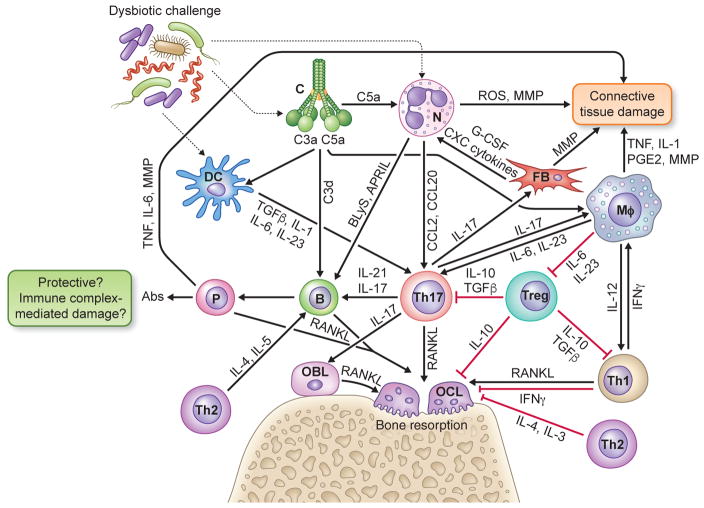
Fig. 1. Innate-adaptive immune interplay leading to inflammatory tissue damage and bone loss in periodontitis.
Periodontitis arises from complex interactions between the host and the subgingival dysbiotic microbiota that lead to excessive or dysregulated inflammatory responses involving elements of both innate (complement, phagocytes) and adaptive immunity (regulatory and effector lymphocytes). Shown is a simplified view of cytokine- and chemokine-mediated cross-talk interactions between innate and adaptive immune cells leading to destruction of connective tissue and bone in periodontitis. See text with figure-1 callouts for details. Abbreviations in the figure: Abs, antibodies; APRIL, a proliferation-inducing ligand; B, B cell; BLyS, B lymphocyte stimulator; C, complement; DC, dendritic cell; FB, fibroblast; G-CSF, granulocyte-colony stimulating factor; Mφ, macrophage; MMP, matrix metalloproteinases; IL, interleukin; IFN, interferon; N, neutrophil; OBL, osteoblast; OCL, osteoclast, P, plasma cell; RANKL, receptor activator of nuclear factor-κB ligand; ROS, reactive oxygen species; TGFβ, transforming growth factor-β; TNF, tumor necrosis factor; Treg, T regulatory cell; Th-1,-2,-17, T helper type -1,-2, -17 cells.