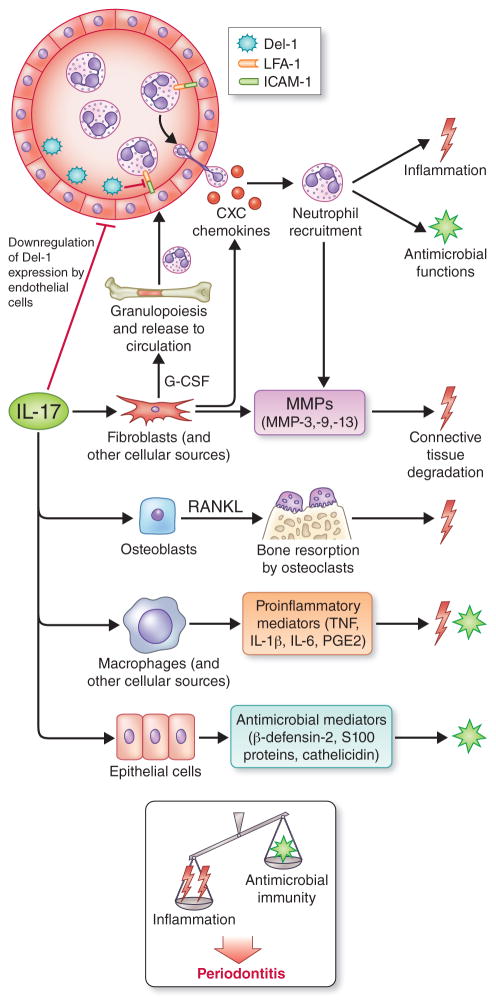
Fig. 3. Biological functions of interleukin-17 and their potential impact on periodontitis.
Interleukin-17 acts predominantly on innate immune and stromal cells (e.g., fibroblasts, endothelial and epithelial cells) to promote innate immunity, especially neutrophil-mediated antimicrobial and inflammatory responses. In this regard, interleukin-17 promotes granulopoiesis and neutrophil recruitment by up-regulating granulocyte-colony stimulating factor and CXC chemokines and by down-regulating developmental endothelial locus-1, an endogenous inhibitor of neutrophil adhesion and extravasation. Interleukin-17 can moreover induce the production of epithelial cell-derived antimicrobial molecules. On the other hand, interleukin-17 can contribute to the destruction of both connective tissue and the underlying bone by stimulating the production of matrix metalloproteinases and RANKL from the indicated stromal cell types. Interleukin-17 is thus an immunological double-edged sword with both protective and destructive functions. As indicated, the current burden of evidence from human and animal model studies suggests that the net effect of interleukin-17 signaling promotes periodontal disease development. Abbreviations in the figure: developmental endothelial locus-1; developmental endothelial locus-1; G-CSF, granulocyte-colony stimulating factor; MMPs; matrix metalloproteinases; RANKL, receptor activator of nuclear factor-κB ligand. From Zenobia and Hajishengallis [ref. (298)]; used by permission.