Abstract
Objectives
The present study tested an attribution model of help-giving in family caregivers of persons with schizophrenia as it relates to caregivers’ reported burden. We hypothesized (a) that caregivers’ attributions of their ill relatives’ responsibility for their symptoms would be associated with more negative and less positive affective reactions, (b) that affective reactions would be related to perceptions of administered support, and (c) that support would in turn predict greater burden.
Methods
We examined 60 family caregivers of Mexican origin living in Southern California. Mexican Americans were chosen because of their high degree of contact with their ill relative thereby facilitating the examination of help-giving and burden. Contrary to past studies, caregivers’ attributions and affective stance were assessed independently, the former based on self-report and the latter based on codes drawn from the Camberwell Family Interview. Caregiver burden was assessed at baseline and one year later.
Results
Path analyses showed partial support for the attribution model of help-giving. Specifically, attributions of responsibility negatively predicted caregiver’s warmth, which in turn predicted more administered support. Contrary to hypotheses, attributions were not associated with caregiver criticism, and criticism was positively related to administered support. In addition, caregiver support was not related to burden at either baseline or a year later. Criticism was a significant predictor of burden at follow-up through burden at baseline.
Conclusion
The emotional stance of caregivers predicts burden independent of the help they provide. Caregiver criticism not only predicts negative patient outcomes but can predict negative caregiver outcomes as well.
Keywords: expressed emotion, schizophrenia, caregiving, attributions, family support, criticism, burden
The psychosocial study of families and schizophrenia focuses on two important questions. One concerns the family’s role in the illness course. Of particular interest are the caregivers’ attitudes, behaviors and emotional stance as they relate to their ill relatives’ clinical or social functioning. The study of families’ expressed emotion (EE) has received the most attention and the main finding is that family criticism and emotional overinvolvement (EOI) is associated with an increased risk for their ill relative to relapse (Cechnicki, Beilanska, Hanuszkiewicz, & Daren, 2013; Hooley, 2007). The second question focuses on how the illness affects caregivers, particularly their burden and distress. Researchers have examined the symptoms and behaviors associated with the illness, as well as caregivers’ construal of the illness, as they relate to caregivers’ outcomes such as their subjective and objective burden. The key finding is that negative symptoms are associated with more caregiver burden and distress (Koutra et al., 2016; Mitsonis et al., 2012; Roick, Heider, Toumi, & Angermeyer, 2006). Both lines of research are important as they address complementary facets of caregiving. Furthermore, they both have informed family interventions (see McFarlane, 2016 for a review) that aim to improve communication, problem-solving, and stress and illness management skills (e.g., Girón et al., 2010; McFarlane et al., 1995; Sharif, Shaygan, & Mani, 2012).
Although most studies examine either EE or caregiver burden, there are only a handful of studies that integrate the two family roles in a single study. For example, Breitborde and colleagues (2013) brought the caregiver burden focus to a study of expressed emotion. Specifically, in a longitudinal design, they found that for Mexican American families, emotional overinvolvement was related to more family burden, and, in turn, worse health outcomes for caregivers over a one-year period. Thus, EOI is not only a predictor of worse clinical outcomes (e.g., Aguilera, López, Breitborde, Kopelowicz & Zarate, 2010) but it also is a predictor of worse caregiver health outcomes.
Provencher and Mueser (1997) did the opposite and brought aspects of the expressed emotion framework (i.e., caregivers’ attributions of their ill relatives’ responsibility for their symptoms) to the study of caregiver burden. In a cross-sectional study, their main finding was that caregivers who judged their ill relatives’ negative symptoms as outside their relatives’ responsibility reported more objective burden. The authors hypothesize that this is due to caregivers placing ill relatives in the sick-role and taking on extra family and household responsibilities. Other studies have documented the relation between expressed emotion and caregiver burden (e.g., Scazufca & Kuipers, 1996). Relatives identified as high in expressed emotion or criticism report more burden than those relatives identified as low in expressed emotion or criticism (e.g., Carrà, Cazzulo, & Clerici, 2012, Möller-Leimkühler & Jandl, 2011, Raune, Kuipers, & Bebbington, 2004).
Each of these studies takes steps to integrate the study of family attitudes, beliefs and emotional reactions with the study of caregiver burden. Doing so provides an opportunity to depict a more complete understanding of family processes and schizophrenia. What is missing in these studies, however, is a direct measure of what the caregiver does that contributes to greater burden. It could be that the help offered by the caregiver (e.g., attending medical and psychiatric appointments, and assisting with activities of daily living) contributes to the greater burden. Another possibility is that the negative emotional stance of caregivers is what contributes to their burden, not necessarily the help they offer their ill relatives. Such knowledge could inform psychoeducation interventions for caregivers.
Attribution theory offers a useful theoretical framework to study help-giving. Based on the work of Weiner and colleagues in hypothetical scenarios unrelated to caring for ill relatives with schizophrenia, persons who make greater attributions of responsibility tend to report more negative affect (anger) and less positive affect (sympathy), which in turn is related to helping (Weiner, 1993; Weiner, Perry, & Magnusson, 1988). More negative affect is associated with less helping and more positive affect is associated with more helping. In the context of caring for a relative with a serious mental illness, we would expect that greater helping would be associated with greater caregiver burden.
Past research that has examined caregivers’ attributions has primarily attempted to understand how expressed emotion relates to the clinical course not caregiver’s help (see Hooley, 1985 for the first consideration of attributions). Previous studies have found that more attributions of control are related to criticism (e.g., Weisman, Nuechterlein, Goldstein, & Snyder, 1998) and warmth (López et al., 2004), and the affective reactions, in turn, are related to more or less relapse (López, Nelson, Snyder, & Mintz, 1999). We know of only one study that examined the association between caregiver attributions, affect and help-giving and they found limited support for the model (Weisman, Gomes & Lopez, 2003). Extending attribution theory to help-giving and caregiver burden has the potential to integrate the study of the two family models. It may be that caregivers’ expressed emotion and help-giving may share similar conceptual processes, specifically cognitive appraisal (attributions) and emotional reactions. (See Kuipers, Onwumere and Bebbington, 2010 for a related model).
One limitation of much of the family attribution research to date is that both attributions and emotions have been obtained from the same source—the Camberwell Family Interview (Vaughn & Leff, 1976). Independent raters listen to the audiotaped semi-structured interview of the caregivers and code either attributions (e.g., Brewin, MacCarthy, Duda, and Vaughn, 1991) or emotional responses (e.g., criticism or warmth). The findings of associations between attributions and expressed emotion may be at least in part due to similar method variance. A more rigorous test of the linkage between attributions and emotional responses would require two independent observations.
The study of Mexican American families has helped to identify cross-cultural variability in families’ emotional stance as they express more warmth and less criticism than Euro-Americans (Lopez et al., 2009). Moreover, criticism has proven not to be predictive of future relapse (Aguilera et al., 2010; Kopelowicz et al., 2002; Lopez et al., 2004) whereas in one of only a few studies, family warmth was related to less relapse (Lopez et al., 2004). This was not the case for Euro-Americans. The prominence of warmth in Mexican American families provides a favorable sociocultural context to examine the role of help-giving and its relationship to caregiver burden.
Study Overview and Hypotheses
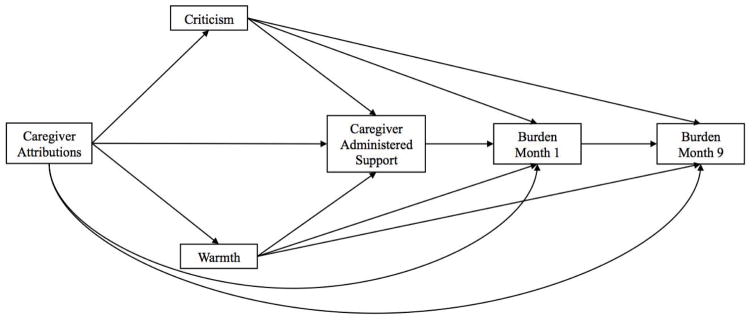
The overall objective of this study therefore is to test an attributional model of helping and burden among Mexican origin caregivers of persons with schizophrenia. We first hypothesized that caregivers’ greater attributions of responsibility for their relatives’ symptoms would be associated with more negative affect (criticism), and less positive affect (warmth). Second, we expected affect would be associated with caregiver support such that negative affect would be related to less support and positive affect would be related to more support. Third, we examined the interrelations of attributions, affect, and helping behavior with the burden of caregivers. We hypothesized that administered support provided by caregivers (as predicted by attributions of responsibility and affect) would predict greater burden at baseline and one year later. To address previous methodological limitations we used independent measures of attributions, affect, and help giving. The hypothesized model is given in Figure 1.
Figure 1.
Hypothesized attribution model.
Method
Participants
Sixty Mexican-American patients with schizophrenia or schizoaffective disorder and 60 caregivers participated in the study. All participants were recruited from two outpatient mental health centers in the greater Los Angeles, area. Both clinics are publicly funded community mental health centers and about 50% are of Latino origin of whom most are of Mexican descent. To qualify for the study, all patients and caregivers had to be of Mexican descent, over 18 years of age, show no evidence of organic impairment or mental retardation, provide informed consent, agree to participate in the study, and respond coherently to the questioning. In addition, patient participants had to be less than 65 years of age, and have a diagnosis of schizophrenia or schizoaffective disorder based on the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (First, Spitzer, Gibbon, & Williams, 2002).
Table 1 presents caregiver and patient demographic characteristics. Patients ranged in age from 19 to 60 (M = 39.4; SD = 11.2) and had an average of 10.4 years of education (SD = 3.5). Patients were primarily male (n = 40; 66.7%) and single (n = 37; 61.7%). Caregivers included 39 parents, 9 partners, 8 siblings and 4 children; the majority of which were mothers (55.0%; n = 33). Caregivers ranged in age from 22 to 88 (M = 55.1; SD = 16.8) and had completed about 8 years of education (SD = 4.4). Caregivers were primarily female (n = 49; 81.7%) and married (n = 32; 58.2%). In terms of preferred language, patients were primarily English-speakers (n = 38; 63.3%) whereas caregivers were primarily Spanish-speakers (n = 38; 63.3%). Caregivers had to either live with or have at least weekly contact with the patient participants. In fact, caregivers reported spending on average 42 hours (SD = 29.8) with their ill relatives during the week prior to the interview.
Table 1.
Descriptive Characteristics of Patients and Caregivers
| Patients (n = 60) | Caregivers (n = 60) | |
|---|---|---|
| Age, in years | 39.42 (SD = 11.15) | 55.12 (SD = 16.76) |
| Gender | ||
| Female | 20 (33.3%) | 49 (81.7%) |
| Male | 40 (66.7%) | 11 (18.3%) |
| Caregiver relationship to patient | ||
| Parent | 39 (65.0%) | |
| Partner | 9 (15.0%) | |
| Sibling | 8 (13.4%) | |
| Child | 4 (6.7%) | |
| Primary language | ||
| English | 38 (63.3%) | 22 (36.7%) |
| Spanish | 22 (36.7%) | 38 (63.3%) |
| Place of birth | ||
| Mexico | 27 (45.0%) | 26 (70.3%) |
| United States | 33 (55.0%) | 11 (29.7%) |
| Education, in years | 10.38 (SD = 3.54) | 7.96 (SD = 4.42) |
| Marital status | ||
| Married | 11 (18.3%) | 32 (58.2%) |
| Single | 37 (61.7%) | 5 (9.1%) |
| Other | 12 (19.9%) | 18 (32.6%) |
Note. The demographic data reflect the full sample except for the following caregiver characteristics: age (n = 59); place of birth (n = 37); education (n = 56); and marital status (n = 55).
Procedure
Mental health professionals at the two clinics identified potential participants among their patients with a diagnosis of DSM-IV schizophrenia or schizoaffective disorder. Clinic staff gave identified patients and their caregivers recruitment flyers in their preferred language and a research team member subsequently provided an overview of the study to patients who agreed to be contacted. After informed consent from both the patients and the caregivers was obtained, a research team member conducted interviews and administered study measures in a face-to-face meeting. In total, the research team contacted 178 patients and their caregivers. A total of 118 participants were excluded from the study due to participation refusal, failure to meet study criteria, and inability of both the patient and the key relative to be reached by the research team. Of the 60 patient-caregiver dyads interviewed at time 1, 39 (65%) dyads were interviewed approximately one year later. Twenty-one dyads did not complete interviews at time 2 because they could not be located or declined further participation. Analyses comparing dyads that dropped out of the study to those who completed study measures showed no significant differences in baseline measures of attributions of responsibility, expressed emotion, or support.
Measures
Each measure was administered in the preferred language of the participant (English or Spanish). In addition, research staff members read each measure aloud to participants to ensure that participants understood the questions and that their responses were recorded accurately on questionnaires.
Attributions
The Key Relative’s Attributions of Symptoms Scale (Harrison & Dadds, 1992), modified and used by Niv, López, Glynn and Mueser (2007), assesses the perceptions of behavioral responsibility that caregivers hold concerning their relatives’ illness. The measure consists of 28 items, each of which is a symptom that the key relative rates on a scale of responsibility. Examples of the symptoms of this measure include: slow in completing tasks, poor concentration, and angry/hostile behavior. Caregivers were asked to only rate items if patients exhibited the symptom within the past month. For attributions of responsibility, caregivers were presented with the following question: “How much is he or she at fault for this behavior?” They were asked to rate their responses on a 0 (not at all at fault) to 5 (completely at fault) Likert scale. Each key relative received an averaged total score for attributions of responsibility. Cronbach’s alpha for this scale in this study was .95.
Affect
Key relative’s emotional reactions toward their ill relative were assessed using the Camberwell Family Interview (CFI; Vaughn & Leff, 1976), a one to two hour semi-structured interview. During the interview, caregivers talked about a variety of topics, including the onset of the disease and the disease’s impact on family life during the past three months. All interviews were audiotaped and later scored on warmth (positive affect) and criticism (negative affect). Warmth is a global measures rated on a 6-point scale (0 = no warmth, 5 = high warmth). Coders made a global rating of warmth based on the key relative’s positive tone of voice, spontaneous expression of positive regard, and expression of sympathy, concern, understanding, and interest in the ill relative. Criticism was measured by the number of critical comments made about the ill relative, which ranged from 0 to 12 in our sample. A critical comment expresses dislike, or disapproval regarding the ill relative’s behavior or personality in content or tone of voice. Seven coders rated the CFI interviews. Intraclass correlation coefficients of each coder’s ratings revealed adequate to excellent reliability for the EE indices: warmth (.73 – .94) and criticism (.73 – .97).
Administered Support
Caregivers completed a measure of administered support. The questionnaire consisted of 6 items influenced by items from the Arizona Social Support Interview Schedule (ASSIS; Barrera, 1981) that measure different domains of support: emotional, tangible, informational, appraisal, instrumental, and social companionship. Caregivers were asked to rate whether they provided each of these types of support to their ill relative during the past month on a scale from 1 (not at all) to 5 (always). A mean score of administered support was obtained for each key relative. The internal consistency of this scale for this study was .78.
Burden
Key relative’s reported burden was measured at time 1 and time 2 (approximately 10 months after baseline) using the Burden Assessment Scale (BAS; Reinhard, Gubman, Horwitz, & Minsky, 1994). This 19-item scale assesses the amount of burden perceived by the caregiver as a result of providing care to the patient. The scale is divided into two subscales, objective burden (α = .91) and subjective burden (α = .78). Objective burden measures the extent to which caregivers experience negative behavioral effects of caretaking, such as financial problems, limitations of personal activity, disruptions of the household, and lack of social interactions. Subjective burden assesses the negative feelings, attitudes, and emotions that result from the caregiving experience. Respondents indicated how much they agreed with statements on a 4-point scale (1 = not at all; 4 = a lot). Items from the objective burden subscale included “Had financial problems” and “Had less time to spend with friends.” Items from the subjective burden subscale include “Feel trapped by your caregiver role” and “Found the stigma of the illness upsetting.”
Statistical Analyses and Assumptions
A path analysis model was estimated to examine the three primary hypotheses of the model. Prior to model testing, the statistical assumptions underlying the model were tested and descriptive statistics examined. The total sample size was 60, with some missing data, particularly on burden measured at one year. It was reasonable to impute missing data (Schafer & Graham, 2002). Additionally, we tested the homogeneity of the covariance matrices to examine the hypothesis that the missing data was representative of a different underlying population than the present data (Kim & Bentler, 2002). We found evidence that missingness was unrelated to homogeneity of covariance matrices χ2 (N=60, 15) = 5.23, p = .97. Therefore, we imputed the data using ML estimation (Jamshidian & Bentler, 1999). Chi square statistics typically require larger sample sizes than a sample of 60. Therefore the models will be evaluated with Yuan-Bentler residual based F statistic (Bentler & Yuan, 1999).
There were no multivariate or univariate outliers. Using Mardia’s coefficient there was evidence to support the assumption that the data followed a multivariate normal distribution, standardized coefficient = −.11, p > .05. Means, standard deviations and bivariate correlations are given in Table 2.
Table 2.
Descriptive Statistics and Correlations of Attributions of Responsibility, Expressed Emotion, Support, and Burden
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Responsibility | ---- | .19 | −.35** | .01 | .22 | .23 |
| 2. Criticism | ---- | −.36** | .15 | .52*** | .37* | |
| 3. Warmth | ---- | .30* | −.15 | −.15 | ||
| 4. Administered Support | ---- | .11 | .12 | |||
| 5. Burden | ---- | .39** | ||||
| 6. Burden 2 | ---- | |||||
|
| ||||||
| N | 60 | 60 | 60 | 60 | 60 | 39 |
| M | 1.23 | 3.23 | 2.88 | 2.94 | 2.29 | 2.25 |
| SD | 1.34 | 2.93 | 1.28 | 0.95 | 0.69 | 0.71 |
Note. 2 = Time 2.
p < .05,
p < .01,
p < .001.
Results
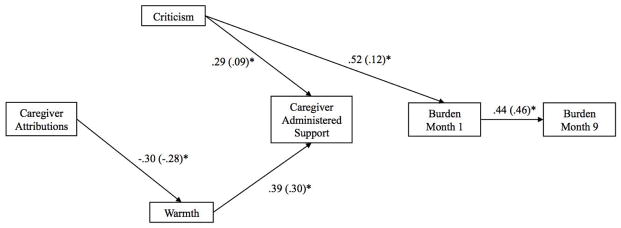
The hypothesized model fit the data well, Yuan-Bentler residual based F(9,51) = .30, p = .97. Although χ2 is not the optimal test statistic given the sample size, it is most typically used to evaluate path analysis models. Therefore, for purposes of reference, the maximum likelihood chi square for the hypothesized model is also presented, χ2(N=60, 1) = .06, p = .81, CFI = .1.00. Prior to interpretation, a trimmed model was estimated with the non-significant paths removed. This model also fit the data, Yuan-Bentler residual based F(9,51) = .30, p = .97. Again, to facilitate understanding the maximum likelihood chi square for the hypothesized model, χ2 is also presented, χ2(N=60, 5) = 8.27, p = .14, CFI = .1.00. The final model with both standardized and unstandardized coefficients is presented in Figure 2.
Figure 2.
Key relative model with and unstandardized (standardized) coefficients. Note residuals were estimated but are not included in diagram for ease of interpretation
We found partial support for the proposed caregiver attribution-affect link. Caregiver attributions significantly predicted less warmth (standardized coefficient = −.30, unstandardized coefficient = −.28, p < .05), however caregiver attributions were not related to criticism. We also found partial support for the hypothesized caregiver affect and help-giving link. Greater positive affect (warmth) predicted more caregiver administered support (standardized coefficient = −.39, unstandardized coefficient = .30, p < .05). Although negative affect (criticism) was also related to administered support, the relationship was in the opposite direction than expected. Greater criticism predicted more administered support (standardized coefficient = .29, unstandardized coefficient = .09, p < .05).
In testing the full attribution-affect-helping-burden model we found that criticism also predicted burden at month 1 (standardized coefficient = .52, unstandardized coefficient = .12, p < .05). In addition, total burden at month 1 predicted total burden at month 12 (standardized coefficient = .44, unstandardized coefficient = .46, p < .05). Finally, we observed that although criticism did not predict burden at month 12, it did indirectly predict burden at 12 months through burden at month 1 serving as an intervening variable (standardized indirect effect coefficient =.23, unstandardized indirect effect coefficient = .06, p < .05). We also tested models of subjective and objective burden separately to test for differential effects and we found the same magnitude and significance of coefficients. The bivariate correlation between subjective and objective support is high (r = .63, p < .001). Therefore given the similar pattern of results and the high correlation, models were estimated using total burden.
Discussion
The findings point out the central role that a critical emotional stance plays in family members’ caregiving and burden. Contrary to attribution theory, criticism is associated with more not less help-giving. Moreover caregivers’ criticism is related to more caregiver burden at baseline and at follow-up one year later. What is particularly striking is the significant role criticism played in a sample of Mexican origin families for whom criticism is not particularly salient (Lopez et al., 2009) and has not been related to relapse in previous reports with this sample (Aguilera et al., 2010) and two other samples of Mexican origin (Kopelowicz et al., 2002; Lopez et al., 2004).
The finding that a critical family stance is associated with more help-giving suggests that family members are engaged and motivated to help their ill relatives. Criticism marks an expectation that better functioning is possible, and given its association with help-giving, it also reflects a willingness to lend a hand to foster behavioral gains. One might even consider the possibility that criticism and help-giving together reflect a caring posture on the part of the caregiver. Hooley (2007) in fact wrote that “the impression one gets from conversations with high-EE relatives is that the vast majority of them are highly motivated to help the patient” (p. 341).
It is curious that both criticism and warmth predicted more help-giving. The findings regarding warmth are consistent with attribution theory as lower attributions of responsibility were associated with more warmth and more help-giving. It is unclear what underlies the critical stance as attributions were found not to be related to criticism. It may have been some aspect of their ill relative’s social or clinical functioning, something that caregivers thought could be changed. Whatever the case, the findings indicate that caregiver help-giving appears to be motivated by both positive (warmth) and negative (criticism) affect.
Although we were able to identify the affective basis to help-giving, it turns out that help-giving was not at all associated with caregiver burden. What the caregivers report doing to help their ill family member is not related to their degree of burden. Caregiver criticism again proved to be the significant predictor of burden. More criticism was associated with greater burden at baseline that then served as the intervening variable between more criticism and greater burden one year later. Our findings are consistent with past studies that demonstrated the high EE or criticism link with caregiver burden (e.g., Möller-Leimkühler and Jandl, 2011). Additionally, the fact that help-giving was not related to burden suggests that burden is not a function of the amount of help offered by caregivers but instead is a function of the caregiver’s negative emotional stance. This may be consistent with previous findings that caregivers’ internalized stigma (i.e., shame and low self-efficacy) also contributes to greater burden (Hasson-Ohayona, Levy, Kravetz, Vollanski-Narkis, & Roe, 2011).
We were surprised with the prominent role criticism played in caregivers’ help-giving and burden given that in previous studies of Mexican Americans’ clinical outcomes criticism has played a modest role. It is important to keep in mind a number of factors in interpreting these results. First, the average level of criticism (M = 3.23, SD = 2.93) is well below the threshold of 6 critical comments for designating high EE and is lower than other studies (e.g., M = 7.59, SD = 5.13 for a Euro-American sample; Snyder et al., 1984). The lower and more restricted range of criticism within this sample is compatible with the interpretation of an engaged but not overly critical caregiver sample. Second, although criticism has been shown to be related to burden in a prior study of schizophrenia and depression (Möller-Leimkühler & Jandl, 2011), the possibility that criticism may deviate from expectations that the caregivers have of themselves in their caregiver role may contribute to the subjective burden that they may experience. Finally, it is worth noting that in a previous caregiving study of the same sample (Breitborde et al., 2009), emotional overinvolvement proved to be associated with poorer physical and mental health of the caregivers over time. Although emotional overinvolvement and warmth have played prominent roles in past reports of Mexican American families, findings from the current study and Aguilera et al. (2010) caution against overlooking the role criticism can play in family processes of Mexican Americans caring for persons with schizophrenia.
Strengths and Limitations
One strength of the current study is that the key relative’s affective stance was based on a coder’s rating of the Camberwell Family Interview and help-giving and burden were based on caregivers’ self report. It is not likely that the observed relationships can be explained by shared method variance. A second strength of the study is that burden was assessed at baseline and one-year later. This prospective design rules out the possibility that burden at follow-up leads to the observed family processes at baseline. The main limitation of the study is the attrition of subjects at follow-up from 60 to 39, which is greater than previous prospective studies on family processes and schizophrenia (e.g., Rosenfarb, Triana, Nuechterlein, Ventura, and Breitborde, 2016). An additional limitation is that participants in the study were initially identified by clinic staff potentially introducing biases in our sample’s characteristics.
Implications and Conclusion
A critical emotional stance of caregivers is the most significant family predictor of poor outcomes of persons with schizophrenia. Our findings indicate that family criticism is a significant predictor of caregiver outcomes as well, particularly their level of burden. It is important that family interventions address families’ critical emotional stance not only because of its relation to poor clinical outcomes, but also because of its relation to poor caregiver outcomes. Integrating a balanced rationale for family interventions—to improve ill relatives’ and caregivers’ outcomes—may serve to enhance existing family interventions. It may promote further engagement of both parties as some caregivers may be additionally motivated to improve their own well-being, and some ill relatives may appreciate more equitably distributing the treatment focus.
Practitioner Points.
Positive Clinical Implications
In family treatment it is important to address caregiver criticism not only because of its relationship to poor clinical outcomes of ill relatives but also because of its relationship to greater caregiver burden.
Integrating a balanced rationale for family interventions—to improve ill relatives’ and caregivers’ outcomes—may promote further engagement of both parties as some caregivers may be additionally motivated to improve their own well-being, and some ill relatives may appreciate more equitably distributing the treatment focus.
Limitations
The caregiver sample was in general low in criticism thereby the findings may not be generalizable to families with a higher degree of criticism.
There was a 35% sample attrition at the one year follow-up.
Acknowledgments
The research was supported by the National Institute of Mental Health (MH01499) and the National Institute of Minority Health and Health Disparities (MD003405).
Contributor Information
Bianca T. Villalobos, University of Arkansas
Jodie Ullman, California State University, San Bernardino.
Tracy Wang Krick, Johns Hopkins University.
Darcy Alcántara, University of Massachusetts, Boston.
Alex Kopelowicz, University of California, Los Angeles.
Steven R. López, University of Southern California
References
- Aguilera A, López SR, Breitborde NJK, Kopelowicz A, Zarate R. Expressed emotion and sociocultural moderation in the course of schizophrenia. Journal of Abnormal Psychology. 2010;119(4):875–885. doi: 10.1037/a0020908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera M., Jr . Social support in the adjustment of pregnant adolescents. In: Gottlieb BH, editor. Social networks and social support. Beverly Hills, CA: Sage; 1981. pp. 69–96. [Google Scholar]
- Bentler PM, Yuan KH. Structural equation modeling with small samples: Test statistics. Multivariate Behavioral Research. 1999;34(2):181–197. doi: 10.1207/S15327906Mb340203. [DOI] [PubMed] [Google Scholar]
- Breitborde NJ, López SR, Aguilera A, Kopelowicz A. Perceptions of Efficacy, Expressed Emotion, and the Course of Schizophrenia: The Case of Emotional Overinvolvement. Journal of Nervous and Mental Disease. 2013;201(10):833. doi: 10.1097/NMD.0b013e3182a5bf1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitborde NJ, López SR, Chang C, Kopelowicz A, Zarate R. Emotional over-involvement can be deleterious for caregivers’ health. Social Psychiatry and Psychiatric Epidemiology. 2009;44:716–723. doi: 10.1007/s00127-008-0492-0. [DOI] [PubMed] [Google Scholar]
- Brewin CR, MacCarthy B, Duda K, Vaughn CE. Attributions and expressed emotion in the relatives of patients with schizophrenia. Journal of Abnormal Psychology. 1991;100:546–554. doi: 10.1037/0021-843X.100.4.546. [DOI] [PubMed] [Google Scholar]
- Carrà G, Cazzullo CL, Clerici M. The association between expressed emotion, illness severity and subjective burden of care in relatives of patients with schizophrenia. Findings from an Italian population. BMC Psychiatry. 2012;12:140. doi: 10.1186/1471-244X-12-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cechnicki A, Bielańska A, Hanuszkiewicz I, Daren A. The predictive validity of expressed emotions (EE) in schizophrenia. A 20-year prospective study. Journal of Psychiatric Research. 2013;47(2):208–214. doi: 10.1016/j.jpsychires.2012.10.004. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Harrison CA, Dadds MR. Attributions of symptomatology: An exploration of family factors associated with expressed emotion. Australian and New Zealand Journal of Psychiatry. 1992;26(3):408–416. doi: 10.3109/00048679209072063. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion: A review of the critical literature. Clinical Psychology Review. 1985;5(2):119–139. doi: 10.1016/0272-7358(85)90018-2. [DOI] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Jamshidian M, Bentler PM. ML estimation of mean and covariance structures with missing data using complete data routines. Journal of Educational and Behavioral Statistics. 1999;24(1):21–24. doi: 10.3102/10769986024001021. [DOI] [Google Scholar]
- Kim KH, Bentler PM. Tests of homogeneity of means and covariance matrices for multivariate incomplete data. Psychometrika. 2002;67(4):609–623. doi: 10.1007/BF02295134. [DOI] [Google Scholar]
- Kopelowicz A, Zarate R, Gonzalez V, Lopez SR, Ortega P, Obregon N, Mintz J. Evaluation of expressed emotion in schizophrenia: A comparison of Caucasians and Mexican Americans. Schizophrenia Research. 2002;55:179–186. doi: 10.1016/S0920-9964(01)00193-1. [DOI] [PubMed] [Google Scholar]
- Koutra K, Triliva S, Roumeliotaki T, Basta M, Lionis C, Vgontzas AN. Family functioning in first-episode and chronic psychosis: The role of patient’s symptom severity and psychosocial functioning. Community Mental Health Journal. 2016;52(6):710–723. doi: 10.1007/s10597-015-9916-y. [DOI] [PubMed] [Google Scholar]
- Kuipers E. Family interventions in schizophrenia: Evidence for efficacy and proposed mechanisms of change. Journal of Family Therapy. 2006;28(1):73–80. doi: 10.1111/j.1467-6427.2006.00338.x. [DOI] [Google Scholar]
- Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis. British Journal of Psychiatry. 2010;196:259–265. doi: 10.1192/bjp.bp.109.070466. [DOI] [PubMed] [Google Scholar]
- López SR, Garcia Ramirez JI, Ullman JB, Kopelowicz A, Jenkins J, Breitborde NJK, Placencia P. Cultural variability in manifestation of expressed emotion. Family Process. 2009;48:179–194. doi: 10.1111/j.1545-5300.2009.01276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López SR, Hipke KN, Polo AJ, Jenkins JH, Karno M, Vaughn C, Snyder KS. Ethnicity, expressed emotion, attributions, and course of schizophrenia: Family warmth matters. Journal of Abnormal Psychology. 2004;113(3):428–439. doi: 10.1037/0021-843X.113.3.428. [DOI] [PubMed] [Google Scholar]
- López SR, Nelson KA, Snyder KS, Mintz J. Attributions and affective reactions of family members and course of schizophrenia. Journal of Abnormal Psychology. 1999;108(2):307–314. doi: 10.1037/0021-843X.108.2.307. [DOI] [PubMed] [Google Scholar]
- McFarlane WR. Family interventions for schizophrenia and the psychoses: A review. Family Process. 2016;55(3):460–482. doi: 10.1111/famp.12235. [DOI] [PubMed] [Google Scholar]
- McFarlane WR, Lukens E, Link B, Dushay R, Deakins SA, Newmark M, … Toran J. Multiple-family groups and psychoeducation in the treatment of schizophrenia. Archives of General Psychiatry. 1995;52(8):679–687. doi: 10.1001/archpsyc.1995.03950200069016. [DOI] [PubMed] [Google Scholar]
- Mitsonis C, Voussoura E, Dimopoulos N, Psarra V, Kararizou E, Latzouraki E, … Katsanou MN. Factors associated with caregiver psychological distress in chronic schizophrenia. Social Psychiatry and Psychiatric Epidemiology. 2012;47(2):331–337. doi: 10.1007/s00127-010-0325-9. [DOI] [PubMed] [Google Scholar]
- Möller-Leimkühler AM, Jandl M. Expressed and perceived emotion over time: does the patients’ view matter for the caregivers’ burden? European Archives of Psychiatry and Clinical Neuroscience. 2011;261(5):349–355. doi: 10.1007/s00406-010-0178-y. [DOI] [PubMed] [Google Scholar]
- Niv N, López SR, Glynn SM, Mueser KT. The role of substance use in families’ attributions and affective reactions to their relative with severe mental illness. Journal of Nervous and Mental Disease. 2007;195(4):307–314. doi: 10.1097/01.nmd.0000243793.64279.48. [DOI] [PubMed] [Google Scholar]
- Onwumere J, Kuipers E, Bebbington P, Dunn G, Freeman D, Fowler D, Garety P. Patient perceptions of caregiver criticism in psychosis: Links with patient and caregiver functioning. Journal of Nervous and Mental Disease. 2009;197(2):85–91. doi: 10.1097/NMD.0b013e3181960e57. [DOI] [PubMed] [Google Scholar]
- Parabiaghi A, Lasalvia A, Bonetto C, Cristofalo D, Marrella G, Tansella M, Ruggeri M. Predictors of changes in caregiving burden in people with schizophrenia: A 3-year follow-up study in a community mental health service. Acta Psychiatrica Scandinavica. 2007;116(s437):66–76. doi: 10.1111/j.1600-0447.2007.01094.x. [DOI] [PubMed] [Google Scholar]
- Provencher HL, Mueser KT. Positive and negative symptom behaviors and caregiver burden in the relatives of persons with schizophrenia. Schizophrenic Research. 1997;26(1):71–80. doi: 10.1016/S0920-9964(97)00043-1. [DOI] [PubMed] [Google Scholar]
- Raune D, Kuipers E, Bebbington PE. Expressed emotion at first-episode psychosis: investigating a carer appraisal model. British Journal of Psychiatry. 2004;184(4):321–326. doi: 10.1192/bjp.184.4.321. [DOI] [PubMed] [Google Scholar]
- Reinhard SC, Gubman GD, Horwitz AV, Minsky S. Burden Assessment Scale for families of the seriously mentally ill. Evaluation and Program Planning. 1994;17(3):261–269. doi: 10.1016/0149-7189(94)90004-3. [DOI] [Google Scholar]
- Roick C, Heider D, Toumi M, Angermeyer MC. The impact of caregivers’ characteristics, patients’ conditions and regional differences on family burden in schizophrenia: a longitudinal analysis. Acta Psychiatrica Scandinavica. 2006;114(5):363–374. doi: 10.1111/j.1600-0447.2006.00797.x. [DOI] [PubMed] [Google Scholar]
- Rosenfarb IF, Triana S, Nuechterlein KH, Ventura J, Breitborde NJ. Expressed emotion and the escalation of depressive symptoms in individuals with recent-onset schizophrenia. Early Intervention in Psychiatry. 2016 doi: 10.1111/eip.12307. [DOI] [PubMed] [Google Scholar]
- Scazufca M, Kuipers E. Links between expressed emotion and burden of care in relatives of patients with schizophrenia. British Journal of Psychiatry. 1996;168(5):580–587. doi: 10.1192/bjp.168.5.580. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Sharif F, Shaygan M, Mani A. Effect of a psycho-educational intervention for family members on caregiver burdens and psychiatric symptoms in patients with schizophrenia in Shiraz, Iran. BMC Psychiatry. 2012;12(1):1. doi: 10.1186/1471-244X-12-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn C, Leff J. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology. 1976;15(2):157–165. doi: 10.1111/j.2044-8260.1976.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Weiner B. On sin and sickness. A theory of perceived responsibility and social motivation. American Psychologist. 1993;48(9):957–965. doi: 10.1037/0003-066X.48.9.957. [DOI] [PubMed] [Google Scholar]
- Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1988;55(5):738–748. doi: 10.1037/0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- Weisman AG, Nuechterlein KH, Goldstein MJ, Snyder KS. Expressed emotion, attributions, and schizophrenia symptom dimensions. Journal of Abnormal Psychology. 1998;107(2):355–359. doi: 10.1037/0021-843X.107.2.355. [DOI] [PubMed] [Google Scholar]
- Weisman AG, Gomes LG, Lopez SR. Shifting blame away from ill relatives: Latino families’ reaction to schizophrenia. Journal of Nervous and Mental Disease. 2003;191(19):574–581. doi: 10.1097/01.nmd.0000087183.90174.a8. [DOI] [PubMed] [Google Scholar]