Abstract
Early use of mechanical circulatory support, e.g. veno-arterial extracorporeal membrane oxygenation (ECMO) or left ventricular unloading by microaxial pump in refractory cardiogenic shock is recommended in current guidelines. Development of acquired von Willebrand Syndrome (AVWS) in patients with left ventricular assist devices (LVADs) and ECMO has been reported. There is an increasing number of patients treated with the Impella® CP microaxial pump for left ventricular unloading. However, the prevalence of AVWS in these high risk patients is unknown and needs to be determined. We therefore screened 21 patients (68 ± 11years) treated with Impella® (17 for cardiogenic shock, 4 for protected PCI) for the presence of AVWS by determining von Willebrand factor multimers, VWF collagen binding capacity and VWF antigen. During the time course of Impella® support, 20/21 patients (95%) developed AVWS (mean duration of support: 135 ± 114 hours, mean time from device implantation to first diagnosis of AVWS: 10.6 ± 10.8 hours). Our data indicate that AVWS is a common phenomenon during left ventricular unloading via microaxial pump support. Thus, AVWS has to be considered as contributing factor for potential bleeding complications in this high risk patient population, especially in the context of dual antiplatelet therapy.
Introduction
Mortality of cardiogenic shock (CS) patients remains high despite improvement of intensive care strategies. Hence, current guidelines recommend the early use of mechanical circulatory support (MCS) in refractory CS [1].
Amongst others, options of MCS comprise veno-arterial extracorporeal membrane oxygenation (va-ECMO) bypassing the right and left ventricle [2] and microaxial pump for left ventricular unloading [3] such as the Impella® family. Microaxial pumps can easily be implanted under fluoroscopic guidance directly in the cath lab via transfemoral access. Blood is drawn from the left ventricle cavity and expelled above the aortic valve into the ascending aorta. Different Impella® devices are available varying in size and maximum flow capabilities [4]. As coronary ischemia is a major cause of CS, rapid revascularization is the treatment of choice. Consequently, dual antiplatelet therapy as well as systemic anticoagulation to prevent clotting of the device is indispensable on mechanical support. As triple therapy predisposes to bleeding complications, distinct therapy options depending on the underlying mechanism would be desirable.
Acquired von Willebrand syndrome (AVWS) is a bleeding disorder caused by structural or functional alterations of von Willebrand factor (VWF) commonly attributable to an underlying disease, such as hematological and autoimmune disorders and cardiovascular diseases. The latter group, for example, comprises patients with aortic valve stenosis [5] and the increasing cohort of permanent left ventricular assist device (LVAD) patients [6, 7]. In LVAD patients, shear stress-induced conformational change and subsequent proteolytic cleavage [8] is the proposed mechanism for AVWS. As Impella® microaxial pumps achieve very high shear rates we investigated the prevalence of AVWS in this patient cohort.
Methods
Patients
In this observational study, 21 consecutive patients with microaxial pump support Impella CP® were investigated between August 2016 and March 2017. Blood samples (2 x 3 mL) were drawn using commercial tubes containing 3.2% citrate which were directly sent to a certified laboratory where standardized testing for AVWS was performed. The collection of blood samples for research had been approved by the ethics committee at the Hannover Medical School.
Laboratory testing
AVWS analysis was performed in a core facility (Medilys Laboratory, Asklepios Klinik Altona, Hamburg, Germany) analyzing VWF antigen (VWF:Ag), VWF collagen binding activity (VWF:CB) and plasma VWF by electrophoresis of VWF to determine its multimeric structure. The VWF multimer pattern was analyzed using low-resolution agarose gel electrophoresis (1.2% lgt-agarose) [9]. Moreover, VWF activity (VWF:Act) assay was performed measuring agglutination of polystyrol particles coated with GPIb and addition of recombinant GPIb. The ratios of VWF:CB/VWF:Ag and VWF:Act/VWFAg were performed to quantify the functional capability of VWF. A ratio > 0.8 represents physiologic functionality of VWF [9]. In all patients VWF diagnostics was performed during Impella® treatment, in 12 patients, samples were available before as well as after Impella® implementation.
Anticoagulation and / or antiplatelet therapy
All patients were treated with unfractionated heparin during microaxial pump support aiming at an activated clotting time [ACT] of 160–180 sec. In addition to effective anticoagulation, 17 of the patients were on dual antiplatelet therapy after drug-eluting stent implantation.
Bleeding events
Bleeding events were assessed by the TIMI bleeding classification as previously reported [10].
Statistical analysis
Values are given as mean ± standard deviation (SD). For comparison between different time points Friedman’s nonparametric test for matched data was used followed by Dunn’s multiple comparisons test. Data were analyzed using GraphPad Prism 6.0 (GraphPad Software, Inc., La Jolla, CA).
Results & discussion
Patient characteristics are shown in Table 1. Mean age was 68 ± 11 years, and mean duration of Impella® support was 135 ± 114 hours. In addition to therapeutic administration of unfractionated heparin (target ACT 160–180 sec), 17 patients were on dual antiplatelet therapy (n = 6 aspirin + clopidogrel, n = 11 aspirin + prasugrel) due to prior coronary stent implantation (Table 1).
Table 1. Patient characteristics.
| N | 21 |
| Age (years) | 68 ± 11 |
| Sex (male) | 17 (81%) |
| Indication for microaxial pump support | |
| Cardiogenic shock | 17 |
| • Cardiopulmonary Resuscitation | 9/17 (53%) |
| - OHCA | 7/17 |
| - IHCA | 2/17 |
| • Protected PCI | 4 |
| Duration of Impella® support (hrs) | 135 ± 114 |
| Implementation of hypothermia (32°C for 24hrs) | 8/21 (30%) |
| Antiplatelet therapy | 19 |
| • aspirin–prasugrel | 11 |
| • aspirin–clopidogrel | 6 |
| • aspirin only | 2 |
| Bleeding events | |
| • TIMI bleeding | |
| - None | 3/21 (14.3%) |
| - Minimal | 5/21 (23.8%) |
| - Minor | 13/21 (61.9%) |
| - Major | 0/21 |
| Transfusion of blood products | |
| • Red blood concentrates | 5 ± 6 (13/21) |
| • Platelet concentrates | 0.4 ± 0.8 (3/21) |
| Intrahospital survival | 14/21 (66.7%) |
Values as number (%) of observation, means ± standard deviation
OHCA = out-of-hospital cardiac arrest
IHCA = in-hospital cardiac arrest; PCI = percutaneous coronary intervention
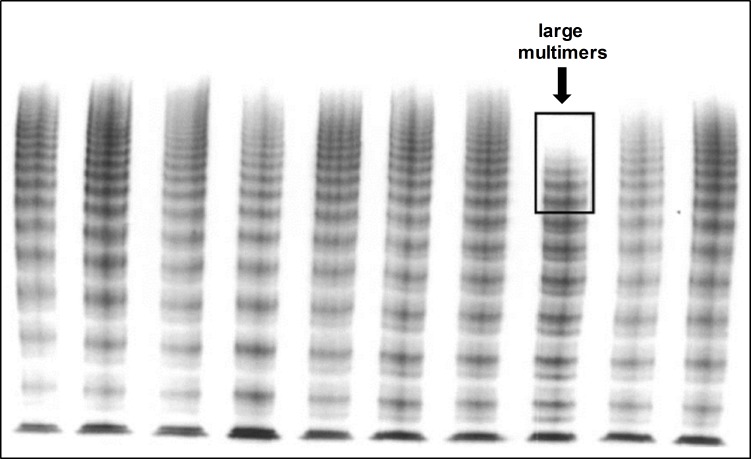
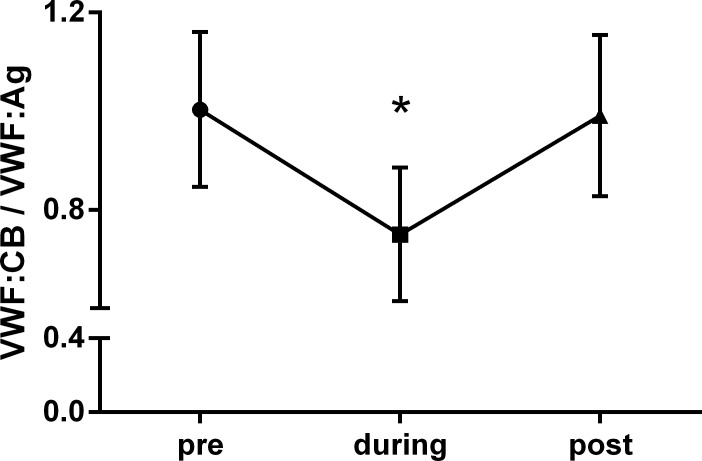
Ninety-five percent of patients were diagnosed with VWS, i.e. loss of very large multimers (Fig 1) and concomitant significant decrease of VWF:CB–VWF:Ag ratio (Fig 2). Occurrence of VWS was rapid, mean time from device implantation to first assessment of von Willebrand parameters was 10.6 ± 10.8 hours. In one patient, AVWS was detected as soon as 93 min post beginning of left ventricular unloading. For 12 patients, VW diagnostics were performed before as well as after removal of Impella® (mean time 25 hours post implantation and 58 hours post explantation). In all these patients, there was a significant increase in VWF:CB / VWF:Ag ratio compared to the ratio during microaxial pump support (Fig 2, Table 2), which is also reflected in regression of AVWS, i.e. recovery of large and very large multimers by electrophoresis (Fig 3). No correlation between level of left ventricular unloading and amount of high molecular weight multimers could be observed (data not shown). This is in line with a previous report of LVAD patients where device speed did not significantly influence the extent of VWF degradation [11]. Bleeding complications and the need for transfusion were more frequently observed in CS patients requiring device therapy over a longer period of time. No major bleeding events according to the TIMI classification could be observed. However, minor bleedings were frequent (Table 1), most often located in the nasopharyngeal area.
Fig 1. Representative electrophoresis.
Low-resolution gel (1.2%) of plasma from a patient with Impella® support (marked lane) compared to other plasma samples. Very large VWF multimers are missing, large multimers are reduced.
Fig 2. Course of VWF:CB / VWF:Ag ratio.
Significant reduction of VWF:CB / VWF:Ag ratio during Impella® support—and normalization after cessation of left ventricular unloading. n = 12, *p<0.05 vs pre / post Impella® therapy.
Table 2. Diagnostics of von Willebrand syndrome.
| Presence of AVWS | 20 / 21 (95%) |
| Time device implant–first diagnosis of AVWS (hrs) | 10.6 ± 10.8 |
| Platelet count (103 / μL) | 160 ± 61 |
| VWF: CB (%) | 213 ± 82 |
| VWF: Ag (%) | 265 ± 106 |
| VWF: Act (%) | 183 ± 56 |
| VWF: CB / VWF: Ag Ratio | 0.82 ± 0.1 |
| VWF: Act / VWF: Ag Ratio | 0.71 ± 0.2 |
VWF = von Willebrand factor; CB = collagen binding activity; Ag = antigen; AVWS = acquired von Willebrand Syndrome
Fig 3. Characteristic electrophoresis at different time points.
Characteristic low-resolution gel (1.2%) of a patient with Impella®: Very large multimers are absent and large multimes are reduced during microaxial pump support. Existence / recovery of large multimers is documented before and after mechanical left ventricular unloading. The right lane illustrates a characteristic trace of a plasma sample from a healthy person.
The presence of AVWS is a well-described observation in LVAD patients [12] and patients on ECMO [13, 14]. Recent data suggest two mechanisms to be involved in this phenomenon: shear stress induced mechanical damage and, more importantly, enzymatic cleavage by ADAMTS-13 (a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13) [15]. Interestingly, inhibition of ADAMTS-13 significantly decreased VWF degradation during supraphysiological shear stress without affecting platelet activity in an ex vivo setting [16].
Here, we for the first time describe the presence of AVWS in patients treated with a microaxial pump for left ventricular unloading. 17 of the 21 investigated patients were treated for cardiogenic shock, 7 of them after previous out-of-hospital resuscitation, 2 after prior in-hospital resuscitation. All of these patients developed AVWS and had minor bleeding complications according to the TIMI classification [10] (Table 1). As resuscitated patients were routinely subjected to therapeutic hypothermia (32°C core temperature) following cardiac arrest, and hypothermia by itself might increase the likelihood of bleeding, we cannot definitively relate the observed AVWS to the bleeding phenotype in this group of patients. However, apart from the patients undergoing protected PCI with only short-time microaxial pump support, almost all cardiogenic shock patients required red blood cell concentrates independently of hypothermia implementation. Triple anticoagulation by itself undoubtedly increases the risk of bleeding and cannot be withheld in patients with recent coronary intervention and microaxial pump support as presented in this cohort. It is unclear to what extent the presence of AVWS contributes to observed bleeding complications. Still, it is important to raise the awareness that genesis of bleeding is multifactorial.
In summary, it is tempting to speculate that AVWS alone might not be relevant in stable patients. However, in critically ill and hemodynamically unstable patients the development of AVWS should be considered as predisposing factor. This cohort most often requires dual antiplatelet therapy due to acute coronary intervention and frequently experiences a significant decrease in platelet count for various reasons [17]. As AVWS might be one factor contributing to bleeding complications, a specific treatment option, i.e. ADAMTS-13 inhibition, which might become available in the near future, would be desirable.
Supporting information
(PZFX)
(XLSX)
Acknowledgments
We thank the nursing staff of the cath lab and the cardiology intensive care unit for supporting this study. This study was supported by the German Research Foundation [Clinical Research Unit 311, BA 1742/9-1].
Data Availability
All relevant data are within the paper and its supporting information files.
Funding Statement
A.S. received grant support for research projects from Abiomed. This funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mebazaa A, Yilmaz MB, Levy P, Ponikowski P, Peacock WF, Laribi S, et al. Recommendations on pre-hospital and early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine—short version. European heart journal. 2015;36(30):1958–66. doi: 10.1093/eurheartj/ehv066 . [DOI] [PubMed] [Google Scholar]
- 2.Napp LC, Kuhn C, Hoeper MM, Vogel-Claussen J, Haverich A, Schafer A, et al. Cannulation strategies for percutaneous extracorporeal membrane oxygenation in adults. Clinical research in cardiology: official journal of the German Cardiac Society. 2016;105(4):283–96. doi: 10.1007/s00392-015-0941-1 ; PubMed Central PMCID: PMC4805695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schafer A, Bauersachs J. [Left ventricular unloading in cardiogenic shock]. Herz. 2017;42(1):18–26. doi: 10.1007/s00059-016-4512-7 . [DOI] [PubMed] [Google Scholar]
- 4.Burzotta F, Trani C, Doshi SN, Townend J, van Geuns RJ, Hunziker P, et al. Impella ventricular support in clinical practice: Collaborative viewpoint from a European expert user group. International journal of cardiology. 2015;201:684–91. doi: 10.1016/j.ijcard.2015.07.065 . [DOI] [PubMed] [Google Scholar]
- 5.Vincentelli A, Susen S, Le Tourneau T, Six I, Fabre O, Juthier F, et al. Acquired von Willebrand syndrome in aortic stenosis. The New England journal of medicine. 2003;349(4):343–9. doi: 10.1056/NEJMoa022831 . [DOI] [PubMed] [Google Scholar]
- 6.Geisen U, Heilmann C, Beyersdorf F, Benk C, Berchtold-Herz M, Schlensak C, et al. Non-surgical bleeding in patients with ventricular assist devices could be explained by acquired von Willebrand disease. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery. 2008;33(4):679–84. doi: 10.1016/j.ejcts.2007.12.047 . [DOI] [PubMed] [Google Scholar]
- 7.Meyer AL, Malehsa D, Budde U, Bara C, Haverich A, Strueber M. Acquired von Willebrand syndrome in patients with a centrifugal or axial continuous flow left ventricular assist device. JACC Heart failure. 2014;2(2):141–5. doi: 10.1016/j.jchf.2013.10.008 . [DOI] [PubMed] [Google Scholar]
- 8.Tsai HM, Sussman II, Nagel RL. Shear stress enhances the proteolysis of von Willebrand factor in normal plasma. Blood. 1994;83(8):2171–9. . [PubMed] [Google Scholar]
- 9.Meyer AL, Malehsa D, Bara C, Budde U, Slaughter MS, Haverich A, et al. Acquired von Willebrand syndrome in patients with an axial flow left ventricular assist device. Circulation Heart failure. 2010;3(6):675–81. doi: 10.1161/CIRCHEARTFAILURE.109.877597 . [DOI] [PubMed] [Google Scholar]
- 10.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449 . [DOI] [PubMed] [Google Scholar]
- 11.Kang J, Zhang DM, Restle DJ, Kallel F, Acker MA, Atluri P, et al. Reduced continuous-flow left ventricular assist device speed does not decrease von Willebrand factor degradation. The Journal of thoracic and cardiovascular surgery. 2016;151(6):1747–54 e1. doi: 10.1016/j.jtcvs.2016.01.031 . [DOI] [PubMed] [Google Scholar]
- 12.Nascimbene A, Neelamegham S, Frazier OH, Moake JL, Dong JF. Acquired von Willebrand syndrome associated with left ventricular assist device. Blood. 2016;127(25):3133–41. doi: 10.1182/blood-2015-10-636480 ; PubMed Central PMCID: PMC4920020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalbhenn J, Schmidt R, Nakamura L, Schelling J, Rosenfelder S, Zieger B. Early diagnosis of acquired von Willebrand Syndrome (AVWS) is elementary for clinical practice in patients treated with ECMO therapy. Journal of atherosclerosis and thrombosis. 2015;22(3):265–71. doi: 10.5551/jat.27268 . [DOI] [PubMed] [Google Scholar]
- 14.Tauber H, Ott H, Streif W, Weigel G, Loacker L, Fritz J, et al. Extracorporeal membrane oxygenation induces short-term loss of high-molecular-weight von Willebrand factor multimers. Anesthesia and analgesia. 2015;120(4):730–6. doi: 10.1213/ANE.0000000000000554 . [DOI] [PubMed] [Google Scholar]
- 15.Bartoli CR, Restle DJ, Zhang DM, Acker MA, Atluri P. Pathologic von Willebrand factor degradation with a left ventricular assist device occurs via two distinct mechanisms: mechanical demolition and enzymatic cleavage. The Journal of thoracic and cardiovascular surgery. 2015;149(1):281–9. doi: 10.1016/j.jtcvs.2014.09.031 . [DOI] [PubMed] [Google Scholar]
- 16.Bartoli CR, Kang J, Restle DJ, Zhang DM, Shabahang C, Acker MA, et al. Inhibition of ADAMTS-13 by Doxycycline Reduces von Willebrand Factor Degradation During Supraphysiological Shear Stress: Therapeutic Implications for Left Ventricular Assist Device-Associated Bleeding. JACC Heart failure. 2015;3(11):860–9. doi: 10.1016/j.jchf.2015.06.016 . [DOI] [PubMed] [Google Scholar]
- 17.Greinacher A, Selleng K. Thrombocytopenia in the intensive care unit patient. Hematology American Society of Hematology Education Program. 2010;2010:135–43. doi: 10.1182/asheducation-2010.1.135 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PZFX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its supporting information files.