Abstract.
Strategies to improve the quality of hospital care are needed if ongoing gains in child health and survival are to be made. We previously reported on improvements in the quality of case management in hospitals following a guideline-based intervention in Lao PDR, with variation in the degree of change achieved between clinical conditions. This study aims to understand the factors that influenced the uptake of the guideline-based intervention, and its impact on care. This qualitative study was embedded in a mixed-methods evaluation of guideline implementation in nine hospitals in Lao PDR. Focus groups and individual interviews were conducted with 70 health staff from central, provincial, and district hospitals. The interview guide was based on the Theoretical Domains Framework. Inductive content analysis was performed on interview transcripts to identify themes, supported by field notes from the intervention. Findings were triangulated against previously reported quantitative outcomes using driver diagrams. Key influences on guidelines uptake related to the guideline and intervention (filling a void, physical accessibility, comprehensibility, training in guideline use), health staff (behavior regulation, trust in guidelines, and beliefs about consequences), and the environment (social influences particularly consensus and incorporation into clinical norms). The major barrier was family preference for treatments in conflict with guideline recommendations. This study identifies contextual factors that explain, as well as validate previously identified improvements in care following guideline implementation in Lao PDR. It provides novel understanding of why the same intervention may have a differential impact on different clinical conditions.
INTRODUCTION
Strategies to improve the quality of hospital care are needed if ongoing gains in child health are to be made in line with the sustainable development goals.1–4 The World Health Organization (WHO) Pocketbook of Hospital Care for Children (Pocketbook) is one potential strategy.5 It contains evidence-based guidelines for the hospital management of children and is accompanied by materials for training health workers in its use. Although significant resources have been invested in the development of the guidelines, their implementation has not been systematic and the impact on quality of care is not well understood.6,7
At the heart of interventions to improve care is the need to change clinical behavior and extensive literature, from developed and developing countries, attests that this is difficult. Interventions, such as guidelines, often have modest and variable impact on clinical practices.8–13 Variation in impact is likely to be explained by local contextual factors that influence the success or failure of any one intervention.14,15 Therefore, it is essential to understand not only if an intervention improves care, but also why.16
The Pocketbook was implemented in hospitals in Lao PDR between 2010 and 2011 using a multifaceted intervention delivered through collaboration with Lao pediatricians, the WHO, and the Ministry of Health. The intervention included distribution of written guidelines, interactive workshops using case-based training materials, engagement of local opinion leaders, consensus building, and audit and feedback on clinical practice. Implementation efforts were delivered in a context that lacked a culture of guideline use and reading more broadly.17 The Pocketbook represented the first comprehensive, Lao-language pediatric text. Translation was therefore an important part of this process and required initial translation of individual chapters by senior Lao pediatricians, followed by collaborative review of the translation to gain consensus on both the technical content and translated document.
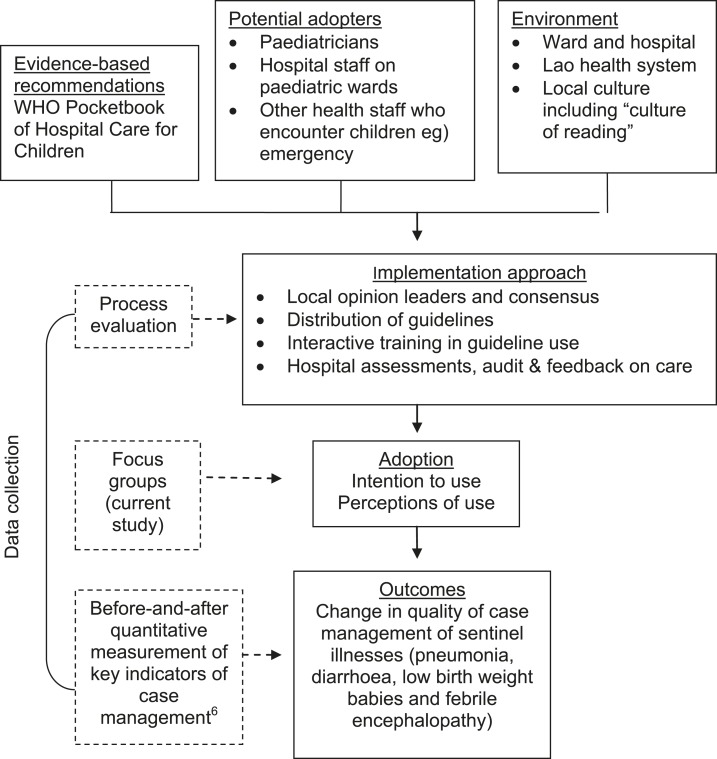
The qualitative work described in this paper was embedded in a mixed-methods evaluation of the Pocketbook implementation and its impact on hospital care for children in Lao PDR. (Figure 1) Previously reported quantitative findings from the evaluation demonstrated improvements in the quality of case management of sentinel illnesses, including treatment of conditions by severity and increased rational drug and fluid prescribing. There was, however, variation in the degree of change for different diseases—large change seen for pneumonia, and moderate change for diarrhea.7 In this qualitative study, we aimed to identify contextual factors that influenced uptake of clinical guidelines and their impact on practice.
Figure 1.
Framework for a mixed-methods evaluation of the implementation of the World Health Organization Pocketbook of Hospital Care for Children in Lao hospitals, based on the Ottawa Framework of Research Use.16
MATERIALS AND METHODS
Framework.
The Ottawa Model of Research Use provided the overall framework for the mixed-methods evaluation of the guideline implementation in Lao PDR and was used to plan the different levels of data collection (Figure 1).18,19 This qualitative study aimed to understand perceptions of “potential adopters” of the intervention, their intention to adopt guidelines, and factors influencing this intent. For this work, we used the Theoretical Domains Framework (TDF).20,21
Subjects.
A qualitative study using focus group discussions and individual interviews was conducted at nine hospitals approximately 6 months after guideline workshops, including three central, three provincial, and three district hospitals. Seventy participants were interviewed including 22 pediatricians, 14 pediatric residents, nine doctors, 22 nurses, and three medical assistants.
Data collection and analysis.
In central hospitals, more than 95% of doctors in relevant wards had received training in guideline use and focus group participants were purposively selected from this cohort. Five focus groups were conducted, one for staff from each hospital and two for pediatric residents. In provincial and district hospitals, one focus group was conducted in each of the six hospitals. Both trained and untrained staff participated in focus groups at the hospitals’ request. Only 2–3 staff had been trained in each provincial and district hospital at the time of the study, including doctors, nurses, and medical assistants. This was due to the cascade approach used in training and limitations to expanding training coverage. Nonetheless, we felt it was important to include these hospitals at this time to determine if the intervention was appropriate at lower levels of care before committing to broader implementation. Key stakeholders in the implementation of the guidelines or those with leadership roles in the study hospitals were interviewed individually to facilitate availability, provide confidentiality, and ensure their presence did not influence focus group discussions.
The TDF domains and suggested questions for exploring them were used to develop a semistructured interview guide20 (Table 1). Focus groups were conducted in English and Lao language. In central hospitals, questions were asked in English then translated into Lao by a senior member of the focus group. Participants responded in Lao or English, both of which could be understood by the interviewer (Amy Gray), who had worked in Lao PDR for 2 years conducting this research, providing technical support to guideline implementation and supporting clinical care more broadly. Alternative translators for central hospitals with both adequate medical knowledge and English skills were senior Lao clinicians, usually in leadership positions in hospitals. Their presence in the discussions may have limited the freedom of participants to express their views. Consequently, the interview process successfully relied on the combined language skills of the interviewer and interviewees. When misunderstanding occurred, discussion of responses actually led to a better understanding of underlying perspectives. In provincial and district hospitals, an independent translator, who was not a clinician, was used to support the interview process, given the lower level on English skills in these settings. The same translator was used for each focus group and they relied on the primary researcher for medical content knowledge. Discussions were audio-taped and transcribed in their original Lao and English text then translated into complete English transcripts. All English transcription was performed by the primary researcher (Amy Gray). The Lao components of the interviews were transcribed in Lao then translated into English by a senior Lao pediatrician (Bandith Soumphonphakdy).
Table 1.
Example of domains explored, questions asked and prompts used in the interview guide
| Domain | Question | Prompts |
|---|---|---|
| Current practice, knowledge, and skills | Are you currently using the WHO Pocketbook in your day-to-day practice? | If yes, can you describe how you use them? |
| When do you use them? (e.g., every patient, only for complicated patients, only for drug information) | ||
| What else do you use? | ||
| Professional role and identity | What do you think about the book? | |
| Do you have confidence in the guidelines in the WHO Pocketbook? Why/why not? | For whom do you think the Pocketbook is important? | |
| Do you think it is important to use the guidelines in practice? | Why/why not? | |
| Beliefs about consequences and capabilities | How difficult/easy is it to use the book in practice? | Is there anything that would help you use it better? |
| Can you describe any changes after the Pocketbook was introduced? | For themselves, patients, quality of care, cost of care? | |
| Please give an example of something which has changed. | ||
| Has anything improved? | ||
| Social Norms | Do you see other people using the Pocketbook? | Please give an example |
| Do other people encourage you to use the book? | Government, hospital leaders, colleagues, patients | |
| Is it expected that you use the guidelines on the ward? | ||
| External control beliefs (including environmental constraints) | Do other factors in the hospital prevent you from using the guidelines? | For example |
| Do other factors in the hospitals stop you from giving better care to patients? | Time | |
| What factors have been important for introducing the Pocketbook into Lao hospitals? Why? | Equipment and supplies | |
| Cost of treatment | ||
| Other staff | ||
| Conflict with other guidelines | ||
| Check each intervention component | ||
| Translation? | ||
| Hospital assessments? | ||
| Feedback on assessments? | ||
| Training? | ||
| Leadership? | ||
| Other? |
Inductive content analysis of focus group and interview data was performed manually. Codes were drawn from the data and individual codes were grouped into overarching themes by the primary researcher (Amy Gray). Themes that correlated with a TDF domain were relabeled accordingly. The coding structure was reviewed by two reviewers in an iterative process. The first reviewer reviewed the coding with the primary researcher, reviewing where codes had been drawn from data, discussing themes, interrogating the primary researcher for exceptions to reported themes and potential biases. Codes and themes were revised and the process repeated with the second reviewer. Themes that emerged were mapped against the Ottawa Framework of Research Use in terms of factors relating to the intervention, the health-care providers, and the environment.18 Complete transcripts were then recoded using the final set of agreed themes and codes. Data saturation was reached after focus groups in central hospitals, one provincial and one district hospital. Data from focus groups were complemented by field notes and observations made throughout 2 years of implementation activities for the guidelines in Lao PDR.
We used driver diagrams to triangulate our findings with our previously reported quantitative outcomes.7 Driver diagrams are a quality improvement tool used to visualize how barriers and facilitators of improving care interact within a health system.22 They have been proposed as a potential tool for considering why or how an intervention works, and to highlight variation in contextual factors between sites of implementation.23 In this instance, we used them for understanding the differential impact of our intervention on diseases.
Ethical statement.
Ethics approval for the research was obtained from the Lao National Ethical Committee for Health Research, in Vientiane Lao PDR and from the Human Research Ethics Committee at the University of Melbourne. Written consent was obtained from the director of each participating hospital before conducting hospital assessments. Focus group participants signed individual consent forms.
RESULTS
Themes were identified in three overarching categories relating to the guidelines themselves, the care providers, and the broader environment.
Guideline and intervention factors.
Filling a void.
All staff described the need for comprehensive Lao language, pediatric hospital guidelines, suitable to their situation and resources, which was filled by the intervention. Although one previous guideline for hospitals existed, its perceived usefulness in everyday practice, content, and relevance to pediatrics was limited. Some drug reference books had previously been used in practice, but no resources that outlined a complete, and systematic approach to case management, from triage to assessment, diagnosis, treatment, and supportive care in a practical way (Table 2).
Table 2.
Guideline and intervention factors influencing uptake and use of pediatric hospital guidelines in Lao PDR
| Theme | Subtheme | Exemplar quotation |
|---|---|---|
| Filling a void | Lack of existing guidelines | “It is my first guideline!”(Pediatrician 5, central hospital 1) |
| “And in Laos, because we lack books for medical students, for the staff, for the medical books for reading, so I think that it is very good.” (Pediatrician 4, central hospital 2) | ||
| “If they [provincial and district hospitals] have the Pocketbook to use it is better to treat patients in the province. [The existing guidelines] are not complete and they are not for children.”(Pediatrician 15, central hospital 3) | ||
| Broad, relevant content | “Ah...so many things there [in the Pocketbook] for children. Everything is already there, only you use that. (Pediatrician 3, central hospital 2) | |
| Accessibility | Physical availability | “You use that [the Pocketbook] for reading and not for that [demonstrates putting the book in shelf] and to read if you have a problem. All of them have it in their pocket.” (Pediatrician 4, central hospital 2) |
| Language and comprehensibility | “Before, many people had this book. But many people do not understand English well, and they may interpret correctly or incorrectly.” (Pediatrician 14, central hospital 1) | |
| “Some medical words are difficult to understand in Lao. Some people understand English then translate to Lao and understand, but in the provincial and district hospitals they don’t understand English, but I am not sure they understand the Lao meaning.” (Pediatric resident 3) | ||
| Simplicity | “If possible, simplify the book...and to start, what to simplify? Many things in there are for us, everything is important so what to keep, what to cut out, to simplify?” (Pediatrician 3, central hospital 2) | |
| Training in use | “[Before training] I had the book but we don’t know how to use...We read page by page. Difficult” (Pediatrician 10, central hospital 1) | |
| “…when we compare physicians who have trained before with people who did not get training, for the people who have trained they understand better, to use, and understand better the contents of the book. But the people who did not receive training they still find difficulties.” (Pediatrician 13, central hospital 2) |
Accessibility.
The accessibility of the guidelines was perceived to be essential in facilitating their uptake. Accessibility related first to the physical availability of the book due to saturation of hospital staff with individual copies of guidelines, and the size of the book allowing it to be carried and available during clinical duties. This was described as a contrast to previous guidelines—often distributed in limited copies and kept in cupboards for safekeeping.
In addition, accessibility related to the comprehensibility of the contents. Guideline translation was described as being fundamental to health staff from all levels of care being able to access and use them appropriately. Separate to the issue of simple translation was the conceptual understanding of the translated text. As a first major pediatric text in Lao language, many of the words included in the guidelines did not have an agreed translation, with a risk to staff misunderstanding both Lao and English terms. Despite some concerns, overall the translation was viewed as comprehensible and appropriate.
The role of simplicity in guideline accessibility was made apparent by focus group discussion participants both describing and re-enacting the relative ease of following pneumonia guidelines compared with diarrhea. The latter required participants to reference different charts on different pages, which is not necessarily intuitive to those who have limited access to guidelines, and books more generally. The desire for simplification contrasted with recognition that the guidelines were already relatively concise, all content was relevant and that training had led to changes in reading practices and improved staff capacity to access guidelines.
Desire for guideline simplicity was driven by perceptions of staff capacity to use guidelines. Participants emphasized the need to understand the practicalities of how guidelines should be used. Although clinical algorithms such as Integrated Management of Childhood Illnesses (IMCI) existed previously in Lao PDR, the concept of a guideline that should be applied “in real time” at the bedside was a new skill to learn. The idea of referencing sections of the book, which were relevant to the clinical case at hand through the use of contents or the index pages, had to be learnt. As a result, participation in the training that focused on how to use guidelines, rather than just their content, was identified as an important factor determining guideline uptake by individuals.
Health provider factors.
Behavior regulation.
Although staff described guideline use as a specific skill which required training, they also reported it was a skill that, beyond training, required ongoing application on the job to achieve a level of competence and efficiency. This clearly required a change of habit, which took time. Staff reported only a few examples of colleagues who were not willing to do so, and they were felt to be largely the exception. (Table 3)
Table 3.
Provider factors influencing uptake and use of pediatric hospital guidelines in Lao PDR
| Theme | Subtheme | Exemplar quotation |
|---|---|---|
| Behavioural regulation | “Usually paediatric doctors do not like to read” (Pediatric resident 1) | |
| “The attitude” (Pediatric resident 2) | ||
| “Some people don’t like to read, they just do in their same old way” (Pediatric resident 1) | ||
| Trust | “[Through the process of] translation into Lao many senior doctors read and have agreement already, what wouldn’t we trust it?” (Pediatric resident 9) | |
| Belief about capabilities | It makes staff and residents more confident...they have the same guidelines as the teachers have...They think they do the right thing for the patient.” (Pediatrician 20, central hospital 1) | |
| This book....is the same as a teacher who sits here with us. If I want to ask the teacher I open the book and look....If I want to check something about a symptom or treatment of a child I go to this book...I am more confident...(District hospital doctor 2) | ||
| Beliefs about consequences | Improved rational prescribing | “… it has changed a lot. Before we did this workshop to give medicines, the method, the patient comes and we give ceftriaxone. But after, we changed the medicine depending on severity and we changed the way we give amoxicillin...” (Pediatrician 12, central hospital 2) |
| Standardisation of care | “…before we did not have a book and some read this [book], and some read that, and there is no agreement...but now we have [information] in the book, we can tell them, use the book…Anywhere, anything is the same...” (Pediatrician 17, central hospital 3) | |
| Completeness of care | “At the beginning of seeing every patient we compare things we do with the information in the book. We must agree in the ways we take care of patients such as triage, drug doses…should be done step-by-step, as the book says.” (Provincial doctor 5) | |
| Attitude to reading | “[The Pocketbook]...encourages nurses, doctors and other people to read more...the people want to read more...because they understand.” (Pediatrician 4, central hospital 2) | |
Trust.
. Consensus around the use of the Pocketbook was facilitated by trust in the guidelines, their evidence base, and the authority that comes with the WHO. Importantly, trust in the guidelines also arose from knowledge of senior Lao pediatrician engagement throughout the implementation process.
Beliefs about capabilities and consequences.
Staff perceived a number of changes following guideline implementation. The most common were improved antibiotic prescribing, including reduced unnecessary prescriptions and weight-based prescribing, and appropriate prescribing of intravenous fluid, with reduced unnecessary fluid use. Overall, they felt patient care had improved. However, apart from practice change related to antibiotics and intravenous fluids, doctors found it difficult to articulate examples. The idea that care was “better” seemed to reflect care completeness and standardisation. The resulting consistency facilitated rational treatment decisions, confidence of staff in decision-making and transfer of patients within the hospital referral system. There was a perceived move away from simple diagnostic labeling and drug prescribing with an increasing awareness of the complete steps in case management, as taught by the training approach.
There was an unanticipated perceived change in the reading culture. Availability of a relevant and accessible, local language resource motivated health workers to read, including those yet to attend the training.
Environmental factors.
Social influences.
Consensus—widespread agreement on the guidelines and their acceptance as standards of care—was described an essential component in the implementation process. A consensus meeting was conducted early in the implementation process to agree on the translation and the implementation approach. Yet “consensus” was not described by participants as a one off event—rather it evolved during the implementation process through involvement of local pediatricians at all steps including translation, evaluation, training, and group discussion forums. Conversely, failure to engage pediatric leadership in this process would have prevented successful implementation. The level of consensus achieved was reflected in expressions of local ownership over the Pocketbook, as “our Pocketbook” (Table 4).
Table 4.
Environmental factors influencing uptake and use of pediatric hospital guidelines in Lao PDR
| Theme | Subtheme | Exemplar quotation |
|---|---|---|
| Social influences | Consensus/group norms | “There is agreement across the whole country already. You can say it comes from WHO it is easy to say.” (Pediatric resident 10) |
| “Because the [workshop] attendees came from everywhere, so they have to agree after the workshop, they have to make a decision how to do [to use the guidelines] and follow.” (Pediatrician 11, central hospital 2) | ||
| Local opinion leaders | “...if it is a good book but they [senior doctors] do not agree, we cannot use it.” (Pediatric resident 6) | |
| So you know, here in our country, when teachers in central hospitals say something, they doctors or medical staff from rural areas, from provincial or district hospitals, they would believe us. So when we use it they would use it too... (Pediatrician 3, central hospital 2) | ||
| Modeling | “I could see the residents too, they encourage each other [to use the book], they ask each other. And I could see residents teaching medical students to use the book too, so medical students can use the book and residents explain to medical students from the book.” (Pediatrician 9, central hospital 1) | |
| Reinforcement | “Yes the book is in their pocket. If the resident does not have it I will…(indicates cutting motion)…their score.” (Pediatrician 5, central hospital 1) | |
| Environmental context and resources | Culture | “You have to respond to the family, to make them happy. Even if the child will die [if you do what the family wants]...you have to ask their opinion.”(Provincial hospital doctor 3) |
| Equipment and supplies | Yes some problems, for example, for very severe pneumonia with cyanosis, we should have oxygen prongs but we don’t have them. It says to give the oxygen by nose but we only have the nasal prongs for adults so we give by mask. We have a problem.” (District hospital nurse 3) | |
Staff provided numerous examples of how the guidelines had become integrated with clinical norms. There was an expectation that guidelines should be carried by all staff and used in everyday practice was modeled by doctors. In central hospitals, doctors described reinforcement of guideline use through the introduction of consequences, such as implications for academic performance, if staff or students were not seen meeting these expectations.
Environmental context and resources.
Expectations and preferences of patients and their families were major external determinants of the ability of doctors to follow guideline recommendations. In particular, they were barriers to certain procedures such as lumbar puncture and naso-gastric tubes, and to optimal timing of discharge—with many patients discharging early.
Equipment and supply availability was not a barrier to uptake in central hospitals and a minor issue at lower levels of care. Essential equipment, drugs, and supplies were felt to be largely accessible, even if organisation or quantity of available equipment could be improved. In district and provincial hospitals, missing essential equipment often reflected staff or family preference or awareness of treatment alternatives—such as intravenous over nasogastric fluids for rehydration, and oxygen masks over cannulas for treatment of hypoxia—rather than a lack of availability of the equipment in-country.
DISCUSSION
Following implementation of the WHO Pocketbook of Hospital Care for Children in Lao PDR, health workers reported a strong intent to use the guidelines in practice, evidence of uptake beyond those who had been trained and perceptions that guidelines had led to better clinical care. Perceptions of change correlate well with the previously reported quantitative findings from the evaluation of guideline implementation which demonstrated improved quality of case management, both overall and in specific areas including rational drug and fluid prescribing.7 This research primarily highlights facilitators of change in contrast to much of the literature, which focuses on barriers.8,20,24–28
A key guideline factor was physical accessibility.29 But more important than this, accessibility relied on appropriate language, content, and upskilling health workers in how to access information needed in real-time clinical practice. Two guideline attributes from this study have not been previously emphasized—the degree to which these guidelines “filled a void” and the importance of understanding complexities in the local language, which have implications for the comprehension of translated guidelines by users. The Lao translation aimed for both technical accuracy and “conceptual equivalence”–a term that refers to how words or phrases are understood in the local context, which may be different from the literal translation.30 This was done through an interactive and collaborative translation process, which has been shown to be valid in Lao than back translation.31 Effectively, this process became part of our intervention, by building consensus and trust.
Relatively novel to the literature is the lack of Lao language texts described by participants, with implications for the existing culture of reading, which was felt to be poor. This context is a clear test of the critical balance between the comprehensibility and accessibility of written clinical guidelines on one hand, and the capacity of the intended users to apply them on the other. The importance of training in guideline use, and not assuming this is an innate skill, cannot be underestimated. Although guidelines had been distributed in central hospitals before training, training was the impetus for change. Change in practice was then further enabled by favourable social influences, including local consensus and modeling of desired behaviours, which integrated the guidelines into clinical practice norms. Integration would have benefitted staff and students who were not specifically trained. In previous studies, the absence of these factors has been identified as a barrier to guideline use.24,27
Guidelines have often been criticized as oversimplifying clinical management. In contrast, in this setting where guidelines, let alone any local language medical texts, were limited there were concerns about the capacity of lower level health workers to understand and apply guidelines. Simplifying guidelines was raised as a potential solution. Of note, central hospital staff suggested simplification. District hospital staff for whom simplification was intended requested further support in developing their skills in applying guidelines in practice.
Participant responses in our research were heavily orientated toward facilitators of guideline uptake, rather than barriers. The barriers described largely reflected those previously described in the literature; views of patients and their families,8,20,26,27 difficulties in changing habits,24,26 time taken using guidelines26 and, to some extent, equipment supplies.14,24,25,27,32
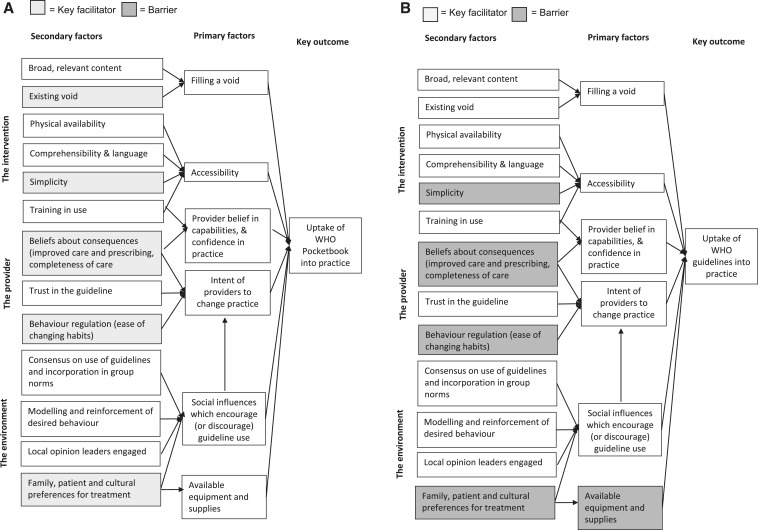
The facilitators and barriers identified in this study are important influences on our intervention overall. Greater value comes from triangulating them with our quantitative findings, which showed greatest improvement in pneumonia case management, with less change in diarrhea and other diseases7 (Figure 2). Changes in pneumonia management were facilitated by an absence of existing agreed hospital guidelines for pneumonia, by the guidelines implemented being simple and algorithmic to follow and compatible with existing provider practice of prescribing antibiotics and patient expectations (Figure 2A). Providers felt rational prescribing for pneumonia led to equivalent patient outcomes to previous. In contrast, for diarrhea, guidelines were difficult to follow for staff not used to referencing written guidelines in real-time patient care (Figure 2B). The guidelines did not “fill” the same need as IMCI guidelines had previously been in use. Furthermore, strong family preferences for intravenous fluids, which mirrored staff preferences, went against guideline recommendations for nasogastric hydration. Resultant infrequent use of nasogastric hydration meant staff capability to use nasogastric tubes, as well as availability of the equipment, had to be overcome also to change practice.
Figure 2.
Driver diagram of key contextual factors identified to be influencing implementation and uptake of the World Health Organization Pocketbook of Hospital Care for Children in Lao hospitals in relation to (A) pneumonia and (B) diarrhea case management.
There are two key limitations of our study. First, pediatric staff in central Lao hospitals are disproportionately represented. We acknowledge different views may be obtained as further implementation experience is gained. Second, the primary researcher had a dual role in both implementation of the intervention and in interviewing participants, who knew them. This is a challenge in low-resource settings where other options may not exist—including sufficient human resources or funding to separate research and implementation roles. In Laos, limited access to individuals with appropriate capacity for interviewing, language competence, and medical knowledge led to different choices of interviewers in central and peripheral hospitals. In a pure research sense this may not be optimal. At a pragmatic level, it led to greater clarity in interview discussions as participants and interviewers sought to clarify understanding of each other.
The dual role of implementer and interviewer may have led participants to avoid criticizing the intervention, and contributed to smaller numbers of barriers being reported. However, the validity of the focus group findings is supported both by quantitative findings and prolonged periods of observation on wards by the interviewer during the study. The insider–outsider perspective is extensively discussed in qualitative research—with an insider having a more nuanced, in-depth understanding of the context and an outsider having more ability to distance themselves from those they study.33 There are advantages in both. The key is for the researcher to practice reflexivity through active reflection on their role and its potential interaction with research findings.34 This was prioritized in this research, particularly in the iterative process of data coding.
The implementation of the WHO pediatric hospital guidelines in Lao PDR was previously demonstrated to have led to improved quality of hospital care for children.7 The current study identifies contextual factors that explain these changes and provides a framework for understanding how one intervention in one setting can have a variable impact on improving care for different clinical conditions. Moving forward, it provides potential targets to close the gap between guideline recommendations and practice. Intervention activities need to be focused on bridging gaps where they exist; between the guidelines on one hand and the capacity of individual health workers to apply them on the other; between the intent of staff to use guidelines, and actual use in practice; and between guideline recommendations and cultural preferences.
Acknowledgmenets:
Trevor Duke, Geoff McColl, and Glenn Bowes of the University of Melbourne are acknowledged for their contribution to the oversight and supervision of the overall mixed-methods study conducted in Lao hospitals. Lynn Gillam is acknowledged for her review of coding and themes identified in the qualitative analysis. The work would not have been possible without the cooperation of the WHO Office in Lao PDR, the directors and staff of the Lao Hospitals and the Ministry of Health Lao PDR.
Disclaimer: Amy Z. Gray, Douangdao Soukaloun and Bandith Soumphonphakdy all have previously worked as consultants for the World Health Organization. All authors were involved in the implementation efforts related to introduction of the WHO Pocketbook of Hospital Care for Children in Lao PDR
REFERENCES
- 1.Campbell H, Duke T, Weber M, English M, Carai S, Tamburlini G, 2008. Global initiatives for improving hospital care for children: state of the art and future prospects. Pediatrics 121: e984–e992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duke T, Kelly J, Weber M, English M, Campbell H, 2006. Hospital care for children in developing countries: clinical guidelines and the need for evidence. J Trop Pediatr 52: 1–2. [DOI] [PubMed] [Google Scholar]
- 3.Duke T, 2006. Global implementation of WHO clinical guidelines to improve child survival: the need for collaboration, resources and action. J Paediatr Child Health 42: 565–567. [DOI] [PubMed] [Google Scholar]
- 4.Akachi Y, Tarp F, Kelley E, Addison T, Kruk ME, 2016. Measuring quality-of-care in the context of sustainable development goals. Bull World Health Organ 94: 160–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO, 2005. WHO Pocketbook of Hospital Care for Children. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 6.Li MY, Kelly J, Subhi R, Were W, Duke T, 2013. Global use of the WHO Pocket Book of Hospital Care for Children. Paediatr Int Child Health 33: 4–17. [DOI] [PubMed] [Google Scholar]
- 7.Gray AZ, Soukaloun D, Soumphonphakdy B, Duke T, 2015. Implementing WHO hospital guidelines improves quality of paediatric care in central hospitals in Lao PDR. Trop Med Int Health 20: 484–492. [DOI] [PubMed] [Google Scholar]
- 8.Grol R, 2001. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 39: II46–II54. [DOI] [PubMed] [Google Scholar]
- 9.Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, Grilli R, Harvey E, Oxman A, O’Brien MA, 2001. Changing provider behavior: an overview of systematic reviews of interventions. Med Care 39: II2–II45. [PubMed] [Google Scholar]
- 10.Grimshaw JM, et al., 2004. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 8: iii–iv, 1–72. [DOI] [PubMed] [Google Scholar]
- 11.Flodgren G, Parmelli E, Doumit G, Gattellari M, O'Brien MA, Grimshaw J, Eccles MP, 2011. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 8: CD000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, O’Brien MA, Johansen M, Grimshaw J, Oxman AD, 2012. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 6: CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giguere A, Legare F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, Makosso-Kallyth S, Wolf FM, Farmer AP, Gagnon MP, 2012. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 10: CD004398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Victora CG, Schellenberg JA, Huicho L, Amaral J, El Arifeen S, Pariyo G, Manzi F, Scherpbier RW, Bryce J, Habicht JP, 2005. Context matters: interpreting impact findings in child survival evaluations. Health Policy Plan 20 (Suppl 1): i18–i31. [DOI] [PubMed] [Google Scholar]
- 15.Francke AL, Smit MC, de Veer AJE, Mistiaen P, 2008. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 8: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore GF, et al., 2015. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 350: h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duerden J, 2017. Nascent Book Culture Spreads in Rural Laos. Nikkei Asian Review. Tokyo, Japan: Nikkei Inc. [Google Scholar]
- 18.Logan J, Harrison MB, Graham ID, Dunn K, Bissonnette J, 1999. Evidence-based pressure-ulcer practice: the Ottawa model of research use. Can J Nurs Res 31: 37–52. [PubMed] [Google Scholar]
- 19.Graham K, Logan J, 2004. Using the Ottawa model of research use to implement a skin care program. J Nurs Care Qual 19: 18–24, quiz 25–26. [DOI] [PubMed] [Google Scholar]
- 20.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, 2005. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 14: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cane J, O’Connor D, Michie S, 2012. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 7: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bailie J, Laycock A, Matthews V, Bailie R, 2016. System-level action required for wide-scale improvement in quality of primary health care: synthesis of feedback from an interactive process to promote dissemination and use of aggregated quality of care data. Front Public Health 4: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Svoronos T, Mate KS, 2011. Evaluating large-scale health programmes at a district level in resource-limited countries. Bull World Health Organ 89: 831–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nzinga J, Mbindyo P, Mbaabu L, Warira A, English M, 2009. Documenting the experiences of health workers expected to implement guidelines during an intervention study in Kenyan hospitals. Implement Sci 4: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nzinga J, Ntoburi S, Wagai J, Mbindyo P, Mbaabu L, Migiro S, Wamae A, Irimu G, English M, 2009. Implementation experience during an eighteen month intervention to improve paediatric and newborn care in Kenyan district hospitals. Implement Sci 4: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR, 1999. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 282: 1458–1465. [DOI] [PubMed] [Google Scholar]
- 27.Chandler CI, Jones C, Boniface G, Juma K, Reyburn H, Whitty CJ, 2008. Guidelines and mindlines: why do clinical staff over-diagnose malaria in Tanzania? A qualitative study. Malar J 7: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.NICS, 2006. Identifying Barriers to Evidence Uptake. Melbourne, Australia: National Institute of Clinical Studies. [Google Scholar]
- 29.Martis R, Ho JJ, Crowther CA, 2008. Survey of knowledge and perception on the access to evidence-based practice and clinical practice change among maternal and infant health practitioners in southeast Asia. BMC Pregnancy Childbirth 8: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Herdman M, Fox-Rushby J, Badia X, 1997. ‘Equivalence’ and the translation and adaptation of health-related quality of life questionnaires. Qual Life Res 6: 237–247. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen QT, Joo JH, Yuen EJ, Nguyen ET, Sakata Y, Hang SC, Phommachanh S, 2009. Cultural and Linguistic Issues in Developing an Adaptation of the Geriatric Depression Scale for Laotian Elderly. Water and Public Health, APHA Annual Meeting and Expo. Philadelphia, PA: American Public Health Association. [Google Scholar]
- 32.Pariyo GW, Gouws E, Bryce J, Burnham G, 2005. Improving facility-based care for sick children in Uganda: training is not enough. Health Policy Plan 20 (Suppl 1): i58–i68. [DOI] [PubMed] [Google Scholar]
- 33.West C, Stewart L, Foster K, Usher K, 2013. Accidental insider: living the PhD study. Collegian 20: 61–65. [DOI] [PubMed] [Google Scholar]
- 34.Liamputtong P, 2009. Qualitative Research Methods. South Melbourne, Australia: Oxford University Press, 384. [Google Scholar]