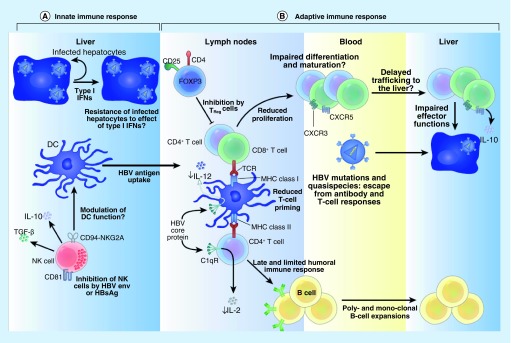
Figure 1. . Interactions between hepatitis B virus proteins and the immune system.
(A) Innate immune system: HBV-infected hepatocytes trigger a type 1 interferon response in the liver. This in turn primes DCs to antigen uptake, processing and initiation of an effective adaptive immune response. This interferon response also activates NK cells to lyse target (HBV-infected) cells and promote maturation of DCs. HBsAg can inhibit NK cells thereby downmodulating intrahepatic innate immunity. (B) Adaptive immune system: appropriate priming of T cells results in maturation of an effective HBV response that leads to secretion of protective antibodies and/or cytotoxic T cells in the lymph node. These HBV-specific T and B cells circulate to the liver via blood, targeted by CXCR3 and CXCR5 ligands. Chronic HBV infection is associated with enhanced Treg activity (inhibits T-cell maturation and proliferation), impaired humoral response (low protective antibodies), emergent escape mutants (ineffective cytotoxic T-cell response) and enhanced T-cell exhaustion. Collectively these effects contribute to HBV persistence.
DC: Dendritic cell; HBV: Hepatitis B virus; NK: Natural killer.