalizations. Another study reported a 10-20% increase in cannabis-related treatment admissions among men after the passage of medical cannabis laws (Chu, 2014). Data from Colorado indicate significant increases in cannabis-related ED visits and hospitalizations (CDPS, 2016; Kim et al., 2016).
While causality remains unclear, studies have documented associations of chronic or frequent CU with substance use disorders (SUDs), medical conditions (chronic bronchitis symptoms, cardiovascular diseases, depression, psychotic symptoms), and driving injuries (Blanco et al., 2016; Jouanjus et al., 2014; Monte et al., 2015; Volkow et al., 2014). Further, a high proportion of recent/active cannabis users has CUD. Using the national survey data, it was estimated that as many as 19% of past-year cannabis users aged 18-25, and 9-13% of cannabis users aged 26-49 meet criteria for past-year CUD (Wu et al., 2014). The impact of cannabis-involved harms is associated with cannabis potency, number of cannabis users, and indicators of problem use (CUD, cannabis-related medical events) (Freeman and Winstock, 2015). The combined rise in prevalence of CU, cannabis potency, and cannabis-involved ED admissions suggest a potential impact of CU on the burden of the health system (Compton and Baler, 2016; Hasin et al. 2015; Volkow et al., 2014; Zhu and Wu, 2016).
Here, we utilize a large sample of adults from the 2005–2013 National Surveys on Drug Use and Health (NSDUH) to gauge prevalence and correlates of alcohol/drug treatment use among adults with CUD to inform intervention efforts. The use of the large sample is critical to understanding population-level treatment use prevalence and inform disparity for demographic groups. Some racial/ethnic groups (blacks, mixed-race individuals, native-Americans) appear to have a higher prevalence of past-year CUD than whites (Wu et al., 2014, 2016). Findings from the TEDS also revealed that cannabis was among the most commonly identified illicit/nonmedical drugs for treatment admissions among blacks (27%), Hispanics (20%), and Asians/Pacific Islanders (20%), while cannabis accounted for just 11% of annual treatment admissions among whites (SAMHSA, 2016). TEDS data suggest that racial/ethnic minority groups may be over-represented among cannabis-using patients at substance use treatment facilities. However, TEDS data reflect treatment admissions that are confounded by the possibility of multiple admissions among frequent treatment users, which provide inadequate information about prevalence and correlates of treatment use for CUD.
We analyze the national sample of adults drawn from the NSDUH to gauge prevalence and correlates of treatment use among adults with CUD. We examine treatment use for alcohol, drug use, and CU, respectively, to understand the fuller extent of substance treatment use among adults with CUD (i.e., whether treatment is related to cannabis or other substances). Following Andersen's healthcare utilization model, we examine correlates of treatment use in three domains found to influence treatment-seeking: predisposing/demographic variables (race/ethnicity, age, sex, marital status); enabling variables (family income, education, health insurance, county type of residence); and need-related factors (CUD status, other SUD, mental health) (Andersen, 1995; Fleury et al., 2014; Wu et al., 2003, 2007, 2012). Given the reported concern with CU problems and treatment admissions among minority groups (SAMHSA, 2016; Wu et al., 2016), we evaluate racial/ethnic differences in prevalence of behavioral health indicators (cannabis dependence, major depressive episode, other SUD), treatment use (alcohol/drug, any drug, cannabis-specific), and location/setting.
2. Methods
2.1. Data source
The annual NSDUH is the primary national survey designed to provide ongoing estimates of substance use and SUDs among civilian, non-institutionalized individuals aged ≥12 years in the United States (SAMHSA, 2006, 2014). It uses cross-sectional designs to provide substance use related estimates. The target population consisted of residents of households (including shelters, rooming houses, and group homes) from the 50 states and civilians residing on military bases. The survey used stratified, multistage area probability sampling methods to select a representative sample of the U.S. population aged ≥12 years.
NSDUH data collection used a face-to-face household interview approach. Computer-assisted personal interviewing, in which interviewers read less-sensitive questions to respondents and enter the respondents' answers on the laptop, was employed to collect demographic information. Substance use and health-related questions were assessed by an audio computer-assisted self-interviewing method (in which respondents read or listen to the questions on headphones and then enter their answers directly on the NSDUH laptop computer) to increase honest reports of sensitive behaviors (Turner et al., 1998).
We analyzed adult samples (aged ≥18 years) of public-use datasets from nine survey years (2005–2013) (n=36,965–39,133/year) to characterize substance use treatment among adults with CUD. The NSDUH implemented changes in the survey design in 2005 and in 2014. Data from prior (2004) and later (2014) years were not included for this analysis. The 2005–2013 years used similar designs to allow analysis of the same variables to study treatment use. Weighted response rates of household screening and interviewing for these years were 84–91% and 72– 76%, respectively (SAMHSA, 2006, 2014). In the 2005-2013 adult sample (unweighted N=340,456), 1.47% (unweighted n=10,943) met criteria for past-year CUD, which formed the analysis sample.
2.2. Study variables
Demographics
The NSDUH defined seven mutually exclusive racial/ethnic groups based on respondents' self-reported race and ethnicity: non-Hispanic white, non-Hispanic black, non-Hispanic native-American (American Indian/Alaska-native), non-Hispanic native-Hawaiian/Pacific-Islander, non-Hispanic Asian-American, mixed-race (>1 race), and Hispanic. Respondents' self-reported age, sex, family income, marital status, county type, health insurance, and educational level were included as covariates (Hasin et al., 2015; Wu et al., 2014, 2016).
CU and CUD
CU was defined as any self-reported illicit (nonmedical) use of cannabis/hashish. Respondents were read the following: “Marijuana is also called pot or grass. Marijuana is usually smoked, either in cigarettes called joints or in a pipe. It is sometimes cooked in food. Hashish is a form of marijuana that is also called hash. It is usually smoked in a pipe. Another form of hashish is hash oil.” The survey assessed cannabis use status. Respondents who used cannabis in the past year were then assessed for cannabis-specific abuse and dependence symptoms in the past year based on DSM-IV criteria (APA, 2000). Consistent with DSM-IV's hierarchical definition for CUD (cannabis abuse or dependence), cannabis abuse included presence of ≥1 abuse symptom and absence of dependence, and cannabis dependence included presence of ≥3 dependence symptoms, regardless of the abuse status (APA, 2000). This definition indicated a more severe status of dependence than abuse, and we examined whether cannabis dependence was associated with greater odds of treatment use than cannabis abuse.
Behavioral health indicators
As in the case of CUD, respondents who reported alcohol or other drug use in the past year were assessed by structured, substance-specific questions designed to operationalize DSM-IV criteria for abuse of or dependence on each individual substance class (cocaine, heroin, hallucinogens, inhalants, prescription opioids, stimulants/amphetamines, tranquilizers, or sedatives). Current (past-month) nicotine dependence was assessed by the Nicotine Dependence Syndrome Scale (NDSS) and the Fagerström Test of Nicotine Dependence (FTND) (Shiffman et al., 2004; Heatherton et al., 1991). The NSDUH categorized respondents as having nicotine dependence in the past month if they met criteria for dependence as specified by NDSS or FTND. Given the association between CUD and major depression, we examined past-year major depressive episodes (MDE) as a correlate of treatment use (Fleury et al., 2014). Questions assessing past-year MDE were based on DSM-IV criteria that were adapted from National Comorbidity Survey Replication (Kessler et al., 2005).
Past-year substance use treatment
Respondents' treatment use was assessed by separate questions that asked about the receipt of treatment for use of alcohol or drugs and for any drug (e.g., “During the past 12 months, that is since [DATE FILL] have you received treatment or counseling for your use of alcohol or any drug, not counting cigarettes?”). Among respondents who reported the receipt of treatment or counseling for drug use, the survey assessed drug-specific treatment use during their most recent treatment use. Cannabis-specific treatment included the receipt of treatment or counseling for the respondent's use of marijuana/hashish. Among respondents who reported the receipt of alcohol/drug treatment in the past year, we examined their treatment locations: hospital (inpatient), alcohol/drug rehabilitation facility (inpatient, outpatient), mental health facility (outpatient), emergency department, private doctor's office, self-help group (Alcoholics Anonymous, Narcotics Anonymous), and prison/jail.
2.3. Data analysis
We examined demographic distributions and prevalence of MDE and other SUDs among adults with CUD by race/ethnicity. We compared differences in demographics, MDE, and other SUDs by CUD status (dependence vs. abuse) using descriptive and logistic regression analysis. We calculated prevalence of treatment use (alcohol/drug, drug, cannabis) and location by CUD status. We conducted logistic regression analyses to identify factors associated with treatment use. All analyses took into account the NSDUH's complex designs, such as weighting and clustering (StataCorp, 2013). Weighted estimates are used for all prevalence and odds ratio results.
3. Results
3.1. Sociodemographics of adults with CUD (Table 1)
Table 1. Characteristics of adults aged ≥ 18 years with past-year cannabis use disorder: 2005-2013 NSDUH.
| Race/ethnicity Sample size, unweighted |
Total n=10,943 |
White n=6,406 |
Black n=1,841 |
Native-American n=325 |
Native-Hawaiian/Pacific-Islander n=64 |
Asian-American n=197 |
Mixed-Race n=489 |
Hispanic n=1,621 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weighted % | % (SE) | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Age in years | |||||||||||||||
| 18–25 | 56.46 (0.90) | 55.98 | 53.52-58.41 | 49.42 | 45.75-53.11 | 58.18 | 47.89-67.81 | 94.40 | 78.80-98.71 | 64.36 | 50.18-76.40 | 55.27 | 43.09-66.86 | 65.87 | 60.48-70.87 |
| 26–34 | 21.05 (0.81) | 19.59 | 17.79-21.53 | 25.65 | 21.83-29.88 | 22.82 | 14.68-33.68 | 0 | ….…. | 22.58 | 12.92-36.45 | 20.54 | 11.98-32.95 | 21.35 | 17.21-26.17 |
| 35–49 | 15.68 (0.64) | 16.84 | 15.20-18.62 | 18.17 | 15.45-21.25 | 19.00 | 11.87-28.99 | 1.77 | 0.25-11.32 | 12.55 | 5.06-27.88 | 17.39 | 10.31-27.81 | 7.72 | 5.46-10.82 |
| 50+ | 6.81 (0.70) | 7.59 | 5.75-9.95 | 6.76 | 4.33-10.39 | 0 | ….…. | 3.83 | 0.54-22.76 | 0.51 | 0.10-2.46 | 6.79 | 2.63-16.44 | 5.06 | 2.43-10.23 |
|
| |||||||||||||||
| Sex | |||||||||||||||
| Male | 69.54 (0.64) | 68.69 | 66.80-70.53 | 69.90 | 67.00-72.64 | 67.33 | 56.88-76.31 | 75.68 | 51.42-90.14 | 72.86 | 62.42-81.27 | 64.74 | 54.75-73.58 | 72.90 | 69.10-76.39 |
| Female | 30.46 (0.64) | 31.31 | 29.47-33.20 | 30.10 | 27.36-33.00 | 32.67 | 23.69-43.12 | 24.32 | 9.86-48.58 | 27.14 | 18.73-37.58 | 35.26 | 26.42-45.25 | 27.10 | 23.61-30.90 |
|
| |||||||||||||||
| Education | |||||||||||||||
| Less than high school | 23.78 (0.64) | 19.41 | 17.87-21.05 | 31.29 | 27.91-34.88 | 42.75 | 32.22-53.98 | 17.47 | 8.22-33.36 | 5.69 | 2.72-11.52 | 21.76 | 14.41-31.46 | 33.86 | 29.80-38.17 |
| High school | 34.01 (0.80) | 32.18 | 30.47-33.93 | 39.41 | 35.09-43.90 | 35.76 | 28.03-44.30 | 49.71 | 30.48-69.04 | 16.86 | 11.58-23.89 | 29.54 | 23.67-36.18 | 37.27 | 33.27-41.45 |
| Some college | 29.40 (0.74) | 31.90 | 30.11-33.75 | 24.61 | 20.96-28.67 | 20.19 | 14.13-28.00 | 32.35 | 15.37-55.72 | 46.65 | 34.69-59.02 | 34.97 | 25.42-45.90 | 22.59 | 20.05-25.35 |
| College degree or more | 12.81 (0.55) | 16.51 | 15.01-18.14 | 4.69 | 3.44-6.36 | 1.31 | 0.41-4.10 | 0.47 | 0.07-3.15 | 30.79 | 21.67-41.71 | 13.73 | 8.04-22.46 | 6.29 | 4.21-9.28 |
|
| |||||||||||||||
| Marital status | |||||||||||||||
| Married | 15.32 (0.77) | 17.59 | 15.60-19.76 | 9.70 | 7.37-12.67 | 9.73 | 5.88-15.68 | 9.11 | 3.07-24.06 | 11.06 | 5.05-22.53 | 21.58 | 12.84-33.95 | 13.32 | 10.34-17.00 |
| Separated/divorced/widowed | 10.00 (0.69) | 11.04 | 9.43-12.88 | 8.86 | 6.37-12.21 | 13.00 | 6.85-23.30 | 0 | ….…. | 2.19 | 0.61-7.56 | 9.27 | 5.68-14.76 | 8.26 | 5.46-12.31 |
| Never married/single | 74.68 (0.89) | 71.38 | 69.14-73.52 | 81.43 | 77.83-84.57 | 77.27 | 67.72-84.63 | 90.89 | 75.94-96.93 | 86.74 | 73.96-93.78 | 69.15 | 58.64-78.00 | 78.41 | 73.47-82.65 |
|
| |||||||||||||||
| Total annual family income | |||||||||||||||
| <$50,000 | 66.21 (0.81) | 60.26 | 58.14-62.35 | 82.96 | 79.42-86.00 | 85.29 | 78.58-90.16 | 74.95 | 57.12-87.05 | 48.94 | 36.29-61.73 | 59.52 | 48.83-69.39 | 71.11 | 67.03-74.88 |
| $50,000–$74,999 | 12.64 (0.56) | 14.04 | 12.56-15.65 | 8.18 | 6.26-10.61 | 10.39 | 6.22-16.84 | 12.41 | 5.46-25.79 | 20.12 | 12.06-31.63 | 26.80 | 18.17-37.65 | 9.73 | 7.77-12.11 |
| $75,000+ | 21.15 (0.79) | 25.70 | 23.68-27.83 | 8.86 | 6.94-11.25 | 4.32 | 2.34-7.84 | 12.64 | 3.68-35.42 | 30.94 | 21.13-42.82 | 13.67 | 9.43-19.41 | 19.16 | 15.73-23.13 |
|
| |||||||||||||||
| County type | |||||||||||||||
| Large metropolitan | 57.21 (0.90) | 52.19 | 50.07-54.30 | 66.58 | 62.95-70.03 | 25.45 | 15.76-38.39 | 39.99 | 24.05-58.37 | 78.66 | 67.70-86.64 | 44.03 | 35.16-53.29 | 67.84 | 63.36-72.01 |
| Small metropolitan | 32.06 (0.76) | 35.63 | 33.69-37.62 | 24.68 | 21.75-27.87 | 29.58 | 20.21-41.05 | 42.84 | 21.83-66.80 | 19.91 | 12.01-31.15 | 44.50 | 35.70-53.66 | 26.51 | 22.62-30.81 |
| Nonmetropolitan | 10.73 (0.48) | 12.18 | 11.03-13.44 | 8.73 | 6.76-11.21 | 44.97 | 34.39-56.01 | 17.17 | 5.05-44.68 | 1.43 | 0.64-3.18 | 11.47 | 8.13-15.94 | 5.65 | 4.37-7.27 |
|
| |||||||||||||||
| Health insurance | |||||||||||||||
| Private | 49.09 (0.76) | 56.35 | 54.19-58.50 | 33.26 | 30.06-36.62 | 16.46 | 9.17-27.78 | 48.79 | 28.64-69.35 | 65.09 | 52.86-75.61 | 48.97 | 40.04-57.97 | 39.37 | 35.73-43.12 |
| Public | 20.36 (0.69) | 15.37 | 13.74-17.16 | 31.30 | 27.73-35.11 | 55.20 | 43.89-66.00 | 20.29 | 11.63-32.99 | 15.97 | 8.06-29.17 | 26.58 | 20.85-33.22 | 24.23 | 20.31-28.64 |
| None | 30.55 (0.74) | 28.28 | 26.55-30.07 | 35.44 | 32.06-38.97 | 28.34 | 21.51-36.33 | 30.92 | 13.51-56.19 | 18.94 | 12.35-27.92 | 24.45 | 17.10-33.68 | 36.41 | 32.61-40.37 |
SE: standard error; CI: confidence interval. Boldfaced: The estimate in the given racial/ethnic group differed from the estimate in the given group among whites (P< 0.05).
Among adults with CUD (n=10,943), 38.84% were non-whites (blacks 18.92%, Hispanics 14.48%, others 5.44%), 56.46% were young adults aged 18-25, 69.54% were men, 57.79% had not attended college, 74.68% were single, 66.21% had low family income (<$50,000/year), 57.21% resided in large metropolitan areas, and about one-half had either public (20.36%) or no (30.55%) health insurance.
Compared with whites, native-Hawaiians/Pacific-Islanders and Hispanics included more young adults aged 18-25, while Blacks had a higher proportion of adults aged 26-34. Compared with whites, higher proportions of blacks, native-Americans, and Hispanics had not completed high school, had low family income (<$50,000), and had public or no insurance. A higher proportion of mixed-race adults than whites had public insurance, and a lower proportion of mixed-race adults than whites in the high-income category (≥$75,000). Asian-Americans had the highest proportion of adults that attended college or had health insurance.
3.2. Behavioral health among adults with CUD (Table 2)
Table 2. Prevalence of major depressive episode and substance use disorders among adults with past-year cannabis use disorder: 2005-2013 NSDUH.
| Race/ethnicity Sample size, unweighted |
Total n=10,943 |
White n=6,406 |
Black n=1,841 |
Native-American n=325 |
Native-Hawaiian/Pacific-Islander n=64 |
Asian-American n=197 |
Mixed-Race n=489 |
Hispanic n=1,621 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weighted % | % (SE) | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Major depressive episode† * | 18.25 (0.61) | 20.00 | 18.47-21.62 | 13.80 | 11.39-16.63 | 16.35 | 9.86-25.87 | 11.25 | 1.94-44.80 | 15.63 | 8.69-26.50 | 29.02 | 19.80-40.38 | 15.80 | 12.67-19.54 |
| Any other substance use disorder | 69.36 (0.72) | 71.41 | 69.62-73.13 | 66.85 | 63.21-70.31 | 72.72 | 59.14-83.08 | 76.45 | 51.19-90.95 | 66.10 | 55.52-75.29 | 64.12 | 53.66-73.38 | 64.78 | 60.79-68.59 |
| Alcohol or other drug use disorder† | 51.34 (0.76) | 52.03 | 50.07-53.98 | 46.77 | 43.14-50.44 | 60.85 | 43.14-50.44 | 58.62 | 35.90-78.18 | 42.45 | 33.00-52.49 | 42.67 | 33.51-52.36 | 55.95 | 51.98-59.85 |
| Nicotine dependence‡ | 40.92 (0.77) | 44.05 | 41.93-46.19 | 41.64 | 37.44-45.97 | 35.08 | 25.60-45.89 | 32.58 | 21.14-46.56 | 35.08 | 23.92-48.15 | 39.54 | 30.41-49.47 | 28.37 | 24.54-32.55 |
| Alcohol use disorder† | 44.07 (0.83) | 43.96 | 41.79-46.15 | 41.61 | 37.99-45.32 | 53.34 | 43.30-63.12 | 43.57 | 29.71-58.51 | 40.08 | 30.45-50.54 | 38.39 | 29.56-48.05 | 48.42 | 44.65-52.21 |
| Any other drug use disorder† | 19.70 (0.52) | 20.83 | 19.39-22.34 | 14.19 | 11.93-16.78 | 23.53 | 15.83-33.48 | 19.90 | 6.52-46.92 | 8.92 | 5.40-14.39 | 13.99 | 10.25-18.81 | 24.16 | 19.79-29.15 |
| Opioid use disorder† | 9.67 (0.48) | 11.37 | 10.31-12.53 | 3.77 | 2.82-5.03 | 15.89 | 9.16-26.15 | 15.21 | 3.88-44.38 | 3.15 | 1.14-8.41 | 5.99 | 4.36-8.17 | 11.01 | 7.88-15.19 |
| Cocaine use disorder† | 8.19 (0.39) | 7.41 | 6.46-8.50 | 8.39 | 6.52-10.73 | 7.75 | 4.15-14.00 | 7.62 | 2.15-23.65 | 3.94 | 1.60-9.37 | 5.41 | 3.10-9.28 | 12.25 | 9.18-16.17 |
| Tranquilizer use disorder† | 3.51 (0.32) | 4.11 | 3.43-4.91 | 1.21 | 0.71-2.04 | 3.10 | 1.14-8.18 | 0 | ….…. | 0.61 | 0.14-2.60 | 2.26 | 1.25-4.07 | 4.70 | 2.48-8.73 |
| Hallucinogen use disorder† | 3.44 (0.27) | 3.61 | 3.03-4.29 | 3.07 | 2.18-4.30 | 3.92 | 1.84-8.17 | 0 | ….…. | 1.14 | 0.30-4.17 | 2.84 | 1.38-5.76 | 3.66 | 2.09-6.31 |
| Stimulant use disorder† | 2.92 (0.29) | 3.73 | 3.09-4.50 | 0.71 | 0.31-1.63 | 3.52 | 1.41-8.52 | 2.00 | 0.61-6.36 | 2.72 | 1.02-7.05 | 2.38 | 1.45-3.91 | 2.42 | 1.15-5.04 |
| Heroin use disorder† | 2.26 (0.24) | 2.68 | 2.11-3.40 | 0.84 | 0.36-1.97 | 2.40 | 0.69-8.01 | 7.88 | 0.96-43.01 | 0 | 0.78 | 0.23-2.63 | 2.75 | 1.54-4.88 | |
| Sedative use disorder† | 0.79 (0.14) | 0.90 | 0.57-1.43 | 0.39 | 0.16-0.97 | 0.27 | 0.04-1.72 | 0 | ….…. | 0.39 | 0.05-2.78 | 0.84 | 0.24-2.88 | 0.94 | 0.39-2.21 |
| Inhalant use disorder† | 0.62 (0.10) | 0.60 | 0.42-0.87 | 0.23 | 0.08-0.72 | 0.79 | 0.22-2.77 | 0 | ….…. | 0.61 | 0.14-2.60 | 0.99 | 0.21-4.56 | 1.13 | 0.54-2.37 |
SE: standard error; CI: confidence interval.
In the past year.
In the past month. Boldfaced: The estimate in the given racial/ethnic group differed from the estimate in the given group among whites (P< 0.05).
The sample was 10,795 (148 respondents with missing data on major depressive episode were excluded).
Among adults with CUD, 18.25% met criteria for past-year MDE, 40.92% had current nicotine dependence, 44.07% had past-year alcohol use disorder (AUD), and 19.70% had ≥1 other past-year drug use disorder (opioid 9.67%, cocaine 8.19%, tranquilizer 3.51%, hallucinogen 3.44%, stimulant 2.92%, heroin 2.26%, sedative 0.79%, inhalant 0.62%). Regarding racial/ethnic variation, whites had a higher prevalence of MDE than blacks (20.00% vs. 13.80%), nicotine dependence than Hispanics (44.05% vs. 28.37%), other drug use disorders than blacks (20.83% vs. 14.19%), Asian-American (8.92%), or mixed-race adults (13.99%). In particular, whites had a much higher prevalence of opioid use disorder (11.37%) than blacks (3.77%), Asian-Americans (3.15%), or mixed-race adults (5.99%). Overall, 69% of adults with CUD had another SUD (tobacco, alcohol, drugs), with no racial/ethnic differences.
3.3. Correlates of cannabis dependence vs. cannabis abuse (Table 3)
Table 3.
Adjusted odds ratios (AORs) of cannabis dependence vs. abuse among adults with cannabis use disorder
| Cannabis dependence | Cannabis abuse | Cannabis dependence vs. abuse* (n=10,734†) | ||
|---|---|---|---|---|
|
| ||||
| Row, % | Row, % | AOR | 95%CI | |
| Race/ethnicity | ||||
| White | 65.30 | 34.70 | 1.00 | |
| Black | 67.43 | 32.57 | 1.13 | 0.94-1.35 |
| Native-American | 65.84 | 34.16 | 1.14 | 0.67-1.93 |
| Asian-American | 69.00 | 31.00 | 1.01 | 0.66-1.54 |
| Mixed-race | 70.17 | 29.83 | 1.12 | 0.77-1.64 |
| Hispanic | 64.20 | 35.80 | 0.97 | 0.78-1.22 |
|
| ||||
| Age in years | ||||
| 18-25 | 66.17 | 33.83 | 1.00 | |
| 26–34 | 70.72 | 29.28 | 1.17 | 0.94-1.45 |
| 35–39 | 63.11 | 36.89 | 0.80 | 0.63-1.02 |
| 50+ | 52.57 | 47.43 | 0.47 | 0.29-0.76 |
|
| ||||
| Sex | ||||
| Male | 63.26 | 36.74 | 1.00 | |
| Female | 71.35 | 28.65 | 1.27 | 1.09-1.48 |
|
| ||||
| Marital status | ||||
| Married | 64.32 | 35.68 | 1.00 | |
| Separated/divorced/widowed | 62.87 | 37.13 | 0.94 | 0.63-1.41 |
| Never married/single | 66.40 | 33.60 | 0.96 | 0.72-1.28 |
|
| ||||
| Education | ||||
| Less than high school | 61.66 | 38.34 | 1.00 | |
| High school | 65.33 | 34.67 | 1.14 | 0.96-1.35 |
| Some college | 68.29 | 31.71 | 1.29 | 1.07-1.55 |
| College degree or more | 68.41 | 31.59 | 1.41 | 1.10-1.81 |
|
| ||||
| Total annual family income | ||||
| <$50,000 | 66.51 | 33.49 | 1.00 | |
| $50,000–$74,999 | 66.60 | 33.40 | 0.98 | 0.78-1.24 |
| $75,000+ | 62.77 | 37.23 | 0.80 | 0.68-0.93 |
|
| ||||
| County type | ||||
| Large metropolitan | 67.04 | 32.96 | 1.00 | |
| Small metropolitan | 65.48 | 34.52 | 0.94 | 0.80-1.11 |
| Nonmetropolitan | 59.40 | 40.60 | 0.72 | 0.62-0.84 |
|
| ||||
| Health insurance | ||||
| None | 63.14 | 36.86 | 1.00 | |
| Private | 66.20 | 33.80 | 1.17 | 0.98-1.40 |
| Public | 68.44 | 31.56 | 1.22 | 1.02-1.45 |
|
| ||||
| Major depressive episode, past year | ||||
| No | 63.84 | 36.16 | 1.00 | |
| Yes | 74.16 | 25.84 | 1.62 | 1.33-1.97 |
|
| ||||
| Nicotine dependence, past month | ||||
| No | 66.07 | 33.93 | 1.00 | |
| Yes | 65.23 | 34.77 | 1.02 | 0.88-1.19 |
|
| ||||
| Alcohol use disorder, past year | ||||
| No | 69.06 | 30.94 | 1.00 | |
| Yes | 61.50 | 38.50 | 0.69 | 0.60-0.80 |
|
| ||||
| Any other drug use disorder, past year | ||||
| No | 65.58 | 34.42 | 1.00 | |
| Yes | 66.32 | 33.68 | 1.14 | 0.96-1.36 |
The adjusted logistic regression included all variables listed in the first column and controlled for survey year.
Native Hawaiian/Pacific Islander was excluded due to a small sample size (n=64), and another 145 cases were excluded due to missing values of past-year major depressive episode (n=148, 3 of them were Native Hawaiian/Pacific Islander). CI: confidence interval. Bold-faced: P<0.05.
Two-thirds of adults with CUD had cannabis dependence. We conducted adjusted logistic regression analysis of adults with CUD to identify correlates of cannabis dependence vs. abuse. Due a small sample, native-Hawaiians/Pacific Islanders (n=64) were excluded from the analysis. Race/ethnicity and survey year were unassociated with cannabis dependence. Factors associated with increased odds of cannabis dependence included: ages 18-25 (vs. ages 50+), female sex, ≥college education (vs. <high school), low income (vs. 75,000+), residence in a large metropolitan areas (vs. non-metropolitan areas), public health insurance (vs. no insurance), having MDE, and having no AUD.
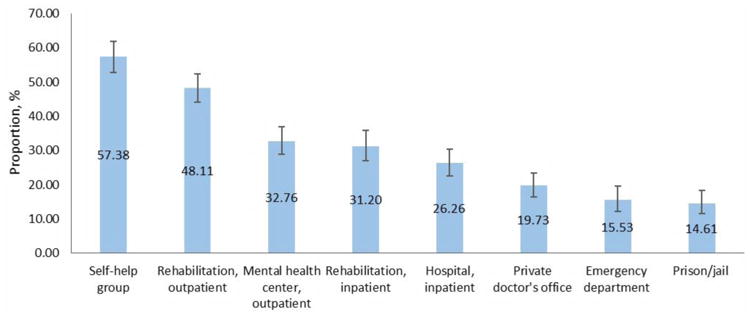
3.4. Prevalence of substance use treatment (Table 4, Fig. 1a-b)
Table 4. Prevalence of alcohol/drug use treatment service use among adults with past-year cannabis use disorder: 2005-2013 NSDUH (n=10,943).
| Race/ethnicity | Total | White | Black | Native-American | Native-Hawaiian/Pacific-Islander | Asian-American | Mixed-Race | Hispanic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Past-year treatment service use, weighted % | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Alcohol/drug use treatment | ||||||||||||||||
| Adults with cannabis abuse (n=3,665) | 13.04 | 11.04-15.34 | 11.78 | 9.70-14.23 | 15.42 | 10.71-21.68 | 16.11 | 9.30-26.46 | 0 | ….…. | 4.69 | 1.77-11.80 | 16.43 | 6.75-34.83 | 15.96 | 10.05-24.40 |
| Adults with cannabis dependence (n=7,278) | 12.87 | 11.62-14.23 | 14.01 | 12.45-15.74 | 10.41 | 8.10-13.27 | 16.85 | 10.44-26.06 | 11.49 | 4.14-28.04 | 8.46 | 2.35-26.19 | 8.37 | 5.17-13.27 | 12.40 | 9.26-16.41 |
| Adults with cannabis abuse/dependence (n=10,943) | 12.93 | 11.89-14.04 | 13.24 | 12.02-14.57 | 12.03 | 9.99-14.42 | 16.59 | 11.30-23.70 | 8.03 | 2.84-20.70 | 7.26 | 2.60-18.67 | 10.76 | 6.81-16.59 | 13.68 | 10.67-17.38 |
|
| ||||||||||||||||
| Drug use treatment | ||||||||||||||||
| Adults with cannabis abuse (n=3,665) | 9.93 | 8.26-11.89 | 8.78 | 7.17-10.71 | 11.20 | 7.33-16.75 | 14.85 | 8.15-25.54 | 0 | ….…. | 3.80 | 1.21-11.34 | 16.17 | 6.54-34.71 | 12.90 | 7.43-21.48 |
| Adults with cannabis dependence (n=7,278) | 10.46 | 9.35-11.68 | 11.36 | 9.92-12.98 | 8.52 | 6.45-11.17 | 12.17 | 6.39-21.96 | 8.34 | 2.25-26.43 | 6.64 | 1.35-26.90 | 7.50 | 4.45-12.35 | 10.18 | 7.40-13.84 |
| Adults with cannabis abuse/dependence (n=10,943) | 10.28 | 9.38-11.24 | 10.47 | 9.40-11.65 | 9.39 | 7.63-11.49 | 13.12 | 8.21-20.30 | 5.83 | 1.54-19.69 | 5.74 | 1.62-18.37 | 10.06 | 6.20-15.93 | 11.16 | 8.27-14.89 |
|
| ||||||||||||||||
| Cannabis use treatment | ||||||||||||||||
| Adults with cannabis abuse (n=3,665) | 7.09 | 5.64-8.88 | 5.71 | 4.30-7.55 | 7.69 | 4.45-12.95 | 14.00 | 7.60-24.35 | 0 | ….…. | 1.97 | 0.46-7.98 | 16.03 | 6.46-34.54 | 11.16 | 5.93-20.02 |
| Adults with cannabis dependence (n=7,278) | 8.18 | 7.19-9.29 | 8.83 | 7.53-10.33 | 7.66 | 5.55-10.48 | 9.49 | 4.49-18.96 | 3.27 | 0.72-13.64 | 0.74 | 0.13-3.99 | 6.03 | 3.26-10.90 | 7.51 | 5.15-10.82 |
| Adults with cannabis abuse/dependence (n=10,943) | 7.81 | 6.97-8.74 | 7.76 | 6.69-8.98 | 7.67 | 5.93-9.87 | 11.08 | 6.71-17.75 | 2.29 | 0.50-9.84 | 1.13 | 0.38-3.27 | 9.00 | 5.22-15.08 | 8.82 | 6.21-12.39 |
CI: confidence interval. Boldfaced: The estimate in the given racial/ethnic group differed from the estimate in the given group among whites (P< 0.05).
Figure 1a. Prevalence of alcohol or drug use related treatment service use among adults with past-year cannabis use disorder: 2005-2013 NSDUH (n=10,943).
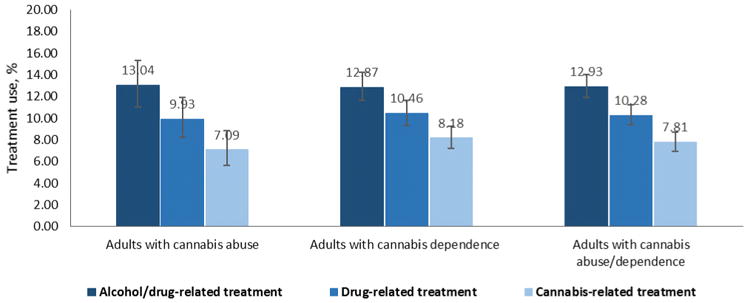
Figure 1b. Treatment settings of past-year alcohol or drug use related treatment service use among adults with cannabis use disorder that received alcohol or drug use treatment services in the past year: 2005-2013 NSDUH (n=1,392).
There was no significant yearly variation in treatment use prevalence for problems related to use of alcohol/drugs, any drug, or cannabis, respectively (Appendix Table S1-S21).
Among adults with CUD (n=10,943), 12.93% received alcohol or drug use treatment, 10.28% used any drug use treatment, 7.81% received cannabis-specific treatment. There were no significant differences in treatment use prevalence by cannabis dependence vs. abuse status. Compared with whites, there was a lower prevalence of cannabis-specific treatment use among Asian-Americans with cannabis dependence (8.83% vs. 0.74%) or any CUD (7.76% vs. 1.13%).
Among adults with CUD that received alcohol or drug use treatment services, common settings were self-help group (57.38%), outpatient rehabilitation (48.11%), outpatient mental health facility (32.76%), inpatient rehabilitation (31.20%), and inpatient hospital (26.26%). Other settings included private doctor's office (19.73%), ED (15.53%) and prison/jail (14.61%). Mixed-race adults (25.04%) and Hispanics (27.85%) had higher proportions of receiving treatment at a private doctor's office than whites (21.49%).
3.5. Adjusted odds ratio of substance use treatment (Table 5)
Table 5. Adjusted odd ratios (AORs) of past-year treatment service use among adults with past-year cannabis use disorder: 2005-2013 NSDUH (n=10,734†).
| Treatment type | Alcohol/drug use related treatment service use-past year | Drug use related treatment service use-past year | Cannabis use related treatment service use-past year | |||
|---|---|---|---|---|---|---|
|
| ||||||
| AOR | 95%CI | AOR | 95%CI | AOR | 95%CI | |
| PREDISPOSING VARIABLES | ||||||
|
| ||||||
| Race/ethnicity (vs. white) | ||||||
| Black | 0.79 | 0.61-1.03 | 0.79 | 0.60-1.05 | 0.83 | 0.61-1.14 |
| Native-American | 0.75 | 0.43-1.33 | 0.74 | 0.39-1.41 | 0.83 | 0.43-1.61 |
| Asian-American | 0.80 | 0.28-2.23 | 0.84 | 0.23-3.04 | 0.21 | 0.06-0.68 |
| Mixed-race | 0.83 | 0.47-1.46 | 1.04 | 0.56-1.92 | 1.32 | 0.66-2.66 |
| Hispanic | 0.86 | 0.65-1.14 | 0.92 | 0.66-1.27 | 0.96 | 0.67-1.39 |
|
| ||||||
| Age in years (vs. 18-25) | ||||||
| 26–34 | 1.08 | 0.81-1.43 | 1.24 | 0.90-1.70 | 1.24 | 0.81-1.90 |
| 35–49 | 1.37 | 0.98-1.91 | 1.59 | 1.11-2.30 | 1.69 | 1.10-2.61 |
| 50+ | 1.05 | 0.58-1.89 | 1.05 | 0.51-2.18 | 0.76 | 0.32-1.79 |
|
| ||||||
| Sex (female vs. male) | 0.75 | 0.62-0.91 | 0.83 | 0.66-1.04 | 0.76 | 0.60-0.97 |
|
| ||||||
| Marital status (vs. married) | ||||||
| Separated/divorced/widowed | 1.87 | 1.13-3.09 | 2.05 | 1.12-3.75 | 2.3 | 1 1.15-4.63 |
| Never married/single | 1.48 | 0.97-2.27 | 1.90 | 1.15-3.12 | 2.34 | 1.25-4.40 |
|
| ||||||
| ENABLING VARIABLES | ||||||
|
| ||||||
| Education (vs. less than high school) | ||||||
| High school | 0.84 | 0.67-1.05 | 0.83 | 0.64-1.07 | 0.80 | 0.61-1.06 |
| Some college | 0.75 | 0.57-0.98 | 0.72 | 0.53-0.98 | 0.67 | 0.48-0.92 |
| College degree or more | 0.51 | 0.32-0.83 | 0.43 | 0.24-0.77 | 0.41 | 0.20-0.86 |
|
| ||||||
| Total annual family income (vs. <$50,000) | ||||||
| $50,000–$74,999 | 0.99 | 0.73-1.34 | 1.05 | 0.75-1.46 | 0.85 | 0.60-1.21 |
| $75,000+ | 1.12 | 0.86-1.46 | 1.29 | 0.95-1.76 | 1.20 | 0.83-1.72 |
|
| ||||||
| County type (vs. large metropolitan) | ||||||
| Small metropolitan | 0.96 | 0.78-1.18 | 0.98 | 0.77-1.24 | 0.98 | 0.74-1.30 |
| Nonmetropolitan | 1.11 | 0.83-1.48 | 1.16 | 0.87-1.56 | 1.10 | 0.76-1.58 |
|
| ||||||
| Health insurance (vs. none) | ||||||
| Private | 0.81 | 0.63-1.06 | 0.77 | 0.58-1.02 | 0.76 | 0.55-1.05 |
| Public | 2.06 | 1.56-2.71 | 1.85 | 1.38-2.48 | 1.76 | 1.33-2.32 |
|
| ||||||
| NEED VARIABLES | ||||||
|
| ||||||
| Major depressive episode (yes vs. no) | 1.69 | 1.30-2.19 | 1.80 | 1.35-2.40 | 1.74 | 1.29-2.34 |
| Nicotine dependence (yes vs. no) | 1.47 | 1.21-1.79 | 1.46 | 1.18-1.79 | 1.33 | 1.06-1.67 |
| Alcohol use disorder (yes vs. no) | 1.61 | 1.33-1.96 | 1.28 | 1.03-1.59 | 1.25 | 0.97-1.61 |
| Any other drug use disorder (yes vs. no) | 3.56 | 2.88-4.40 | 3.92 | 3.16-4.87 | 3.25 | 2.56-4.14 |
Each adjusted logistic regression included all variables listed in the first column and controlled for survey year.
Native Hawaiian/Pacific Islander was excluded due to a small sample size (n=64), and another 145 cases were excluded due to missing values of past-year major depressive episode (n=148, 3 of them were Native Hawaiian/Pacific Islander).
Bold-faced: P<0.05.
We conducted adjusted logistic regression of correlates of treatment received for problems related to use of alcohol/drugs, any drug, and cannabis, respectively, among adults with CUD. Native-Hawaiians/Pacific Islanders with CUD (n=64) were excluded from the analysis.
There was no yearly variation in treatment use prevalence. Asian-Americans had lower odds of using cannabis-specific treatment than whites. Adults aged 35-49 had higher odds than adults aged 18-25 of receiving drug use treatment and cannabis-specific treatment. Women had lower odds than men, and college-educated adults (vs. <high school) had lower odds of receiving treatment for alcohol/drug, drug, or cannabis use. Married adults had lower odds of receiving treatment for alcohol/drug (vs. separated/divorced/widowed adults), any drug, or cannabis use (vs. separated/divorced/widowed adults, single adults). Having public insurance (vs. no insurance), MDE, nicotine dependence, or other drug use disorder were associated with increased odds of receiving treatment for alcohol/drug, any drug, or cannabis use. Having AUD was positively associated with using treatment for alcohol/drug or any drug use.
4. Discussion
The NSDUH constitutes the primary source of CUD data in the United States and includes the largest national sample of adults with CUD to inform treatment needs. The population-level estimates of cannabis-specific treatment use have implications for research and intervention. The majority of the 10,943 adults with CUD were men, had not attended college, had low family income (<$50,000), or resided in large metropolitan areas. Two-thirds of adults with CUD met criteria for cannabis dependence, which was comparatively more common among young adults (18-25), women, low-income or publicly insured adults, and adults with college education. Past-year MDE and other SUD were common among adults with CUD. Overall, 87.07% of adults with CUD had not received alcohol/drug use treatment in the past year; only 7.8% used cannabis-specific treatment. Asian-Americans, women, married adults, and adults with college education in particular underutilized cannabis-specific treatment. Efforts aimed at improving detection, interventions, or treatment for CUD in general medical settings will be needed to mitigate unmet treatment needs for all population groups, such as women, and more-educated or privately insured adults (Shapiro et al., 2013).
There was no significant yearly change in the treatment use prevalence over 9 years. The low prevalence of cannabis-specific treatment use (7.81%) was consistent with the result from the 2012-2013 National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III), which found 7.16% of adults with CUD utilizing cannabis-specific treatment services in the past year (Hasin et al., 2016). The NESARC-III (n=36,309) identified just 972 adults with past-year CUD, which limited the analysis of correlates of treatment use and its comparison with this study. Consistent with other findings, we found that need (severity) indicators (e.g., other SUD and MDE) increased the odds of treatment use (Wu et al., 1999, 2003). Perhaps because of a low prevalence of treatment use, our data suggested no significant differences in treatment use by the CUD status (dependence vs. abuse), and the presence of a comorbid SUD had a small impact on seeking-treatment for drug use. Factors contributing to a low treatment use prevalence may include a low level of cannabis users' perceived need for drug use treatment, stigma, financial concerns, or a lack of routine drug use screening and intervention in general medical settings (Hedden and Gfroerer, 2012; Tai et al., 2011). The absence of a significant increase in treatment use prevalence over the 9-year period reinforces the need for identifying effective strategies to reduce barriers to treatment for CUD and other SUD.
All major non-white racial/ethnic groups examined in this study are growing at a much faster rate than non-Hispanic whites; by 2044, over one-half of Americans will be members of minority groups (Colby and Ortman, 2015). Blacks, native-Americans, and mixed-race adults were found to be more likely than whites to have cannabis dependence in the past year (Wu et al., 2016). The growing population size of nonwhites suggests a rising treatment need for CUD. The large sample of adults with CUD in the NSDUH allowed exploring racial/ethnic differences in treatment use, which could inform screening and intervention efforts for CUD in medical settings. With the exception of Asian-Americans, we found that CUD (abuse or dependence) disproportionally affected low-income or less-educated adults, especially racial/ethnic groups. The lack of significant differences in treatment use between whites and other racial/ethnic groups (other than Asian-Americans) might be related to the finding that having public health insurance increased alcohol/drug and cannabis-specific treatment use. In the United States, the majority of funding for substance use treatment comes from public sources (Mark et al., 2011). Given the predominance of low-income adults with CUD, the expansion of insurance coverage for lower-income individuals (e.g., expansion of Medicaid) and the development of infrastructures to deliver substance use screening, intervention, and treatment will be critically important for improving access to SUD treatment.
Among adults with CUD, Asian-Americans had the highest proportion of college education (77.44%) and the lowest proportion of lacking health insurance; however, only 1% of them received cannabis-specific treatment. Two-thirds of Asian-Americans with CUD had another SUD, suggesting that Asian-Americans experienced extensive barriers to SUD treatment (e.g., culture-related stigma, lack of culturally congruent providers) (Wu and Blazer, 2015). Additionally, few groups of adults with CUD, including women and college-educated adults, showed slightly elevated odds of having cannabis dependence (vs. abuse) but low odds of receiving cannabis-specific treatment. Due to the limitation of cross-sectional data, prospective data will be required to clarify whether such low odds of substance use treatment utilization account partly for cannabis dependence. Married adults with CUD had lower odds of receiving drug/cannabis use treatment. The TEDS data showed a similar pattern in demographics for cannabis-involved treatment admissions: of them, 82% had ≤12 years of education, and only 3.2% reported a currently married status (SAMHSA, 2016). The publicly insured adults with CUD had elevated odds of having cannabis dependence (vs. abuse) and using treatment for cannabis and alcohol/drug use problems, suggesting the presence of severe or comorbid SUD problems that influenced treatment use. Given that the majority of cannabis-related treatment admissions occurred through criminal justice sources, cannabis-related legal or medical events may be a key trigger for treatment entry (SAMHSA, 2016), which is in line with the low treatment use by more educated individuals.
The NSDUH data have some limitations. The cross-sectional data preclude any causal interpretation. The results were based on self-reports that might be influenced by reporting or recall bias. Because the NSDUH provides population-level estimates for the non-institutionalized population, the sampling plan does not cover institutionalized or homeless individuals (about 2%), potentially excluding adults with serious drug use problems. Another limitation is a lack of data about the intensity and quality of treatment received, which is a general weakness in all major surveys of SUDs in the United States. The NSDUH assessment for the treatment location/setting does not specify the information for a specific SUD. Despite the use of the largest national sample available, the sample size of native-Hawaiians/Pacific-Islanders was too small to be a racial/ethnic group in adjusted analysis.
Nonetheless, the NSDUH provides an unparalleled overview of the nation's substance use treatment prevalence for adults with CUD, which is much needed given progressively escalating concerns regarding cannabis potency and CUD (Compton and Baler, 2016). The survey uses the same standardized assessments of CUD and treatment service questions during the 9-year period to track national trends. It includes the largest sample available for exploring racial/ethnic differences in cannabis-specific treatment use and applies statistical computation and analysis weights to minimize nonresponse bias. The survey's response rate is impressive given the size of the sample (SAMHSA, 2014).
In conclusion, over 90% of adults with CUD did not receive cannabis-specific treatment services in the past year. Of them, women, college-educated or married adults, and Asian-Americans especially underutilized cannabis or other substance use treatment. Having private insurance was not associated with treatment utilization. As the CUD prevalence may increase (Hasin et al., 2015), so does its treatment demand. CUD is infrequently addressed by primary care providers (SAMHSA, 2016). Primary care is an entry for healthcare. There is a need to improve screening, brief intervention and referral to treatment efforts to integrate management of CUD and other SUDs into primary care settings (Babor et al., 2017). Research is needed to elucidate the quality of treatment received and outcomes for CUD. Clinical trials for CUD should target women, married adults, and more-educated adults to enhance the representation of the cannabis-using population.
Supplementary Material
Highlights.
Many (69%) adults with cannabis use disorder (CUD) had another substance use disorder.
About 88% of adults with CUD had not received alcohol/drug use treatment services.
Only about 8% adults with CUD used cannabis-specific treatment in the past year.
Asian-Americans, women, and married or college-educated adults underused treatment.
Acknowledgments
The Substance Abuse and Mental Health Data Archive provided the public-use data files for the National Survey on Drug Use and Health, which was sponsored by the Center for Behavioral Health Statistics and Quality of the Substance Abuse and Mental Health Services Administration.
Role of the funding source: This work was made possible by research support from the U.S. National Institutes of Health (R01MD007658, R01DA019623, R01DA019901, UG1DA040317; PI, Li-Tzy Wu). The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:….
Author Disclosures Contributors: LT Wu designed research questions and wrote the drafts of the paper. H Zhu conducted data analyses under the supervision of LT Wu, and all authors contributed to critical revisions and interpretations of the findings to result in the final manuscript.
Conflicts of interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. fourth. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Babor TF, Del Boca F, Bray JW. Screening, brief intervention and referral to treatment: Implications of SAMHSA's SBIRT initiative for substance abuse policy and practice. Addiction. 2017;112:110–117. doi: 10.1111/add.13675. [DOI] [PubMed] [Google Scholar]
- Blanco C, Hasin DS, Wall MM, Flórez-Salamanca L, Hoertel N, Wang S, Kerridge BT, Olfson M. Cannabis use and risk of psychiatric disorders: Prospective evidence from a US national longitudinal study. JAMA Psychiatry. 2016;73:388–395. doi: 10.1001/jamapsychiatry.2015.3229. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (CBHSQ) 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2016a. [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2016b. [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu YWL. The effects of medical marijuana laws on illegal marijuana use. J Health Econ. 2014;38:43–61. doi: 10.1016/j.jhealeco.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Colby SL, Ortman JM. Current Population Reports. U.S. Census Bureau; Washington, DC: 2015. [accessed 02.10.2016]. Projections of the Size and Composition of the U.S. Population: 2014 to 2060; pp. 25–1143. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. [Google Scholar]
- Compton WM, Baler R. The epidemiology of DSM-5 cannabis use disorders among US adults: science to inform clinicians working in a shifting social landscape. Am J Psychiatry. 2016;173:551–553. doi: 10.1176/appi.ajp.2016.16030314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland J, Pokorski I. Progress toward pharmacotherapies for cannabis-use disorder: An evidence-based review. Subst Abuse Rehabil. 2016;7:41–53. doi: 10.2147/SAR.S89857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colorado Department of Public Safety (CDPS) Marijuana Legalization in Colorado: Early Findings. [assessed 20.06.16];A Report Pursuant to Senate Bill. 2016 :13–283. https://assets.documentcloud.org/documents/2829054/2016-SB13-283-Rpt-Colorado-Early-Findings-in.pdf.
- Drug Enforcement Administration (DEA), U.S. Department Of Justic. 2016 National Drug Threat Assessment Summary. 2016 Accessed on February 2, 2017: https://www.dea.gov/resource-enter/2016%20NDTA%20Summary.pdf.
- Fleury MJ, Ngui AN, Bamvita JM, Grenier G, Caron J. Predictors of healthcare service utilization for mental health reasons. Int J Environ Res Public Health. 2014;11:10559–10586. doi: 10.3390/ijerph111010559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman TP, Swift W. Cannabis potency: The need for global monitoring. Addiction. 2016;111:376–377. doi: 10.1111/add.13207. [DOI] [PubMed] [Google Scholar]
- Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45:3181–3189. doi: 10.1017/S0033291715001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;201572:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, Grant BF. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173:588–599. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hedden SL, Gfroerer JC. Correlates of perceiving a need for treatment among adults with substance use disorder: Results from a national survey. Addict Behav. 2011;36:1213–1222. doi: 10.1016/j.addbeh.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Jouanjus E, Lapeyre-Mestre M, Micallef J French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: Signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638. doi: 10.1161/JAHA.113.000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: Results from the National Comorbidity Survey Replication (NCS-R) Psychol Med. 2010;40:225–237. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA. Marijuana tourism and emergency department visits in Colorado. New Engl J Med. 2016;374:797–798. doi: 10.1056/NEJMc1515009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C, Freisthler B, Ponicki WR, Gaidus A. The impacts of marijuana dispensary density and neighborhood ecology on marijuana abuse and dependence. Drug Alcohol Depend. 2015;154:111–116. doi: 10.1016/j.drugalcdep.2015.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes in US spending on mental health and substance abuse treatment, 1986-2005, and implications for policy. Health Aff (Millwood) 2011;30:284–292. doi: 10.1377/hlthaff.2010.0765. [DOI] [PubMed] [Google Scholar]
- Monte AA, Zane RD, Heard KJ. The implications of marijuana legalization in Colorado. JAMA. 2015;313:241–242. doi: 10.1001/jama.2014.17057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of National Drug Control Policy (ONDCP) National Drug Control Strategy Data Supplement 2015. [accessed 06.03.16];The White House. 2015 https://www.whitehouse.gov//sites/default/files/ondcp/policy-andresearch/2015_data_supplement_final.pdf.
- Shapiro B, Coffa D, McCance-Katz EF. A primary care approach to substance misuse. Am Fam Physician. 2013;88:113–121. [PubMed] [Google Scholar]
- Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: A multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Substance Abuse and Mental Health Services Administration; Rockville, MD: 2006. [accessed 03.02.16]. Results from the 2005 National Survey on Drug Use and Health: National Findings. NSDUH Series H-30, DHHS Publication No. SMA 06-4194. http://www.dpft.org/resources/NSDUHresults2005.pdf. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [accessed 03.02.16]. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Episode Data Set (TEDS): 2004-2014 National Admissions to Substance Abuse Treatment Services. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2016; Rockville, MD: 2016. BHSIS Series S-84, HHS Publication No. (SMA) 16-4986. [Google Scholar]
- Tai B, Wu LT, Clark HW. Electronic health records: essential tools in integrating substance abuse treatment with primary care. Subst Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, Bloomfield MA, Curran HV, Baler R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry. 2016;73:292–297. doi: 10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- Wu LT, Kouzis AC, Leaf PJ. Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. Am J Psychiatry. 1999;156:1230–1236. doi: 10.1176/ajp.156.8.1230. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatr Serv. 2003;54:363–369. doi: 10.1176/appi.ps.54.3.363. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatr Serv. 2007;58:192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann Emerg Med. 2012;60:172–180.e5. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Brady KT, Mannelli P, Killeen TK NIDA AAPI Workgroup. Cannabis use disorders are comparatively prevalent among nonwhite racial/ethnic groups and adolescents: A national study. J Psychiatr Res. 2014;50:26–35. doi: 10.1016/j.jpsychires.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG. Substance use disorders and co-morbidities among Asian Americans and Native Hawaiians/Pacific Islanders. Psychol Med. 2015;45:481–494. doi: 10.1017/S0033291714001330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Zhu H, Swartz MS. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug Alcohol Depend. 2016;165:181–190. doi: 10.1016/j.drugalcdep.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H, Wu LT. Trends and correlates of cannabis-involved emergency department visits: 2004 to 2011. J Addict Med. 2016;10:429–436. doi: 10.1097/ADM.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


