Abstract
Background
Catholic hospitals operate under the Ethical and Religious Directives for Catholic Health Care Services, which for obstetrics and gynecology residents may create barriers to receiving adequate training in family planning.
Objective
We evaluated how training at a Catholic hospital affects trainees' subsequent provision of reproductive health services at secular institutions.
Methods
This qualitative study used semistructured interviews with recent obstetrics and gynecology graduates in generalist practice at secular institutions. We queried about their training experiences, perceived deficiencies, and current provision of family planning services. Three researchers independently coded transcripts, using grounded theory.
Results
We reached thematic saturation after 15 of 31 graduates (48%) from 7 Catholic hospital residencies participated in interviews between June 2014 and February 2015. Many participants reported a lack of awareness regarding limitations on this aspect of their training. All participants reported reproductive health care training deficiencies, and many explained that “elective” training required resident initiative to obtain. After graduation, participants reported dissatisfaction with training in family planning, delayed competency in this area, and a lack of ability to provide certain family planning procedures. All felt that Catholic programs should improve family planning training by providing routine, opt-out family planning opportunities.
Conclusions
Obstetricians and gynecologists who trained at Catholic institutions felt that religion-based policies negatively affected their training experiences and the range of reproductive health services they subsequently provide in practice. Forming collaborations with off-site facilities, particularly for postpartum tubal ligation and uterine evacuation, may improve the reproductive care these physicians ultimately provide to women.
What was known and gap
Accreditation Council for Graduate Medical Education (ACGME) standards require that all obstetrics and gynecology residents have access to training in family planning.
What is new
A qualitative analysis of the perceptions of recent graduates who trained in Catholic institutions showed barriers to training, reduced perceived competence, and reported reduced use of family planning services in practice.
Limitations
Study assessed resident perceptions, not actual training; there is a potential for bias.
Bottom line
Ethical objections at religious institutions create barriers to residents receiving training in the full range of family planning services, despite ACGME requirements.
Introduction
Obstetricians and gynecologists are expected to be experts in women's health care, including family planning services such as contraceptive, sterilization, and abortion services.1–3 The Accreditation Council for Graduate Medical Education (ACGME) recognizes religious, moral, or legal restrictions that interfere with family planning and abortion training, and its requirements stipulate all accredited obstetrics and gynecology programs must provide comprehensive family planning training to residents, with the opportunity to “opt out,” rather than the need to “opt in.”2 Despite these recommendations, discrepancies in abortion and family planning training exist among accredited programs.4–6
Catholic hospitals follow the Ethical and Religious Directives for Catholic Health Care Services that prohibit abortion services, and also limit the provision of and training in contraceptive and sterilization services.7 At least 10% (25 of 250) of the current obstetrics and gynecology residency programs in the United States are at faith-based hospitals that have restrictive policies on family planning service provision.8 The majority (72%, 18 of 25) are Catholic.8 Compared to residents at secular hospitals, residents at Catholic hospitals are less likely to report that they can independently perform contraceptive, sterilization, and uterine evacuation procedures,5 and are less likely to receive abortion training.6 Program directors of family medicine programs affiliated with religious hospitals report lower rates of training in family planning than those affiliated with secular hospitals.9
Understanding how institutional restrictions affect graduates' subsequent perceptions of practice can identify areas for improved training. The aim of this study was to understand if obstetrics and gynecology graduates of training programs affiliated with Catholic hospitals, who subsequently work at secular institutions, perceive deficiencies in their training and how these may affect the care they provide.
Methods
We chose a qualitative design to maximize our opportunity to elicit examples of training experiences at Catholic hospitals and the strategies used by graduates. We used purposive sampling and grounded theory to enhance the authenticity of the data.10–12 We selected study participants from 10 of 18 residency programs primarily affiliated with Catholic hospitals, with these institutions representing a range of US geographical areas. At each site, we contacted a program representative (eg, residency program director) and asked for contact information of graduates currently working as generalists at secular institutions. To reflect recent training experiences, we limited our sample to individuals between 1 and 5 years after graduation. Seven programs provided contact information, resulting in 31 potential participants. We recruited 1 to 3 representatives from each program to allow for variations in perceptions within programs, without oversampling certain programs. Our study excluded graduates from secular institutions, because we were interested in how the Ethical and Religious Directives for Catholic Health Care Services provided an added layer of complexity to reproductive health care training. We e-mailed potential participants and requested a 60-minute telephone interview. Participants received $50 as compensation.
The primary investigator (M.G.), an experienced qualitative investigator who has conducted prior research on this topic,5,13,14 created a semistructured interview guide (provided as online supplemental material) informed by prior research. The guide included open-ended questions about program selection, experience with reproductive health care training, perceived learning deficiencies, and current provision of family planning services (contraceptive management, sterilization practices, and management of abnormal or undesired pregnancies). Another author (J.H.), who had no prior relationship to the participants, conducted audio-recorded telephone interviews between June 2014 and February 2015. The interview guide was modified in response to evolving study findings. Interview recordings were transcribed by a professional service, and individual and institutional names were removed. We ended participant enrollment when thematic saturation was achieved.
The Colorado Multiple Institutional Review Board declared the study exempt.
We used grounded theory to analyze interviews. The 3 investigators deconstructed the data by independently coding each interview, triangulating observations, and reaching consensus on all designated codes. We then created a coding dictionary and refined it as new codes emerged. Next, we interpreted the data by creating a data display, and performed second-line coding to distinguish discrete concepts related to the same phenomena. We examined code details and used an iterative team process to interpret data and formulate plausible relationships within and among the categories. Based on the themes that emerged, we reconstructed the data, generated a conceptual framework, and re-reviewed the transcripts to ensure valid relationships. We used in-person group consensus to resolve differences in codes, subjective memo writing, and discussion of implicit biases based on each coder's personal experiences.10–12
Results
We reached thematic saturation after interviewing 15 of 31 eligible graduates (48%). Participants graduated between 2008 and 2013; the majority were female (14 of 15, 93%) and employed in private practice (11 of 15, 73%). Participants practiced in 11 US states. Five participants matched at 2 different residency programs that underwent institutional changes, resulting in training that was more restrictive.
Our conceptual framework (Figure) includes inputs into the selection of a residency training program at a Catholic hospital, on-site family planning training experience at Catholic hospitals, and outputs from residency training at Catholic hospitals. The Table shows representative quotes associated with inputs and outputs, respectively.
Figure.
Conceptual Framework for Inputs, Outputs, and Family Planning Training Experiences of Residency Training at Catholic Institutions
Abbreviations: FP, family planning; SARC, short-acting reversible contraceptives; LARC, long-acting reversible contraceptives; 1T, first trimester; D&C, dilation and curettage; OR, operating room; 2T, second trimester; IOL, induction of labor.
Note: Central wheel: Inner circle is the reported experience in family planning methods at Catholic hospitals. Middle circle demonstrates modifiers that affected family planning training within Catholic hospitals. Outer circle demonstrates strategies used at off-site centers to supplement family planning training.
Table.
Themes and Participants' Representative Quotes
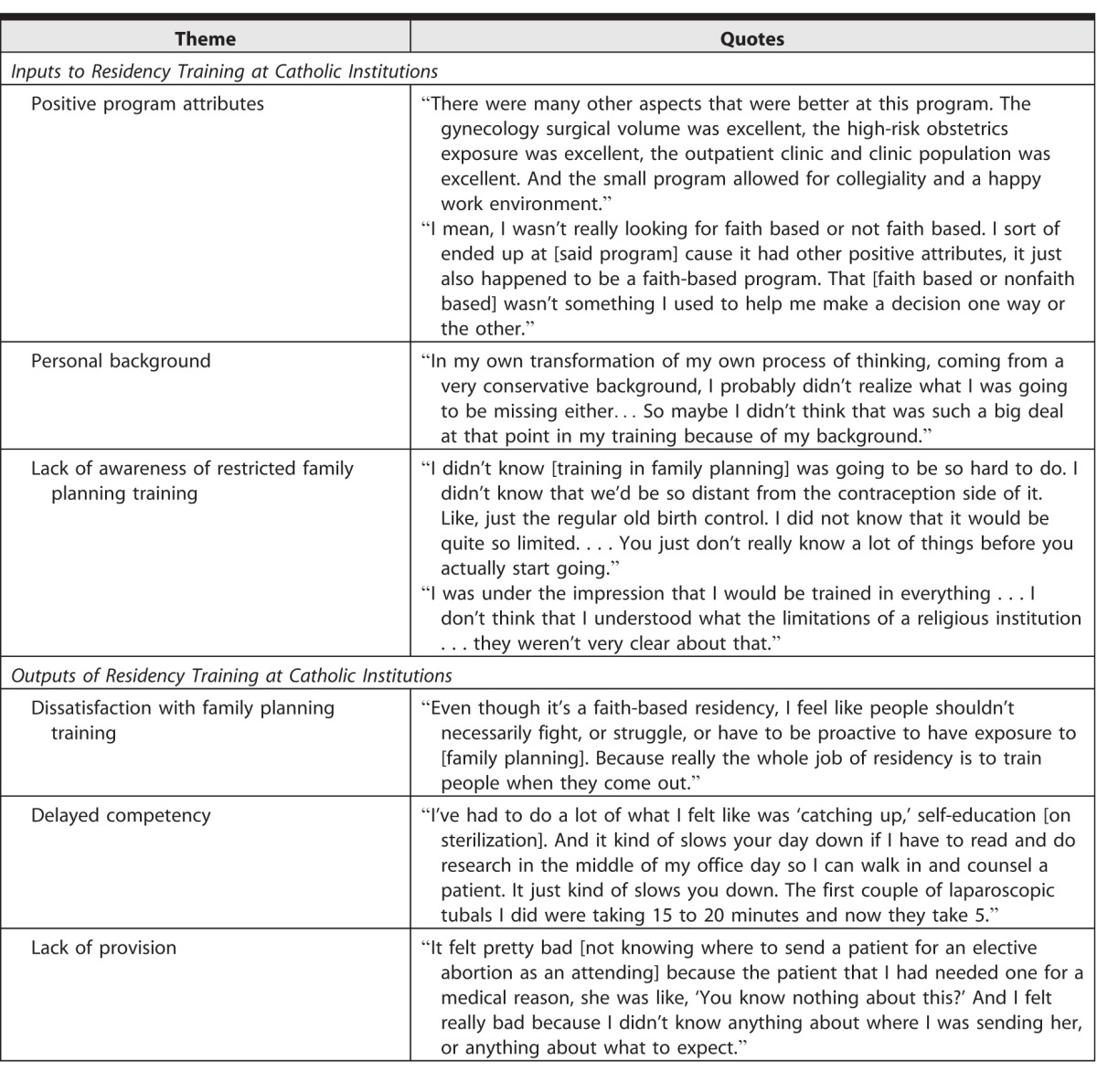
Inputs to Residency Training at Catholic Hospitals
Positive Program Attributes
When asked why they selected a residency program at a Catholic hospital, most participants reported that they did not base their decision on the degree of training in family planning. The majority cited other positive program attributes, such as location, surgical training, and faculty support (Table). A few reported that they preferred to not have routine abortion training, and a few had a negative reaction to the limited abortion training, but this was outweighed by other program attributes.
Personal Background
Several participants explained that during the interview process, they were less focused on the family planning training aspects of the program. Others described their personal values at the time were not aligned with seeking out family planning training (Table).
Lack of Awareness About Restricted Family Planning Training
The majority of interviewees reported that, although they were aware of abortion care restrictions, they did not realize there were restrictions on other areas of family planning (Table). A few reported that during residency interviews, training restrictions and difficulty obtaining off-site training were not sufficiently explained.
On-Site Family Planning Residency Training at Catholic Hospitals
Contraception
Most respondents reported that they were able to provide prescriptions for short-acting birth control methods to be filled off-site, and some indicated they provide injectable contraception on-site. A few reported they were prohibited from using hospital-branded prescriptions, and the vast majority reported minimal to no training on emergency contraception. Many interviewees had not placed or removed a contraceptive implant during training, and only received exposure through a pharmaceutical company training program. Most reported minimal training in on-site intrauterine device (IUD) insertion; a few reported no insertions. One participant described that because contraceptive access was limited, it wasn't emphasized: “We didn't learn that [contraception] was something that you talked about with a patient very early on in their prenatal care, [and] also at their annual visits . . . It just wasn't emphasized, and so it wasn't in the culture to make sure that it was discussed.”
Sterilization
Almost all respondents expressed frustration over the lack of training in postpartum and interval sterilization. Many interviewees had never performed a tubal ligation after a vaginal delivery during training. One reported, “The postpartum tubal. Those we did zero of [them] essentially, so I felt very ill prepared, and in fact, I don't even do them now.” Participants from a program that transitioned ownership to a Catholic system reported that residents lost their ability to provide postpartum and interval sterilizations.
Management of Miscarriage
For first trimester miscarriages, most graduates reported routinely performing in-hospital dilation and curettage and providing medical management. The majority never saw a manual vacuum aspiration procedure. For second trimester demises, most reported offering induction of labor, and indicated they rarely or never provided a dilation and evacuation (D&E).
Abortion
All participants reported no routine on-site abortion training. A few said that they provided options counseling, but many felt that they were not adequately trained in abortion counseling techniques. For example, a participant explained, “I mean they let us [counsel about abortion]; no one ever told us we cannot counsel someone about an elective abortion, but we just never did. . . I didn't even know where the place in town was that they do abortions until I got out of residency and met someone who needed it.” Some did not provide referrals. On-site experiences related to postabortion complications were reported to be rare.
Family Planning Training at Catholic Hospitals
Educational Activities
Some participants reported attending didactic lectures and simulation experiences that improved their family planning knowledge and counseling skills. Most interviewees reflected that classroom-based learning was not the same as practice-based learning, and that it was not sufficient to achieve procedural competency.
Related Skills
Participants acquired other skills during residency that they applied to family planning procedures. Most commonly, they felt competent in laparoscopy and explained that additional skills for interval sterilization were easy to acquire.
Noncontraceptive Indications
Some reported better training exposure because they used family planning interventions for noncontraceptive indications (eg, levonorgestrel IUD for heavy menstrual bleeding). A few described directive counseling specifically to elicit possible noncontraceptive indications from patients desiring contraception, and an exaggeration of noncontraceptive indications in documentation to help patients achieve family planning goals. One participant noted, “We definitely put in Mirenas, but we only could do them for menorrhagia, so possibly some patients [diagnosed with] menorrhagia maybe really didn't actually have menorrhagia, you know, I would say our diagnosis was maybe a little bit more lax.” Participants also received occasional approvals from the hospital's ethics committee for postpartum tubal ligations during cesarean sections for patients with medical indications.
Faculty
Many respondents appreciated that the culture set by key faculty members did not include rigid agreement with institutional restrictions. They noted that some faculty provided additional teaching to compensate for institutional limitations and were supportive of obtaining training off-site. Several were frustrated when procedures were not restricted (eg, D&E for fetal demise), but there were few or no faculty members who were competent in this procedure.
Training Environment
Many interviewees reflected on how their training environment negatively affected their interactions with patients in need of family planning services. Because birth control options were unavailable, participants reported they did not routinely counsel patients or know the full range of options available. Several described a range of efforts to provide patients with better family planning options:
“There's no doubt that many decisions, and logistic planning, and figuring out how to get things done w[ere] purely based on the limitations of the Catholic system that was placed on us. I don't think it improved the well-being of the patients. I think it put the patients at risk in many situations, and [the setting] made it hard for us to do what we thought was the right thing for the patient.”
Off-Site Modifiers to Family Planning Training
Elective Off-Site Training
Participants reported that during interviews, programs told them that they could use elective time or pursue off-site training opportunities for family planning services. Many interviewees commented that this was logistically difficult, because there was no elective time or they had competing interests. Several reported that an established relationship with an off-site facility did not exist, and that it was difficult to arrange an ad hoc rotation. Participants described challenges in obtaining elective training: “I think that [obtaining off-site family planning training] was an inconvenient thing to actually facilitate and make happen, and so I think that because of that it was a little bit discouraged.” A few commented that obtaining off-site training required a strong desire and initiative to overcome barriers.
Routine Off-Site Training
Participants described several strategies used to improve their training. Some received contraceptive training at off-site community health clinics or private practice offices, and several obtained interval tubal ligation experience in private office settings or at surgical centers. One program initially had a separate “secular” floor within a Catholic hospital in which trainees were able to provide sterilizations. However, during participants' training, this floor was closed and the services were discontinued. A few programs offered routine, opt-out abortion training opportunities at an off-site, freestanding clinic, but participants explained that these opportunities were limited and did not result in competency.
Outputs From Residency Training at a Catholic Hospital
Dissatisfaction With Family Planning Training
Most participants reported satisfaction with their overall residency education, yet almost all cited frustrations with their limited training in certain aspects of reproductive health care. Participants who did not receive off-site training reported the greatest frustration (Table). Graduates who described more restrictive changes implemented during their residency reported dissatisfaction and worried about future resident training. A few appreciated learning an approach to family planning that included religious considerations. All proposed that programs at Catholic hospitals should improve family planning training by providing more opportunities; the most common suggestion was nonelective off-site training.
Delayed Competency
Due to their limited residency training in contraception, sterilization, and medical management of miscarriage, many interviewees described using various strategies after graduation to achieve competency (Table), including trial and error, formal self-education, shadowing and inquiring with partners or colleagues, and overcompensating for their training deficiency by providing certain family planning services more frequently to gain competency.
Participants often relied on pharmaceutical representatives to educate them on the differences between pill formulations, obtain implant training, or ensure competency in hysteroscopic sterilization. For IUD placements, many watched manufacturer or YouTube videos online. A few graduates relied on surgical technicians to provide sterilization guidance. The majority needed their partners to train them in postpartum sterilization. Participants reported that it took weeks to a full year in practice to feel comfortable counseling and/or providing these services.
Lack of Provision
A few participants described difficulties with counseling patients about family planning services (Table), and others reported they were uncomfortable counseling about contraceptive pill considerations such as specific formulations.
Many reported that because of inadequate training, they do not provide certain sterilization and/or uterine evacuation procedures. Some do not offer postpartum and/or hysteroscopic sterilizations. Some interviewees explained that they do not provide office-based first trimester uterine evacuations for miscarriage management because they never saw this procedure performed. Most reported that in cases of second trimester demises, they only offer induction of labor. The majority reported that they do not offer elective abortion services because of personal values or because their practice prohibits it. A few who received off-site abortion training and perform D&Es in the early second trimester reported that if they had received more training, they would offer D&Es at later gestational ages.
Discussion
Graduates of obstetrics and gynecology residency programs affiliated with Catholic hospitals, who subsequently work at secular institutions, perceive that their ability to provide family planning services is compromised. Most reported a “catching up” period to develop competency in contraceptive and sterilization practices, and many relied on pharmaceutical representatives for medical education. Some reported never providing certain procedures that they would have otherwise offered, including postpartum tubal ligation, hysteroscopic sterilization, outpatient dilation and curettage, and D&E for abnormal pregnancy. Our study also highlights that there is a range of family planning training experiences for residents at Catholic programs. When opt-out, off-site training occurred, participants reported greater satisfaction and a shorter time to develop competency after graduation. None of the interviewees felt their program provided sufficient off-site training in all areas of family planning to compensate for the lack of these elements in their regular curriculum and experiences.
Our findings confirm prior surveys that residents at Catholic hospitals experience family planning training deficiencies despite the ACGME mandate5,6 and show the consequences of restricted training on the actual provision of women's health care. The rising number of Catholic health system mergers may affect a greater number of residents in the future.15 To ensure that all residents are trained and able to provide family planning services after graduation, program directors and the Review Committee for Obstetrics and Gynecology should address training limitations at Catholic and other faith-based hospitals.
There are limitations to our study. Participants graduated from 7 different programs, accounting for 39% of training programs at Catholic hospitals. We did not contact all programs, since many Catholic hospitals are clustered in the Midwest, and we wanted to equally weigh experiences in other parts of the country. We did not receive responses from all contacts, and our enrollment process may have introduced bias. Our interviews did not include participants who chose their residency program because of restrictive family planning policies. We acknowledge that routine abortion training at secular institutions is not uniform,4,6 and that barriers exist independent of religious-based policies.13 Finally, we sampled graduates from Catholic hospitals who subsequently work at secular institutions, and their perceptions may not reflect peers who work in other settings, including Catholic or other faith-based hospitals.
Conclusion
Without improved family planning training, residents at Catholic and other restrictive faith-based hospitals will continue to graduate less satisfied with their training, less competent, and less likely to offer such services than graduates of secular hospitals. Ultimately, patients may suffer from inadequate counseling and delays in obtaining needed family planning services.
Supplementary Material
References
- 1. ACOG Committee Opinion No. 612: Abortion training and education. Obstet Gynecol. 2014; 124 5: 1055– 1059. [DOI] [PubMed] [Google Scholar]
- 2. Accreditation Council for Graduate Medical Education Review Committee for Obstetrics and Gynecology. Clarifications of program requirements. http://www.acgme.org/portals/0/pfassets/programresources/220_obgyn_abortion_training_clarification.pdf. Accessed May 24, 2017.
- 3. Council on Resident Education in Obstetrics and Gynecology Educational Objectives. Core Curriculum in Obstetrics and Gynecology. 11th ed. Washington, DC: American College of Obstetricians and Gynecologists; 2016.
- 4. Turk JK, Preskill F, Landy U, et al. Availability and characteristics of abortion training in US ob-gyn residency programs: a national survey. Contraception. 2014; 89 4: 271– 277. [DOI] [PubMed] [Google Scholar]
- 5. Guiahi M, Westhoff CL, Summers S, et al. Training at a faith-based institution matters for obstetrics and gynecology residents: results from a regional survey. J Grad Med Educ. 2013; 5 2: 244– 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eastwood KL, Kacmar JE, Steinauer J, et al. Abortion training in United States obstetrics and gynecology residency programs. Obstet Gynecol. 2006; 108 2: 303– 308. [DOI] [PubMed] [Google Scholar]
- 7. United States Conference of Catholic Bishops. Ethical and Religious Directives for Catholic Health Care Services. 5th ed. Washington, DC: United States Conference of Catholic Bishops; 2009. http://www.usccb.org/issues-and-action/human-life-and-dignity/health-care/upload/Ethical-Religious-Directives-Catholic-Health-Care-Services-fifth-edition-2009.pdf. Accessed May 24, 2017. [PubMed]
- 8. American Medical Association. Search the AMA residency and fellowship database. https://www.ama-assn.org/life-career/search-ama-residency-fellowship-database. Accessed May 24, 2017.
- 9. Herbitter C, Greenberg M, Fletcher J, et al. Family planning training in US family medicine residencies. Fam Med. 2011; 43 8: 574– 581. [PubMed] [Google Scholar]
- 10. Strauss AC, Corbin JM. . Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 11. Sullivan GM, Sargeant J. . Qualities of qualitative research: part I. J Grad Med Educ. 2011; 3 4: 449– 452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sargeant J. . Qualitative research part II: participants, analysis, and quality assurance. J Grad Med Educ. 2012; 4 1: 1– 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guiahi M, Lim S, Westover C, et al. Enablers of and barriers to abortion training. J Grad Med Educ. 2013; 5 2: 238– 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guiahi M, Cortland C, Graham MJ, et al. Addressing OB/GYN family planning educational objectives at a faith-based institution using the TEACH program. Contraception. 2011; 83 4: 367– 372. [DOI] [PubMed] [Google Scholar]
- 15. Uttley L, Reynertson S, Pawelko R, et al. Merging Catholic and non-sectarian hospitals: NYS models for addressing the ethical challenges. http://static1.1.sqspcdn.com/static/f/816571/23042588/1372882137057/Models+of+Catholic-secular+hospitals+mergers+in+NYS.pdf?token=zYEZfgnCmvaAVnHjr2Y8%2ByZcLKw%3D. Accessed May 24, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



