Abstract
Introduction:
The number of centenarians in the United Kingdom is increasing. An associated increase in the incidence of hip fractures in the extreme elderly population is expected. The National Hip Fracture Database (NHFD) initiative was introduced in 2007 aiming to improve hip fracture care. There is a paucity of literature on the outcomes of centenarians with hip fractures since its introduction. The aim of this study is to report our experience of hip fractures in centenarians in the era since the introduction of the NHFD to assess outcomes in terms of mortality, time to surgery, length of stay, and complications.
Methods:
A retrospective case note study of all centenarians managed for a hip fracture over a 7-year period at a London district general hospital.
Results:
We report on 22 centenarians sustaining 23 hip fractures between 2008 and 2015. Twenty-one fractures were managed operatively. For patients managed operatively, in-hospital, 30-day, 3-month, 6-month, 1-year, 2-year, 3-year, and 5-year cumulative mortalities were 30%, 30%, 39%, 50%, 77%, 86%, 95%, and 100%, respectively. In-hospital mortality was 100% for those managed nonoperatively. Mean time to surgery was 1.6 days (range: 0.7-6.3 days). Mean length of stay on the acute orthopedic ward was 23 days (range: 2-51 days). Seventy-one percent had a postoperative complication most commonly a hospital-acquired pneumonia or urinary tract infection.
Conclusion:
Compared to a series of centenarians with hip fractures prior to the introduction of the NHFD, we report a reduced time to surgery. Mortality and hospital length of stay were similar.
Keywords: hip fracture, centenarian, extreme elderly, proximal femoral fracture, fragility fracture, National Hip Fracture Database
Introduction
The number of people living to the age of 100 in the United Kingdom has increased 73% to 13 350 in the decade to 2012.1 The incidence of hip fracture increases exponentially with age.2 There will likely be a continuing increase in the number of centenarians sustaining hip fractures in the coming years. Much recent attention has been drawn to the care of patients with hip fractures including the introduction of the National Hip Fracture Database (NHFD) initiative in England, Wales, Northern Ireland, and the Channel Islands in 2007.
The NHFD initiative aims to improve hip fracture care in part by assessing compliance with 6 national clinical standards for hip fracture care as published by the British Orthopaedic Association and British Geriatrics Society in The Care of Patients with Fragility Fractures. 3 Neuburger et al have recently assessed the impact of the NHFD initiative and found a significant reduction in 30-day mortality of hip fracture patients aged 60 years and older in England since its introduction.4 We could find no reports in the literature describing the outcomes of centenarians with hip fractures in the United Kingdom since the introduction of the NHFD initiative.
The most recent UK-based case series reporting mortality of centenarians with hip fractures was in 2003 and reported 1-month and 4-month mortality of 33.3% and 50%, respectively, with a mean length of stay on the acute orthopedic ward of 10.1 days.5
The aim of this study was to report our experience of hip fractures in centenarians in the era since the introduction of the NHFD initiative to assess outcomes in terms of mortality, time to surgery, length of stay, and complications.
Methods
Our district general hospital in Greater London manages a high volume of patients with hip fractures and maintains a prospective database of all patients admitted with a hip fracture. The database was searched to identify all patients admitted with a hip fracture between July 2008 and July 2015 who were 100 years or older at the time of injury. The case notes were retrospectively reviewed for all identified patients to verify the data recorded in the database. Identified patients’ general practitioners were contacted to ascertain dates of death.
The data analyzed included age, sex, preinjury accommodation and mobility, American Society of Anesthesiology (ASA) grade, Charlson comorbidity score,6 fracture configuration, time to surgery, anesthetic type, procedure and implant type, intraoperative and postoperative complications, length of stay, mobility at discharge, discharge destination, and survival. Accommodation was categorized into 1 of 4 groups: own home, sheltered housing, residential home, and nursing home. Mobility was graded on a scale from 1 to 5, with 1 being independent, 2 requiring a stick, 3 requiring a frame, 4 requiring assistance to transfer, and 5 hoist transfers/wheelchair/bedbound. GraphPad Prism version 6.0 for Mac OS (GraphPad Software, San Diego, California) was used for statistical analysis.
Results
In the 7-year period, 24 centenarians presented with 25 hip fractures to our unit (1 patient sustained fractures to both hips over a 2-month period). The case notes were available for review for 23 of these fractures. The demographics of the cohort are presented in Table 1. The mean age at admission was 101.4 years (range: 100.2-103.4 years). Fractures were sustained in 3 men and 19 women. Preinjury 13 lived in their own home, 5 in sheltered accommodation, 3 in residential homes, and 2 in nursing homes.
Table 1.
Demographic Data.
| Age | Sex | ASA Score | Time to Surgery, days | Fracture Type | Operation | Postoperative Complications | Length of Stay, days | Survival, days |
|---|---|---|---|---|---|---|---|---|
| 100.2 | F | 4 | 0.96 | Intracapsular | Uncemented hemiarthroplasty | Nil | 17 | 403 |
| 103.0 | F | 4 | 1.03 | Intracapsular | Uncemented hemiarthroplasty | HAP | 28 | 91 |
| 100.2 | F | 3 | 0.71 | Extracapsular | DHS | UTI | 15 | 800 |
| 100.7 | F | 1 | 0.83 | Intracapsular | Uncemented hemiarthroplasty | Nil | 16 | 769 |
| 100.9 | F | 3 | 3.40 | Extracapsular | DHS | HAP | 26 | 691 |
| 102.7 | F | 3 | 1.10 | Extracapsular | DHS | Myocardial infarction, atrial fibrillation | 2 | 2 |
| 101.8 | F | 3 | 0.85 | Intracapsular | Cemented hemiarthroplasty | HAP, atrial fibrillation | 43 | 185 |
| 102.8 | M | NR | n/a | Intracapsular | Nonoperative | UTI | 2 | 2 |
| 100.7 | F | 3 | 1.12 | Extracapsular | DHS | Nil | 12 | 224 |
| 100.3 | F | NR | n/a | Intracapsular | Nonoperative | HAP | 11 | 11 |
| 101.1 | F | 2 | 1.40 | Extracapsular | DHS | Nil | 15 | 1716 |
| 100.1 | F | 3 | 3.01 | Subtrochanteric | IMHS | UTI | 30 | 138 |
| 100.4 | F | 3 | 0.87 | Extracapsular | DHS | UTI, HAP | 25 | 42 |
| 103.4 | F | 2 | 1.37 | Intracapsular | Cemented hemiarthroplasty | Intraoperative cardiac arrest | 2 | 2 |
| 101.9 | F | 3 | 0.78 | Intracapsular | Uncemented hemiarthroplasty | HAP | 34 | 280 |
| 103.0 | F | 3 | 0.82 | Extracapsular | DHS | DVT | 37 | 42 |
| 100.8 | F | 4 | 1.84 | Extracapsular | IMHS | HAP | 30 | 30 |
| 101.3 | F | 3 | 0.75 | Intracapsular | Cemented hemiarthroplasty | HAP | 40 | 40 |
| 102.2 | F | 3 | 0.78 | Extracapsular | DHS | Nil | 20 | 141 |
| 100.2 | F | 4 | 1.39 | Intracapsular | Uncemented hemiarthroplasty | HAP | 27 | 171 |
| 101.7 | M | 3 | 3.00 | Intracapsular | Cemented hemiarthroplasty | Myocardial infarction, HAP | 51 | 151 |
| 100.6 | M | 3 | 1.49 | Intracapsular | Uncemented hemiarthroplasty | UTI | 40 | 40 |
| 101.9 | F | 3 | 6.31 | Intracapsular | Uncemented hemiarthroplasty | Nil | 25 | Still alive at the time of the study |
Abbreviations: ASA, American Society of Anesthesiologists; DHS, dynamic hip screw; DVT, deep vein thrombosis; F, female; HAP, hospital-acquired pneumonia; IMHS, intramedullary hip screw; M, male; NR, not recorded; UTI, urinary tract infection.
The ASA grade was III or IV in 86% of patients. Mean Charlson score was 1 (range: 0-2). Thirteen fractures were intracapsular, 9 were extracapsular, and 1 subtrochanteric. Twenty-one were managed operatively and 2 nonoperatively. Seven underwent uncemented hemiarthroplasty, 4 cemented hemiarthroplasty, and 10 fixation. Mean time to surgery was 1.6 days (range: 0.7-6.3 days). Forty eight percent underwent spinal anesthesia and 52% underwent general anesthesia. Mean length of stay on the acute orthopedic ward was 23 days (range: 2-51 days).
Seventy-one percent had a postoperative complication, most commonly a hospital-acquired pneumonia or urinary tract infection. Twenty-three percent of patients achieved their premorbid level of mobility at discharge. Forty-six percent of patients were discharged to the same level of accommodation from which they were admitted. For patients managed operatively, in-hospital, 30-day, 3-month, 6-month, 1-year, 2-year, 3-year, and 5-year cumulative mortalities were 30%, 30%, 39%, 50%, 77%, 86%, 95%, and 100%, respectively. Two patients were managed nonoperatively and survived 2 days and 11 days, respectively. Figure 1 shows a Kaplan-Meier survival curve for the cohort.
Figure 1.
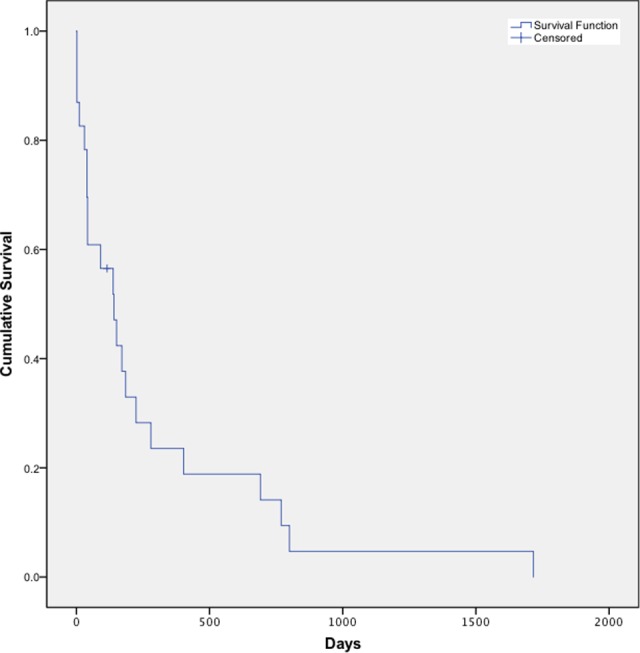
Kaplan-Meier survival curve for centenarians following hip fracture.
Discussion
Mortality
Forster and Calthorpe reported in their 2000 cohort of 13 centenarian hip fractures 30-day, 6-month, and 1-year mortality of 31%, 50%, and 56%, respectively.7 Oliver and Burke reported in 2003 on 18 centenarian hip fractures with in-hospital, 1-month, and 4-month mortality of 11.1%, 33.3%, and 50%, respectively.5 Verma et al reported in 2008 on 23 centenarians with inpatient and 30-day mortality of 17.3% and 30.4%, respectively.8 Shabat et al reported in 2004 on 19 centenarian hip fractures managed operatively in Israel with 6-month and 1-year mortality of 42%.9 Tarity et al reported in a 2013 cohort of 23 centenarian hip fractures in the United States in-hospital, 30-day, 90-day, 6-month, 12-month, 2-year, 3-year, and 6-year mortality of 15%, 20%, 30%, 45%, 60%, 70%, 90%, and 95%, respectively.10 Holt et al reported in 2008 on mortality in 919 Scottish older than 95 years with hip fractures with 30-day mortality of 16.8% and 120-day mortality of 38.1%.11
We report on 23 centenarian hip fractures operatively managed with in-hospital, 30-day, 3-month, 6-month, 1-year, 2-year, 3-year, and 5-year cumulative mortality of 30%, 30%, 39%, 50%, 77%, 86%, 95%, and 100%, respectively. One patient remained alive at the time of analysis 4 months following her surgery and thus was excluded from mortality analysis beyond 3 months. Compared to the most analogous series of Oliver and Verma, we report similar 30-day mortalities with a slightly reduced 3-month mortality as compared to Oliver’s series.5,8 Tarity’s and Shabat’s series represent different health-care environments with broadly similar mortality to our data.9,10 Holt et al demonstrated a reduced 30-day mortality and broadly similar rate of middle-term mortality in a large number of extreme elderly patients in Scotland with hip fractures.11 We believe ours to be the largest series of centenarian hip fractures reporting long-term mortality data.
The 2 patients in our series managed nonoperatively died at 2 and 11 days postadmission. One was deemed medically unfit to undergo anesthesia, and the other died prior to a planned hemiarthroplasty. Providing patients are considered well enough to survive anesthesia, this 100% rate of in-hospital mortality would support operative intervention even in this high-risk patient group.
Given the small numbers of patients involved and potential confounding factors, it is not possible to draw any conclusions about mortality in centenarian hip fractures since the introduction of the NHFD initiative. A larger scale review of mortality incorporating multicenter NHFD data would be required to assess this.
Time to Surgery
Of the 6 clinical standards, 1 introduced in 2007 in The Care of Patients with Fragility Fracture was that medically fit patients should have surgery within 48 hours of admission.3 Simunovic et al found in a systematic review in 2010 that earlier surgery after hip fracture was associated with a lower risk of death.12 Verma et al reported on a centenarian cohort in England between 2000 and 2007 and found a mean time to surgery of 3.65 days (95% confidence interval: 0.59-6.7 days).8 Our data show a mean time to surgery of 1.61 days (range: 0.7-6.3 days). The increased awareness of the importance of early surgery brought about by the NHFD initiative may in part has brought about this reduced time to surgery.
Implant Choice
Ten of our cohort sustained extracapsular hip fractures and were managed with dynamic hip screws or intramedullary hip screws. Of the 11 patients with intracapsular fractures managed operatively, 7 underwent uncemented hemiarthroplasty and 4 underwent cemented hemiarthroplasty. The understanding of bone cement implantation syndrome was improving during the period we report on. As suggested by Donaldson et al, discussion between surgical and anesthetic team was documented in a number of our cases, resulting in agreement to undertake uncemented hemiarthroplasty.13 The mean survival of those undergoing cemented hemiarthroplasty was 95 days (range: 2-185 days) and 292 days (range: 40-769 days) in those undergoing uncemented hemiarthroplasty (1 patient who underwent an uncemented hemiarthroplasty remained alive at the time of the study, so was excluded from this analysis). The difference was not statistically significant (P = .20) but shows a trend toward increased survival in the centenarian population with uncemented hemiarthroplasty.
Complications
Two patients in our cohort suffered intraoperative complications—1 patient undergoing a cemented hemiarthroplasty died following an intraoperative cardiac arrest. One patient undergoing an uncemented hemiarthroplasty sustained a calcar fracture, which was successfully cabled. One patient fell 20 days postoperatively, resulting in the failure of her dynamic hip screw which cut out. She underwent an uncomplicated revision to excision arthroplasty, after which she survived for 4.7 years.
Seventy-one percent of our cohort suffered some form of postoperative complication, most commonly a urinary tract infection or a hospital-acquired pneumonia. Roche et al reported in 2003 on over 2000 patients aged older than 60 with hip fractures and found 20% of patients suffered a postoperative complication.14 This increased rate of complications in the extreme elderly patients may represent a diminished physiological reserve in this high-risk patient group.
Length of Stay
Previous series of centenarians with hip fractures have reported lengths of in-hospital stays from 6.3 to 20.4 days.5,8,9,10 We report a mean length of stay of 23 days (range: 2-51 days). Our data include those treated both operatively and nonoperatively. These series represent different health-care environments and define in-hospital stay differently. Oliver et al reported a mean length of stay on acute orthopedic wards of 10.1 days, with a total hospital stay (including time on rehabilitation wards) of 53.9 days. Fabian reported hospitalization periods of 5 and 6 weeks for the 2 centenarian patients with hip fractures he reported on in 1991.15 For the period, we report on our unit maintained patients in acute orthopedic wards until discharge into the community, rather than with a step down to rehabilitation wards prior to discharge. This method of postoperative care may explain the longer length of stay we report as compared to previous series. When compared to the most comparable series of Oliver and Burke, our data suggest no significant change in the overall length of hospital stay since the introduction of the NHFD initiative.
Walking Ability and Residential Status
Oliver and Burke report 22.2% of surviving centenarians restored to their preinjury mobility.5 Shabat et al reported 4 (36%) of 11 patients restored to preinjury mobility.9 We report 23% restored to preinjury mobility at discharge. Oliver and Burke reported 31.3% of centenarians discharged directly back to their place of origin.5 We report 46% of centenarians surviving to discharge being discharged directly back to their place of origin, often with increased social services provision.
Limitations
As with all studies involving retrospective case note analysis, there is an inherent variability in the quality of data recorded as compared with data fully prospectively collected. Despite reviewing 7 years of care in one of the busier units for hip fractures in England, the number of patients included in the study is small. To further assess whether care has improved in the NHFD era, a larger multicenter study, or review of NHFD data, would be appropriate.
Conclusion
We report the largest series of centenarian hip fractures with long-term mortality data and the first series since the introduction of the NHFD. Mortality is consistent with previous series both in the United Kingdom and elsewhere. We report a reduced time to surgery in centenarians in the NHFD era with a broadly similar overall length of hospital inpatient stay. Patients aged older than 100 who sustain a hip fracture are a high-risk population. Despite the risk of complication being greater than 70%, our study would suggest that early operative treatment is a safe form of management for these patients.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Office for National Statistics. Statistical Bulletin: Estimates of the Very Old (including Centenarians) for England and Wales, United Kingdom, 2002 to 2013.2014. Available at: http://www.ons.gov.uk/ons/dcp171778_378107.pdf. Accessed July 19, 2017.
- 2. Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M. Epidemiology of hip fractures. Bone. 1996;18(suppl 1):S57–S63. [DOI] [PubMed] [Google Scholar]
- 3. British Orthopaedic Association, British Geriatrics Society. The Care of Patients with Fragility Fracture: British Orthopaedic Association 2007. Available at: http://www.bgs.org.uk/pdf_cms/pubs/Blue%20Book%20on%20fragility%20fracture%20care.pdf. Accessed July 19, 2017.
- 4. Neuburger J, Currie C, Wakeman R, et al. The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England an external evaluation using time trends in non-audit data. Med Care. 2015;53(8):686–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oliver CW, Burke C. Hip fractures in centenarians. Injury. 2004;35(10):1025–1030. [DOI] [PubMed] [Google Scholar]
- 6. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 7. Forster MC, Calthorpe D. Mortality following surgery for proximal femoral fractures in centenarians. Injury. 2000;31(7):537–539. [DOI] [PubMed] [Google Scholar]
- 8. Verma R, Rigby AS, Shaw CJ, Mohsen A. Acute care of hip fractures in centenarians—do we need more resources? Injury. 2009;40(4):368–370. [DOI] [PubMed] [Google Scholar]
- 9. Shabat S, Mann G, Gepstein R, Fredman B, Folman Y, Nyska M. Operative treatment for hip fractures in patients 100 years of age and older: is it justified? J Orthop Trauma. 2004;18(7):431–435. [DOI] [PubMed] [Google Scholar]
- 10. Tarity TD, Smith EB, Dolan K, Rasouli MR, Maltenfort MG. Mortality in centenarians with hip fractures. Orthopedics. 2013;36(3): e282–e287. [DOI] [PubMed] [Google Scholar]
- 11. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am. 2008;90(9):1899–1905. [DOI] [PubMed] [Google Scholar]
- 12. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(15):1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009;102(1):12–22. [DOI] [PubMed] [Google Scholar]
- 14. Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005; 331(7529):1374–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fabian W. Hip para-articular fractures in patients over 100 years old [in German]. Aktuelle Traumatol. 1991;21(1):13–15. [PubMed] [Google Scholar]


