Abstract
Background
Epoxyeicosatrienoic acids (EETs) derived from cytochrome P450 (CYP)-dependent metabolism of arachidonic acid are increased in the plasma of women with preeclampsia as compared with normal pregnancy and are significantly higher in fetal than in maternal plasma and erythrocytes. We hypothesized that differences in EET synthesis or metabolism in the feto-placental unit contributed to the observed differences in circulating EETs.
Method
To evaluate EETs, formation as well as the expression of relevant CYP isoforms and the metabolizing enzyme, soluble epoxide hydrolase (sEH), biopsies of placenta were collected from 19 normal pregnancy and 10 preeclampsia at the time of cesarean section delivery. EETs were extracted from tissue homogenates and analyzed by liquid chromatography coupled with tandem mass spectrometry.
Results
Both cis-EETs and trans-EETs were detected in the placenta. Concentration of total EETs was higher in the placenta from preeclampsia compared with normal pregnancy (2.37 ± 1.42 ng/mg vs. 1.20 ± 0.72 ng/mg, mean ± SD, P < 0.01), especially the 5,6-, 8,9- and 11,12- EETs, measured in a subgroup of tissue samples (normal pregnancy = 10, preeclampsia = 5). By immunohistochemistry, sEH, CYP2J2, CYP4A11 were present in placental villi with different pattern distribution, whereas CYP2C8 was not detectable. Neither were CYP2J2, CYP4A11, and CYP2C8 detected in the umbilical cord. Western blot analysis of placenta homogenates showed reduced expression of sEH in preeclampsia as compared with normal pregnancy.
Conclusion
Increased EETs in the placenta and umbilical cord are associated with the presence of CYP2J2, whereas reduced expression of sEH in preeclampsia may be the key factor of increased EETs in the placenta.
Keywords: cytochrome P450, epoxyeicosatrienoic acids, hypertension, placenta, preeclampsia, soluble epoxide hydrolase
INTRODUCTION
Preeclampsia is a disorder of pregnancy defined as the onset of hypertension [arterial blood pressure (BP) ≥140/90 mmHg] and proteinuria (>300 mg/24 h) after the 20th week of gestation [1]. Widespread endothelial dysfunction, with altered placentation, is a key feature of the disease. The etiology and the cascade of events leading to the syndrome are still unclear [1]. Epoxyeicosatrienoic acids (EETs) and cytochrome P450 (CYP) metabolites of arachidonic acid are important lipid mediators capable of altering vascular properties. EETs have primarily vasodilatory (acting as endothelial-derived hyperpolarizing factors), antihypertensive, antiinflammatory and natriuretic properties, although in different organs and clinical settings may exert vasoconstrictor activities either directly or after metabolism via cyclooxygenases to a thromboxane analogue [2,3]. EETs are mostly hydrolyzed by soluble epoxide hydrolase (sEH) into dihydroxyeicosatrienoic acids (DHETs), which circulate in the blood and are excreted in the urine [4].
EETs are mainly generated in the liver, kidney and vascular endothelium [5]. EETs and DHETs have also been detected in the placenta [6–8]. More recently, 5,6-, 8,9-, 11,12- and 14,15-EETs were found in intrauterine tissues of normotensive pregnancies, including fetal membranes (amnion and chorion) and fetal villous tissue [9]. Indeed, 5,6- and 11,12-EETs were present in higher amounts in the placental trophoblast with respect to amnion and chorion [9].
While in other forms of secondary hypertension, such as renovascular hypertension, a significant decrease in plasma EETs was found [10]. An increase in plasma EETs concentration was observed in pregnant women with respect to nonpregnant women, with the highest values of 5,6- and 14,15-EETs and DHETs observed in preeclamptic women [2,11]. This finding could be relevant in the pathophysiology of the disease. The feto-placental unit may contribute to EETs biosynthesis, as there is evidence that EETs concentration is much higher in fetal than in maternal plasma and erythrocytes [11]. The increase in plasma EETs observed during pregnancy might depend on increased synthesis, as immunohistochemistry localized CYP2J2 in trophoblastic villi and decidua, and the CYP2J2 mRNA was found to be upregulated in the placenta of preeclamptic women [2].
The increase in plasma EETs in preeclampsia may also derive from reduced hydrolysis to DHETs, although no evidence so far is available concerning the expression of sEH in the placenta or other intrauterine tissues.
The aim of the present study was to localize the site of production and elucidate the mechanisms of the increased release of EETs observed in normal and preeclamptic pregnancies, with the hypothesis that a major contribution derives from the intrauterine tissues. We therefore measured EETs and their epoxide metabolites DHETs in homogenates of placenta and umbilical cord. Using immunohistochemistry and western blot analysis, we sought to localize and quantify in those tissues the enzymes involved in EETs synthesis and metabolism.
METHODS
The clinical study was performed at the Verona University Hospital, where all samples were collected and stored. The study was approved by the Ethics Committee of the Verona University Hospital (code: CESC1525). All participants signed written informed consent after receiving full written information about the research project.
Patients
Both normotensive and preeclamptic pregnant women, identified according to the AIPE guidelines (‘International Society for the study of hypertension in Pregnancy’), were enrolled. A total of 10 preeclamptic and 19 normotensive pregnant women, matched for age and BMI, were enrolled. Placental and umbilical cord tissues were collected from all the studied women at the time of surgical delivery. The clinical characteristics of preeclamptic and normal pregnant women are shown in Table 1.
TABLE 1.
Characteristics of normal and preeclamptic pregnancies
| Variables | Preeclampsia (n = 10) | Normal pregnancy (n = 19) | P values (t test) |
|---|---|---|---|
| Age (year) | 33.60 ± 5.3 | 36.05 ± 4.45 | 0.197 |
| Pregnancy (week) | 33.8 ± 3.39 | 38 ± 0.75 | 0.003 |
| Placenta weight (g) | 295.3 ± 111.24 | 559.59 ± 88.97 | <0.001 |
| Birth weight (g) | 1751.5 ± 786.4 | 3153.7 ± 510.9 | <0.001 |
| Percentile birth weight (%) | 29.0 ± 22.1 | 55.0 ± 20.0 | 0.003 |
| SBP (mmHg) | 141.67 ± 17.35 | 117.68 ± 13.39 | <0.001 |
| DBP (mmHg) | 86.11 ± 12.85 | 74.77 ± 10.05 | 0.017 |
| Antihypertensive medications (n) | 1.5 ± 0.7 | 0 | <0.001 |
| BMI (kg/m2) | 21.32 ± 2.37 | 23.44 ± 3.39 | 0.097 |
| Proteinuria (mg/dl) | 175.5 ± 143.9 | 13.5 ± 13.8 | <0.001 |
| Hematocrit (%) | 34.98 ± 1.65 | 35.31 ± 3.08 | 0.760 |
| Platelets (cell/µl) | 252.100 ± 87.571 | 247.368 ± 77578 | 0.882 |
| C-reactive protein (mg/l) | 4.34 ± 3.65 | 3.43 ± 2.95 | 0.474 |
| Plasma creatinine (mg/dl) | 0.74 ± 0.14 | 0.57 ± 0.12 | 0.001 |
| Clearance creatinine (ml/min) | 109.31 ± 29.5 | 149.62 ± 48.19 | 0.024 |
| Plasma uric acid (mg/dl) | 6.6 ± 0.91 | 4.24 ± 1.03 | <0.001 |
| Plasma glucose (mg/dl) | 92.40 ± 20.17 | 77.89 ± 10.15 | 0.015 |
| Plasma cholesterol (mg/dl) | 281.89 ± 46.91 | 272.5 ± 65.77 | 0.706 |
| Plasma triglycerides (mg/dl) | 322.44 ± 104.45 | 263.56 ± 97.70 | 0.161 |
Sample collection from placenta and umbilical cord
Cesarean section in preeclampsia was performed, most of the times, for maternal complications related to the hypertensive disorder or for fetal growth restriction, whereas in normal pregnancies, surgery was the elective mode of delivery upon maternal request, usually the woman’s choice after a previous cesarean section. At the time of the delivery, right after placental removal, a sample was collected under sterile conditions: the slice of placenta was cut in a triangular shape with the apex corresponding to the insertion of the umbilical cord, with an angle of nearly 20°. We paid special attention in excluding areas with macroscopic evidence of ischemic or hemorrhagic infarction. A nearly 10 cm-long segment of umbilical cord was taken starting from the insertion to the placenta. The bioptic samples from the placenta and the cord were immediately snap frozen using liquid nitrogen and then stored at −80°C until analysis.
Measurement of eicosanoids in tissue samples
EETs were extracted from tissue homogenates and analyzed by liquid chromatography coupled with tandem mass spectrometry (LC–MS/MS). EETs isoforms were quantified in a subgroup of tissue samples (normal pregnant = 10; preeclampsia = 5).
Tissues were homogenized after thawing, and phospholipids were extracted and hydrolyzed as described [11]. After neutralization to pH at 7, EETs were extracted with ethyl acetate, dried under nitrogen, dissolved in acetonitrile and subjected to LC–MS/MS analyses to measure all the isoforms of EETs [11].
Immunohistochemistry
Immunohistochemical studies were performed on freshly frozen placental and umbilical cord biopsies. Briefly, sections were incubated with the following primary antibodies: a polyclonal rabbit antibody directed against sEH (Cayman; dilution 1 : 100), a polyclonal rabbit antibody against CYP2J2 (Santa Cruz Biotechnology; dilution 1 : 100), a mouse mAb against cytochrome P450 isoform 4A11 (CYP4A11) (Santa Cruz Biotechnology; dilution 1 : 100) and a polyclonal rabbit antibody directed against cytochrome P450 isoform 2C8 (CYP2C8) (Sigma; dilution 1 : 1000). The reactions were revealed by diaminobenzidine tetrahydrochloride. Finally, slides were counterstained with Mayer’s hematoxylin. Histological analysis was performed to identify cell types and the characteristics of tissues.
Digital pathology analysis
Glass slides were scanned using D-Sight (VysiaImaging Company, Florence, Italy) to facilitate fast acquisition, navigation, analysis, archiving and transfer of high quality digital images. By using the image multipreview, the user was able to select and display specific areas of interest (positive immunoexpression) within each tissue to ensure quality interobserver consistency in assessment positivity.
Western blot analysis of soluble epoxide hydrolase
Placental tissue was homogenized in ice-cold radio immunoprecipitation assay buffer (50 mmol/l Tris–HCl, pH 8.0, 150 mmol/l NaCl, 1 mmol/l EDTA, 1% NP-40, 0.1%SDS, 0.5% deoxycholic acid and protease inhibitor cocktail). The lysates were clarified by centrifugation at 1300 × g for 10 min, and protein concentration was determined with the Bradford method. Aliquots corresponding to 30µg of total proteins were loaded on a 10% T polyacrylamide. After electrophoresis, proteins were transferred to a nitrocellulose membrane. For immunoblotting, membranes were prehybridized with 10% nonfat dried milk in Tris-buffered saline for 1 h at real time and then incubated with primary antibody against sEH (Cayman, dilution 1 : 1000), overnight at 4 °C. After washing, membranes were incubated with peroxidase-conjugated antirabbit immunoglobulin G. The signal was revealed with ECL Advance Western Blotting Detection Kit (Amersham Pharmacia Biotech, Buckinghamshire, UK). Gels stained with Coomassie Brilliant Blue R-250 were used to assess protein loading.
Statistical analysis
Data are presented as mean and SD (mean ± SD), unless otherwise specified. Comparison between preeclamptic and nonpreeclamptic placentas, including immunoblot analysis, has been performed by using parametric tests (unpaired t test), after log transformation, if needed, and repeated by nonparametric Mann–Whitney U test. A two-tailed P value less than 0.05 was considered statistically significant.
RESULTS
Anthropometric characteristics and the biochemical profile of preeclampsia and normal pregnant women included in the present study are presented in Table 1. As expected, differences were observed in weeks of gestation at delivery and weight of the newborn and placenta. Different were also BP, plasma creatinine and urinary protein excretion other than plasma glucose and uric acid (see Table 1).
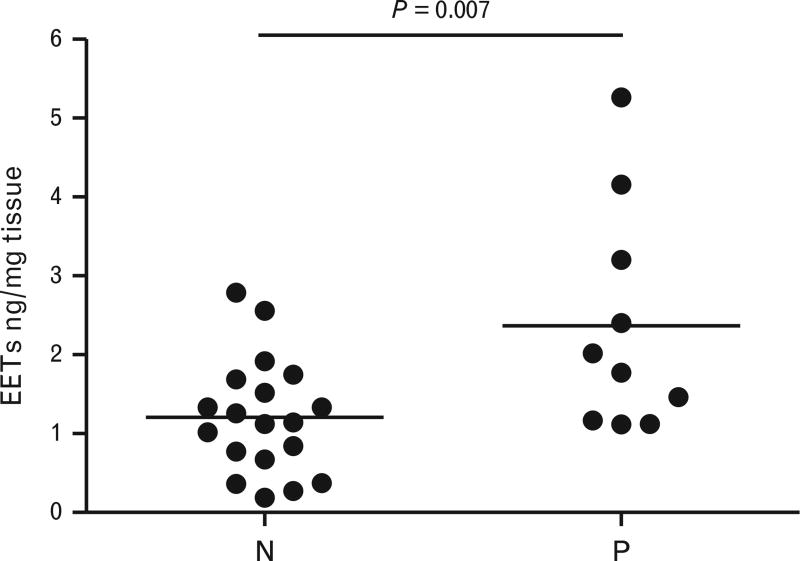
Epoxyeicosatrienoic acid isoforms
Both cis and trans-EETs were detectable in the placenta and umbilical cord (ratio 1 : 1). The total amount of EETs was higher in preeclampsia with respect to normal pregnancies (2.37 ± 1.42 vs. 1.21 ± 0.73 ng/mg, P < 0.01, Fig. 1), with higher concentration of almost all the isoforms except for 14,15-EETs (Table 2). The EETs/DHETs ratio, which can be assumed as an index of sEH activity [12], showed a tendency toward an increase (P = 0.07) in preeclampsia. No difference was detected in umbilical cords as for the whole set of eicosanoids (Table 2). Repetition of all these analyses by nonparametric statistics (Mann–Whitney U test) gave the same significant results. There was a difference in gestational week between preeclampsia and normal pregnant, which could account for the difference in EETs between the groups (see Supplementary Table S1, http://links.lww.com/HJH/A613). Even if a Pearson correlation between EETs and gestational age is significant (r = −0.45; P < 0.05), when considered in linear regression, only disease status and not gestation age, remained significantly associated with EETs (beta ± SEM = 1.162 ± 0.395; P = 0.007).
FIGURE 1.
Total epoxyeicosatrienoic acids concentration in the placenta of normotensive and preeclamptic pregnant women. Data are expressed as ng/mg of dry tissue. Bar indicates mean. P < 0.05 also by nonparametric test.
TABLE 2.
Epoxyeicosatrienoic acid isoforms and dihydroxyeicosatrienoic acids in placenta and umbilical cords from normotensive and preeclamptic women
| Variables | Preeclampsia (n = 5) | Normal pregnancy (n = 10) | P values (t test) |
|---|---|---|---|
| Placenta 5,6-EETs, ng/mg of tissue | 0.87 ± 0.43 | 0.27 ± 0.21 | 0.033 * |
| Placenta 8,9-EETs, ng/mg of tissue | 0.82 ± 0.41 | 0.31 ± 0.23 | 0.009 * |
| Placenta 11,12-EETs, ng/mg of tissue | 0.81 ± 0.48 | 0.27 ± 0.24 | 0.01 * |
| Placenta 14,15-EETs, ng/mg of tissue | 0.73 ± 0.42 | 0.34 ± 0.29 | 0.054 |
| Placenta DHETs, ng/mg of tissue | 0.57 ± 0.31 | 0.29 ± 0.22 | 0.07 |
| Placenta EETs/DHETs | 5.70 ± 1.55 | 4.08 ± 2.52 | 0.07 |
| Umbilical cord EETs, ng/mg of tissue | 1.03 ± 1.50 | 0.38 ± 0.28 | 0.19 |
| Umbilical cord DHETs, ng/mg of tissue | 0.54 ± 0.56 | 0.19 ± 0.17 | 0.09 |
Homogenates of placenta were analyzed by LC–MS/MS (see METHODS for further details). DHETs, dihydroxyeicosatrienoic acids; EETs, epoxyeicosatrienoic acids.
P < 0.05 also by nonparametric test.
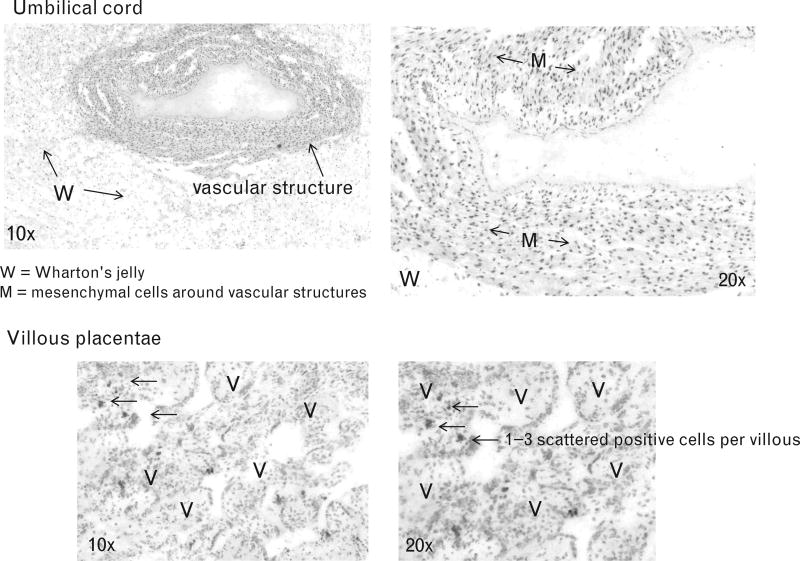
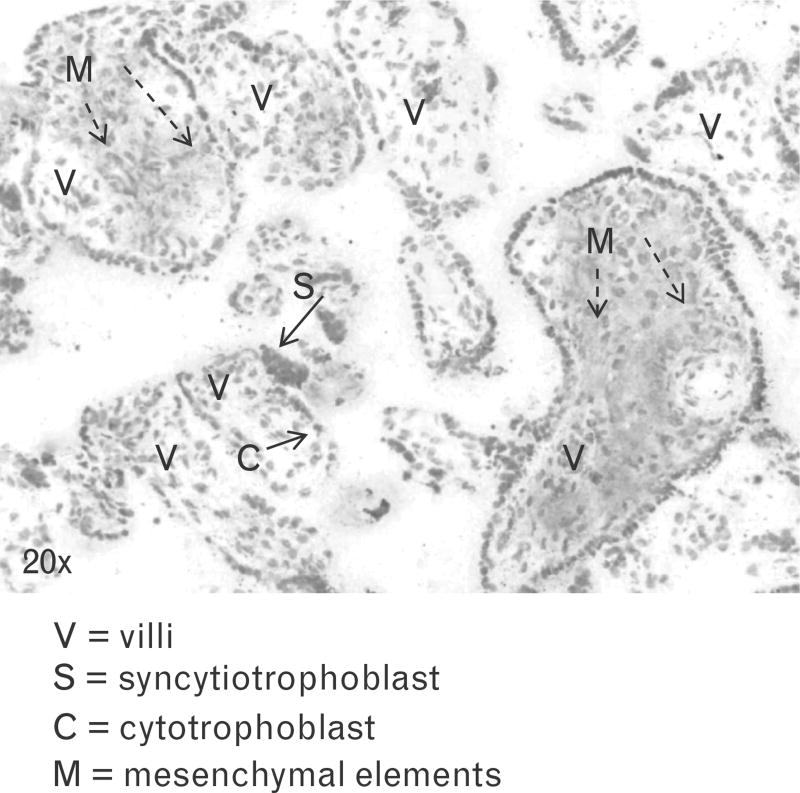
Immunohistochemistry
sEH was observed in the nuclei of mesenchymal elements of the umbilical cord around vessels, and a weak signal was detected in 1–3 cells for each villous of the placenta, with a regular pattern of distribution. CYP2J2 was also detectable in mesenchymal elements of the placenta from both normal and preeclamptic pregnancies (scattered in 10–40% of villi, up to 50%), but not in the umbilical cord. CYP4A11 showed a nonhomogeneous distribution, showing a weak positivity in the mesenchimal axis of sparse villi (up to 50%) and scattered signal in the remaining. Absence of immunostaining was observed in the umbilical cord. CYP2C8 was neither detectable in the placenta nor in the umbilical cord. The analysis of cases vs. controls did not show differences in the distribution of CYP2J2 and sEH after matching images by using an OlympusBX51 optical microscope. Major immunophenotypical findings are summarized in Figs. 2 and 3.
FIGURE 2.
Immunohistochemistry of soluble epoxide hydrolase in the umbilical cord and placenta. Tissue sections of the umbilical cord showing the Warthon’s jelly and one vascular structure at 10× magnification under optical microscope and a tissue section showing intermixed villi from placenta. Soluble epoxide hydrolase immunoexpression was observed in mesenchymal elements of the umbilical cord (arrows M, 20× magnification), and evidenced as weak signal in 1–3 cells per each villous (arrows V, 10× magnification), with an homogeneous pattern of distribution in the placenta (20×).
FIGURE 3.
Immunohistochemistry of cytochrome P450 isoform 2J2 in the placenta of a normotensive woman. Tissue section from placenta showing variable sizes of villi. Morphological details regarding the cytotrophoblast and syncytiotrophoblast (arrows). cytochrome P450 isoform 2J2 was detectable in the mesenchymal elements (arrows M) of placenta (scattered in 10–40%, up to 50% of villi), but not in the umbilical cord (data not shown).
After matching optical glass images vs. scanned clouded-slides, the concordance remained almost perfect (>0.93) for positive immunophenotypical assessment.
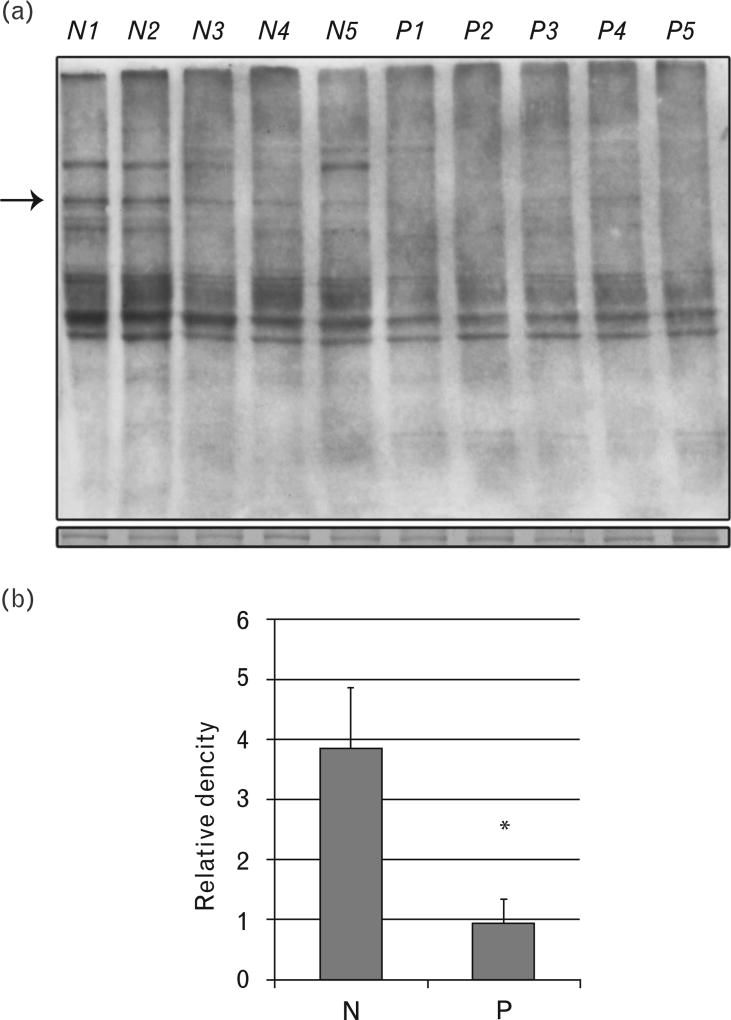
Western blot
In normal and preeclamptic placentas, sEH migrated as a band at a molecular weight of ~60 kDa. The analysis of band intensity showed that the expression of sEH was decreased in preeclamptic as compared with normal placentas (Fig. 4). A statistically significant difference was observed in sEH expression between patients and controls.
FIGURE 4.
Western blot and quantitative analysis of soluble epoxide hydrolase protein expression. Soluble epoxide hydrolase was detected as a band corresponding to a molecular weight of ~60 kDa (a). A few non specific bands were present mainly at low molecular weight. Box plot represents the results of the
DISCUSSION
Major findings from the present study are that all the isoforms of EETs, incorporated in phospholipids of cell membranes in the placenta, are increased in preeclampsia with respect to normotensive women, and that reduced expression of the metabolizing enzyme sEH may account for the observed difference in placental EETs content. The present data extend previous findings of increased EET release in plasma and incorporation in red blood cells of pregnant women with respect to healthy nonpregnant women [11].
Although no statistically significant differences in total plasma EETs levels between preeclampsia and normal pregnancy was observed, Herse and colleagues detected an increase in 5,6-EET and 14,15-EETs cumulated to the corresponding DHETs isomers in preeclampsia [2].
EET concentration was found to be three to fivefold greater in feto-placental than in maternal circulation, particularly in the erythrocytes [11]. This is consistent with the notion that CYP-derived eicosanoids are incorporated in phospholipids of cell membranes, serving as reservoir for circulating bioactive EETs. Previous studies showed the generation and storage of EETs in the placental tissue, with the 5,6-EET as the main isoform, whereas in our sample, all EETs were found to be augmented in preeclampsia [6–9]. Taken together, the present data and previous results indicate a substantial contribution of the feto-placental unit to the release of EETs both in the maternal and the fetal circulation.
Immunochemistry analysis showed that both the enzymes implicated in the synthesis (CYP2J2 and CYP4A11) and in the degradation (sEH) of these lipid mediators are expressed in the placenta of normal pregnant and preeclamptic women. Using a specific mAb, sEH was detected, having a nuclear localization within the mesenchymal cells located in the placental villi. sEH also was localized in the vascular wall of the umbilical cord. To the best of our knowledge, this is the first demonstration of sEH localization in the placenta by immunoistochemistry, whereas previous proteomic studies gave conflicting results, having sEH detected in one study and not in another [13,14]. Expression of sEH mRNA and protein was also found in human umbilical vein after stimulation with angiotensin II in vitro and it has been detected by microarray and serial analysis of gene expression techniques in human placenta, as reported in publically available databases [15,16,17]. Moreover, by immunohistochemistry, sEH was localized in many tissues, including endocrine glands, with a variable intracellular localization being both cytosolic and peroxisomal in some location and exclusively cytosolic in others, such as the endometrium [18,19]. Interestingly, interstitial localization of the enzyme was also observed, as for the retina where glia cells are implicated [20].
Notably, the quantity of sEH by western blot was decreased in preeclampsia. Changes in the overall expression of the enzyme should be related to the observed tendency toward an increased EETs/DHETs ratio in the placenta. This may indicate that lower sEH activity in the placenta could account for the increase in circulating EETs in preeclampsia. Increase in EET biosythesis could also be implicated, as an augmented expression of CYP2J2 mRNA in preeclampsia patients has been observed in previous studies, although no data on protein expression were given [2]. In the present investigation, differences in CYP2J2 distribution could not be clearly identified by immunohistochemistry due to the low level of the signal.
The placenta is ischemic or hypoxemic in preeclampsia. The role of hypoxia, as a stimulus for the production and/or release of EETs, is controversial [21]. Hypoxia activates phospholipases, whereas the promoter regions of several CYP2 genes contain hypoxia-responsive elements, also in cultured human endothelial cells [22–24] suggesting a possible activation of the CYP450 pathway or release of EETs esterified in plasma membranes. Furthermore, sEH expression is markedly downregulated by hypoxia and increased oxidative stress [23,25,26]. In fact, it has been shown that, in mouse lung and liver, as well as in a human hepatoma cell line, Hepatoma 3B, sEH expression is decreased by hypoxia, through a downregulation of its promoter activity [25,26].
Reduced sEH expression in the placenta may therefore have a central role in EET dysregulation and may lead to the accumulation of vasodilatory, proangiogenic EETs within the placenta, which may contribute to placentation and the vascular function in the fetal circulation and may exert compensatory activity toward the vasoconstrictor, antiangiogenic activities that characterize preeclampsia. However, Herse found a different product for at least one of the EET isoforms, the 5,6-EET that is prevalently metabolized through the cyclooxygenase pathway to the thromboxane analogue, 5,6-epoxy-thromboxane A1, a potent vasoconstrictor [3].
In conclusion, increased incorporation of EETs in placenta from preeclamptic women was observed along with reduced expression of sEH, the major EET metabolizing enzyme. When combined with the marked increase of EETs, already observed in the fetal erythrocytes, the present results add information concerning the contribution of the feto-placental unit to the release of EETs in pregnancy and to the dysregulated eicosanoid profile in preeclampsia. A complex network of signals and mediators is implicated in the pathophysiology of preeclampsia: angiotensin II, tumor necrosis factor alpha, antiangiogenetic factors, whereas counteracting systems are impaired: in particular nitric oxide. The present data suggest that EETs generated in the feto-placental unit may have a major role because of their vasodilatory and antiinflammatory actions. It might be speculated that the increase in EETs is part of a protective mechanism, counteracting vasoconstrictor mediators contributing to the ischemia of the placenta. However, considering the relationship between EETs and the vascular abnormalities that characterize preeclampsia, a vasoconstrictor, prohypertensive activity, mediated by EETs or their metabolites, as already shown in the pulmonary and portal circulation, may also be possible.
Supplementary Material
Acknowledgments
This work was supported in part by NIH 34300 mass spectrometry core.
Abbreviations
- 5,6-epTXA1
5,6-epoxy-thromboxane A1
- CYP
cytochrome P450
- CYP2C8
cytochrome P450 isoform 2C8
- CYP2J2
cytochrome P450 isoform 2J2
- CYP4A11
cytochrome P450 isoform 4A11
- DHETs
dihydroxyeicosatrienoic acids
- EETs
epoxyeicosatrienoic acids
- LC–MS/MS
liquid chromatography coupled with tandem mass spectrometry
- NP
normal pregnancy
- PE
preeclampsia
- sEH
soluble epoxide hydrolase
- TNF-alpha
tumor necrosis factor alpha
Footnotes
Conflicts of interest
There are no conflicts of interest.
References
- 1.Young BC, Levine RJ, Karumanchi S. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010;5:173–192. doi: 10.1146/annurev-pathol-121808-102149. [DOI] [PubMed] [Google Scholar]
- 2.Herse F, Lamarca B, Hubel CA, Kaartokallio T, Lokki AI, Ekholm E, et al. Cytochrome P450 subfamily 2J polypeptide 2 expression and circulating epoxyeicosatrienoic metabolites in preeclampsia. Circulation. 2012;126:2990–2999. doi: 10.1161/CIRCULATIONAHA.112.127340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spector AA, Fang X, Snyder GD, Weintraub NL. Epoxyeicosatrienoic acids (EETs): metabolism and biochemical function. Prog Lipid Res. 2004;43:55–90. doi: 10.1016/s0163-7827(03)00049-3. [DOI] [PubMed] [Google Scholar]
- 4.El-Sherbeni AA, El-Kadi AOS. The role of epoxide hydrolases in health and disease. Arch Toxicol. 2014;88:2013–2032. doi: 10.1007/s00204-014-1371-y. [DOI] [PubMed] [Google Scholar]
- 5.Luksha L, Nisell H, Luksha N, Kublickas M, Hultenby K, Kublickiene K. Endothelium-derived hyperpolarizing factor in preeclampsia: heterogeneous contribution, mechanisms, and morphological prerequisites. Am J Physiol Regul Integr Comp Physiol. 2008;294:R510–R519. doi: 10.1152/ajpregu.00458.2007. [DOI] [PubMed] [Google Scholar]
- 6.Patel L, Sullivan MH, Elder MG. Production of epoxygenase metabolite by human reproductive tissues. Prostaglandins. 1989;38:615–624. doi: 10.1016/0090-6980(89)90044-0. [DOI] [PubMed] [Google Scholar]
- 7.Schäfer WR, Zahradnik HP, Arbogast E, Wetzka B, Werner K, Breckwoldt M. Arachidonate metabolism in human placenta, fetal membranes, decidua and myometrium: lipoxygenase and cytochrome P450 metabolites as main products in HPLC profiles. Placenta. 1996;17:231–238. doi: 10.1016/s0143-4004(96)90043-0. [DOI] [PubMed] [Google Scholar]
- 8.Schäfer W, Werner K, Schweer H, Schneider J, Zahradnik HP. Formation of cytochrome P450 metabolites of arachidonic acid by human placenta. Adv Exp Med Biol. 1997;433:411–413. doi: 10.1007/978-1-4899-1810-9_90. [DOI] [PubMed] [Google Scholar]
- 9.Zhang JH, Pearson T, Matharoo-Ball B, Ortori CA, Warren AY, Khan R, et al. Quantitative profiling of epoxyeicosatrienoic, hydroxyeicosatetraenoic, and dihydroxyeicosatetraenoic acids in human intrauterine tissues using liquid chromatography/electrospray ionization tandem mass spectrometry. Anal Biochem. 2007;365:40–51. doi: 10.1016/j.ab.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Minuz P, Jiang H, Fava C, Turolo L, Tacconelli S, Ricci M, et al. Altered release of cytochrome p450 metabolites of arachidonic acid in renovascular disease. Hypertension. 2008;51:1379–1385. doi: 10.1161/HYPERTENSIONAHA.107.105395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang H, McGiff JC, Fava C, Amen G, Nesta E, Zanconato G, et al. Maternal and fetal epoxyeicosatrienoic acids in normotensive and preeclamptic pregnancies. Am J Hypertens. 2013;26:271–278. doi: 10.1093/ajh/hps011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li L, Li N, Pang W, Zhang X, Hammock BD, Ai D, et al. Opposite effects of gene deficiency and pharmacological inhibition of soluble epoxide hydrolase on cardiac fibrosis. PLoS One. 2014;9:e94092. doi: 10.1371/journal.pone.0094092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilhelm M, Schlegl J, Hahne H, Moghaddas Gholami A, Lieberenz M, Savitski MM, et al. Mass-spectrometry-based draft of the human proteome. Nature. 2014;509:582–587. doi: 10.1038/nature13319. [DOI] [PubMed] [Google Scholar]
- 14.Kim M-S, Pinto SM, Getnet D, Nirujogi RS, Manda SS, Chaerkady R, et al. A draft map of the human proteome. Nature. 2014;509:575–581. doi: 10.1038/nature13302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ai D, Fu Y, Guo D, Tanaka H, Wang N, Tang C, et al. Angiotensin II upregulates soluble epoxide hydrolase in vascular endothelium in vitro and in vivo. Proc Natl Acad Sci USA. 2007;104:9018–9023. doi: 10.1073/pnas.0703229104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boon K, Osorio EC, Greenhut SF, Schaefer CF, Shoemaker J, Polyak K, et al. An anatomy of normal and malignant gene expression. Proc Natl Acad Sci USA. 2002;99:11287–11292. doi: 10.1073/pnas.152324199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu C, Orozco C, Boyer J, Leglise M, Goodale J, Batalov S, et al. BioGPS: an extensible and customizable portal for querying and organizing gene annotation resources. Genome Biol. 2009;10:R130. doi: 10.1186/gb-2009-10-11-r130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Enayetallah AE, French RA, Barber M, Grant DF. Cell-specific subcellular localization of soluble epoxide hydrolase in human tissues. J Histochem Cytochem. 2006;54:329–335. doi: 10.1369/jhc.5A6808.2005. [DOI] [PubMed] [Google Scholar]
- 19.Enayetallah AE, French RA, Grant DF. Distribution of soluble epoxide hydrolase, cytochrome P450 2C8, 2C9 and 2J2 in human malignant neoplasms. J Mol Histol. 2006;37:133–141. doi: 10.1007/s10735-006-9050-9. [DOI] [PubMed] [Google Scholar]
- 20.Hu J, Popp R, Frömel T, Ehling M, Awwad K, Adams RH, et al. Müller glia cells regulate Notch signaling and retinal angiogenesis via the generation of 19,20-dihydroxydocosapentaenoic acid. J Exp Med. 2014;211:281–295. doi: 10.1084/jem.20131494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fan F, Muroya Y, Roman RJ. Cytochrome P450 eicosanoids in hypertension and renal disease. Curr Opin Nephrol Hypertens. 2015;24:37–46. doi: 10.1097/MNH.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boutilier RG. Mechanisms of cell survival in hypoxia and hypothermia. J Exp Biol. 2001;204:3171–3181. doi: 10.1242/jeb.204.18.3171. [DOI] [PubMed] [Google Scholar]
- 23.Fleming I. The pharmacology of the cytochrome P450 epoxygenase/ soluble epoxide hydrolase axis in the vasculature and cardiovascular disease. Pharmacol Rev. 2014;66:1106–1140. doi: 10.1124/pr.113.007781. [DOI] [PubMed] [Google Scholar]
- 24.Michaelis UR, Fisslthaler B, Barbosa-Sicard E, Falck JR, Fleming I, Busse R. Cytochrome P450 epoxygenases 2C8 and 2C9 are implicated in hypoxia-induced endothelial cell migration and angiogenesis. J Cell Sci. 2005;118:5489–5498. doi: 10.1242/jcs.02674. [DOI] [PubMed] [Google Scholar]
- 25.Keserü B, Barbosa-Sicard E, Schermuly RT, Tanaka H, Hammock BD, Weissmann N, et al. Hypoxia-induced pulmonary hypertension: comparison of soluble epoxide hydrolase deletion vs. inhibition. Cardiovasc Res. 2010;85:232–240. doi: 10.1093/cvr/cvp281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oguro A, Sakamoto K, Suzuki S, Imaoka S. Contribution of hydrolase and phosphatase domains in soluble epoxide hydrolase to vascular endothelial growth factor expression and cell growth. Biol Pharm Bull. 2009;32:1962–1967. doi: 10.1248/bpb.32.1962. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.