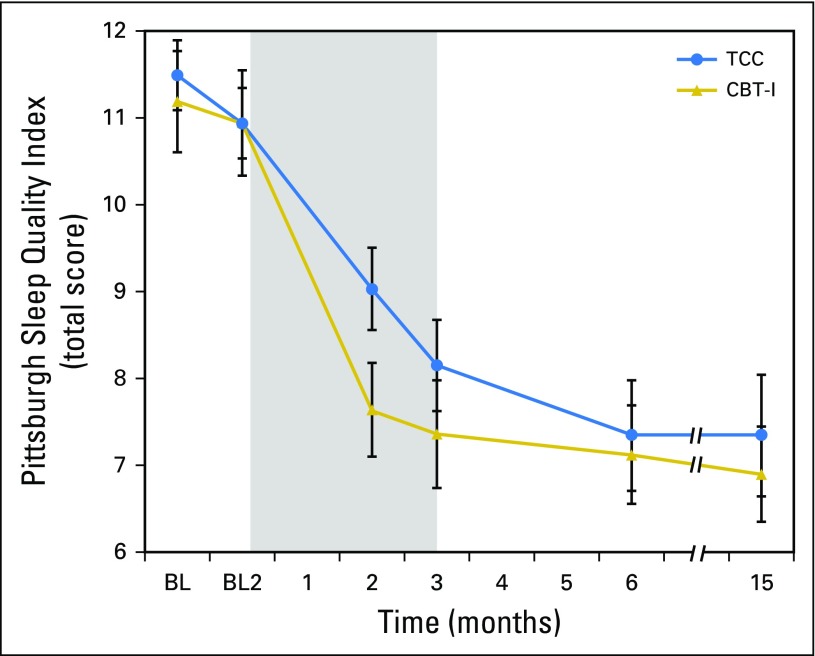
Fig 3.
Change in global sleep quality from baseline to month 15 follow-up in the cognitive behavioral therapy for insomnia (CBT-I) and Tai Chi Chih (TCC) treatment groups. Total scores on the Pittsburgh Sleep Quality Index range from 0 to 21, with higher scores indicating worse sleep quality. Values are means and bars indicate standard error of measurement. Measurements were obtained at baseline 1 (BL1; 2 months before intervention) and baseline 2 (BL2; immediately before intervention), and months 2 (midintervention), 3 (postintervention), and 6 and 15 (follow-up). The numbers of participants evaluated at each time point for each group are as follows: BL1: TCC, n = 45; CBT-I, n = 45; BL2: TCC, n = 45; CBT-I, n = 45; month 2: TCC, n = 38; CBT-I, n = 44; month 3: TCC, n = 38; CBT-I, n = 42; month 6: TCC, n = 35; CBT-I, n = 40; and month 15: TCC, n = 33; CBT-I, n = 40. Shaded area indicates period of exposure to treatment after baseline assessment. Comparisons between BL1 and BL2 were not significant (t377.7 = 0.2; P = .60). Significant pairwise comparisons were found between BL2 and months 2, 3, 6, and 15 (all P < .001). No significant differences were found between CBT-I and TCC at BL1, BL2, months 3, 6, and 15 (all P > .10), but CBT-I and TCC differed at month 2 (P < .02).