Fig. 2.
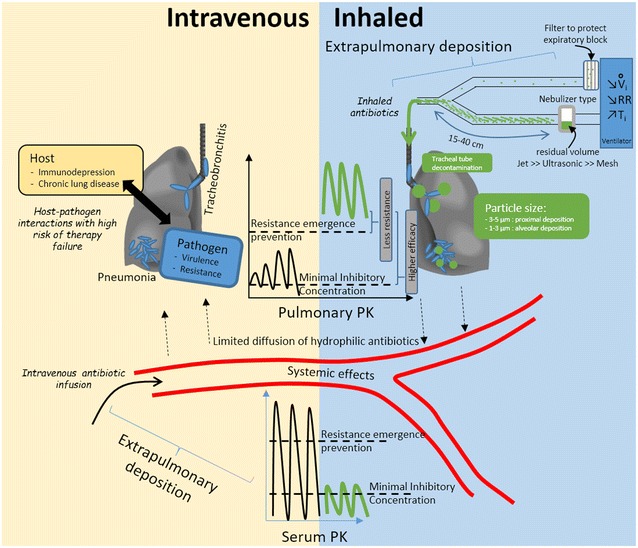
Differences between intravenous and nebulized antibiotic therapy. Intravenous infusion (yellow panel, left bottom corner) leads to high extrapulmonary concentrations and potential toxicities. Diffusion to the lung is limited and resulting concentrations that may not exceed minimal inhibitory concentration can lead to treatment failure in challenging host–pathogen combinations. Nebulized delivery (blue panel, right top corner), implementing an optimized technique (detailed in Table 3) results in higher pulmonary concentrations that are above the resistance emergence prevention threshold, thus reducing the likelihood of resistant strain selection. These concentrations are well above the minimal inhibitory concentration, thus resulting in improved efficacy of concentration-dependent antibiotics, even with difficult-to-treat pathogens; systemic side effects may be reduced. Nebulization requires carful implementation so as to avoid potential respiratory side effects. PK pharmacokinetics, V i inspiratory flow, RR respiratory rate, T i inspiratory time
