Abstract
Introduction
In India, there are approximately 41 million diabetics to date. Impaired glucose tolerance or pre-diabetes may occur as early as adolescence.
Objective
To find out the cut-off values of body mass index (BMI) and waist circumference to predict pre-diabetes in adolescents in north India.
Methods
A cross-sectional study was conducted among 526 students aged 17–19 years, in the Institute of Paramedical Sciences, Chatrapati Shahuji Maharaj University, Kanpur. A pre-tested questionnaire was used and the diagnostic criteria of the American Diabetic Association were applied. Receiver operating characteristic(ROC) analysis was used to assess the cut-offs of BMI and waist circumference for predicting prediabetes.
Results
ROC analysis showed that BMI is a good predictor of prediabetes for both boys and girls.Area under the ROC curve was 0.828 for boys and 0.838 for girls, respectively. The cut-off values of BMI for predicting prediabetes were identified as ≥22.8 kg/m2 in boys and ≥20.5 kg/m2 in girls. Upon ROC analysis for waist circumference, it was observed that it was a good predictor of prediabetes both for boys (area under the curve 0.804) and girls (area under the curve 0.795). The cut-offs for waist circumference for predicting prediabetes were found to be ≥82.5 cm for boys and ≥80.3 cm for girls.
Conclusion
BMI and waist circumference estimation can be done for early detection of prediabetes in adolescents for further diagnostic evaluation and management.
Keywords: Adolescents, Cut-off, BMI, Waist circumference, Pre-diabetes
1. Introduction
Diabetes mellitus is a metabolic disorder defined by chronic hyperglycemia with deranged fat, carbohydrate and protein metabolism that results from improper secretion or action of insulin.1 It is a modern day epidemic. The WHO Global Report on Diabetes has revealed that the number of adult diabetics in the world was 422 million in 2014 in comparison to 108 million in 1980.2 The age standardized prevalence of diabetes has become 8.5% in the adult population, almost double that of the 4.7% in 1980. More than 80% of deaths due to diabetes occur in middle and low income countries.3, 4 WHO estimates that diabetes will become the seventh most common cause of mortality, worldwide, in the year 2030.5
India is the diabetes capital of the world because there are around 41 million Indians suffering from diabetes till date and every fifth person in world, having diabetes, is an Indian.6, 7 Recent studies have revealed that the occurrence of diabetes mellitus is increasing among children and adolescents in India.8, 9, 10 Screening for glucose intolerance in all children and adolescents is not recommended in the current scenario, however it is recommended in high-risk populations.11
There are two main types of diabetes mellitus (DM):Type 1 DM results from the inability of the pancreas to produce enough insulin. Its cause is unknown.12 Type 2 DM occurs due to insulin resistance, in which the peripheral cells fail to respond to insulin properly. As the disease progresses, failure to produce insulin may also occur. The most common risk factor of type 2 DM is excessive body weight and sedentary lifestyle. Type 2 DM accounts for more than 90% of the diabetes cases worldwide. It is difficult to diagnose early, as it is mostly asymptomatic and usually presents with complications like nephropathy, cardiovascular disease, retinopathy, neuropathy, cerebrovascular disease and peripheral vascular disease.12 It can go undetected for 9–12 years and, consequently, present with complications.13
Recent studies have revealed that around half of the diabetics in the world are undiagnosed.12 American Diabetic Association has introduced a new category of blood glucose levels, preceding the onset of diabetes, known as prediabetes. Individuals with prediabetes, have a higher risk of development of diabetes in the future.14 American Diabetic Association has defined pre-diabetes as − Impaired Fasting Glucose, when fasting plasma glucose level ranges from 100 to 125 mg/dl and Impaired Glucose Tolerance, when plasma glucose level 2-h after an oral glucose tolerance test ranges from 140 to 199 mg/dl.15, 16 Screening for prediabetes can lead to early diagnosis and treatment and prevention of complications.15
Keeping in view that the onset of glucose intolerance can occur in the adolescent age group and that early diagnosis can prevent grave complications of diabetes, it is the need of the hour to identify those adolescents who are at risk. Since very few studies have been conducted among Indian adolescents, this study was planned to find out the cut-off values of BMI nd waist circumference for predicting pre-diabetes in adolescents in the Indian population.
2. Material and methods
2.1. Study design and sample size
A cross-sectional study was conducted with a minimum sample size of 506, calculated by taking the prevalence of glucose intolerance among adolescents as 28.2%, as observed in the ICMR-INDIAB study.17
Sample size was estimated using the formula, N = Z(1-α/2)2pq/d2; where α was taken at 5% level of significance; p = prevalence of glucose intolerance = 28.2%; q = 100-p = 71.8%; and d = margin of error = 4%. Therefore, the minimum sample size obtained was 506.
2.2. Sampling
The study setting was the Institute of Paramedical Sciences,affiliated to Chatrapati Shahuji Maharaj University, Kanpur. The Institute offers a course of 4 years in Paramedical Sciences
and admits around 150 students in a year. All the students enrolled in the Institute in all 4 years were enlisted. All students who were present on the day of the interview and willing to be included in the study were selected. Written informed consent was taken from the students as well as from their parents/guardians. Ethical clearance was taken from the Institutional Ethical Committee. The data was analyzed for 526 subjects. Among the study subjects there were 277 boys and 249 girls, aged between 17 and 19 years.
2.3. Methodology
Data was recorded on a pre-designed and pre-tested questionnaire and data was collected regarding the following variables: age, socioeconomic status, family history of diabetes, physical activity, dietary pattern, weight, height, BMI and waist circumference. Fasting blood samples were collected on the day following the day of interview. A 10 ml blood sample was collected from each subject: 4 ml in EDTA tube and 6 ml in plain tube. The samples were taken to the laboratory in the Deptt. of Biochemistry, Chatrapati Shahuji Maharaj University, Kanpur and were centrifuged. Glucose levels were estimated. Enzymatic colorimetric GOD − PAP method was used to estimate fasting plasma glucose.
Subjects were classified as normoglycemic or hyperglycemic using the diagnostic criteria of the American Diabetic Association (ADA). Subjects with fasting plasma glucose level <100 mg/dl (after fasting for 8 h) were classified as normoglycemic, those with fasting plasma glucose level between 100 and 125 mg/dl were classified as prediabetic and those with fasting plasma glucose level ≥126 mg/dl were classified as diabetic.15
To measure body weight, the subject was made to stand motionless on Krup’s weighing machine(least count 0.5 kg). The scale was calibrated to zero before every reading. To measure height, the subject was made to stand in an erect position against a vertical surface, and the head stationed such that the upper margin of the external auditory meatus was in line with the inferior margin of the bony orbit. A hard board was held vertical to the wall, just over the head, height was marked on the wall and was measured with a measuring tape (least count 0.5 cm). Waist circumference was estimated, at the level of the umbilicus, keeping the subject in an erect position, breathing normally.
Physical activity was estimated as increments in BMR. In the present study, the subject’s BMR factor was calculated by questioning him/her about the type of activity and time spent in each activity in the last 24 h.18 Average daily level of activity was classified as sedentary, moderate or heavy, expressed as a multiple of BMR as follows:
| Gender | Sedentary | Moderate | Heavy |
| Boys | 1.55 | 1.78 | 2.10 |
| Girls | 1.55 | 1.64 | 1.82 |
2.4. Statistical analysis
Microsoft Excel and MedCalc12.7.5were used to compile and analyse the data, respectively. Receiver operating characteristic(ROC) analysis was done to estimate the predictive validity, and to calculate the cut-offs of BMI and waist circumference. Area under the curve was estimated to analyse the diagnostic power of the test, and to assess the probability that the anthropometric indices would identify subjects with pre-diabetes. Cut-offs were estimated by measuring the sensitivity and specificity of the anthropometric measurements at different cut-off points. Youden index method was used to identify the associated criterion providing maximum sensitivity and specificity to predict pre-diabetes.
3. Results
The study was conducted on 526 subjects, 277 boys and 249 girls. The mean age of boys was 18.5 ± 1.5 years and the mean age of girls was 17.9 ± 1.8 years. (Table 1). Average BMI of the study subjects was 22.0 ± 3.5 kg/m2 in boys and 20.8 ± 4.1 kg/m2 in girls. The mean waist circumference of boys was 80.2 ± 15.3 cm and that of girls was 72.9 ± 17.5 cm. Average fasting blood glucose level of the study population was 92.9 ± 12.4 mg/dl and 87.9 ± 14.8 mg/dl among boys and girls respectively.Prevalence of prediabetes among the study subjects was 32.1% and that of diabetes was 0.8%.None of the subjects had previously diagnosed Type 1 or Type 2 diabetes mellitus.
Table 1.
Characteristics of the study population.
| Parameter | Boys(N = 277) |
Girls(N = 249) |
||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age | 18.5 | 1.5 | 17.9 | 1.8 |
| Weight | 59.9 | 10.2 | 49.4 | 10.1 |
| Height | 164.9 | 7.9 | 154.1 | 5 |
| BMI | 22 | 3.5 | 20.8 | 4.1 |
| Waist | 80.2 | 15.3 | 72.9 | 7.5 |
| circumference | ||||
| Fasting blood | 92.2 | 12.4 | 87.9 | 14.8 |
| glucose | ||||
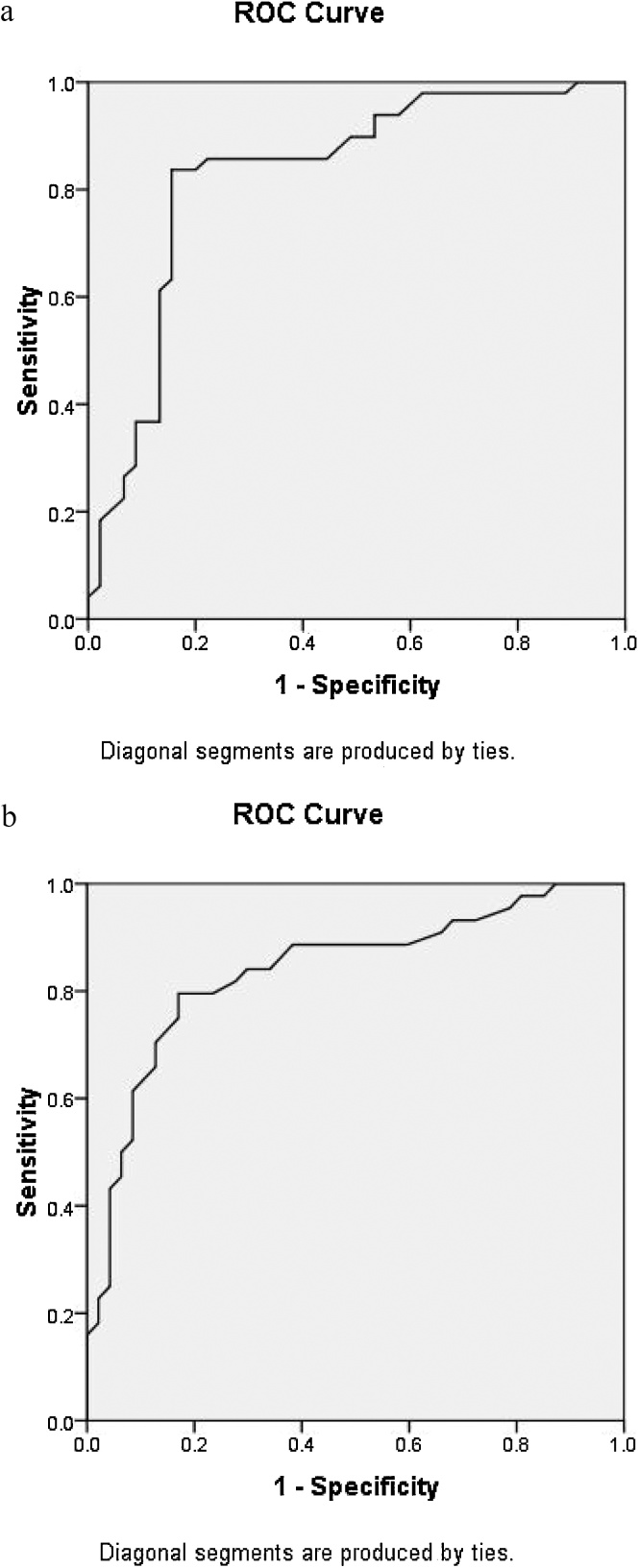
The ROC analysis for BMI showed good predictive power for pre-diabetes for both boys and girls. Area under the curve was 0.828 for boys and 0.838 for girls, respectively. (Fig. 1a and b) The cut-offs of BMI to predict prediabetes were calculated as ≥22.8 kg/m2 in boys and
Fig. 1.
(a) BMI as predictor of pre-diabetes in adolescent boys.
ROC analysis revealed that area under the ROC curve was 0.828 for boys. The cut-off value of BMI for predicting prediabetes was identified as ≥22.8 kg/m2 in boys
(b) BMI as predictor of pre-diabetes in adolescent girls.
ROC analysis revealed that area under the ROC curve was 0.838 for girls, respectively. The cut-off value of BMI for predicting prediabetes was identified as ≥20.5 kg/m2 in girls.
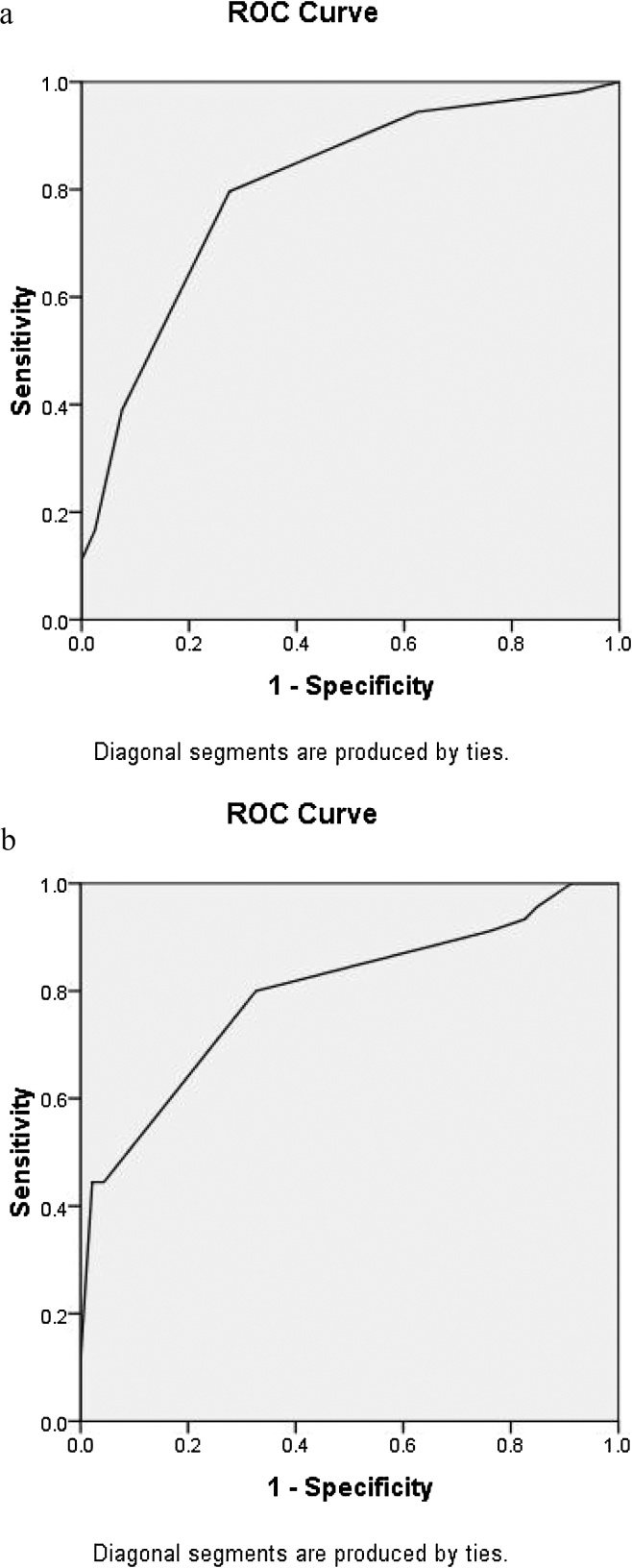
≥20.5 kg/m2 in girls. ROC analysis for waist circumference also revealed that it was a good discriminator of prediabetes both for boys (area under the curve 0.804) and girls (area under the curve 0.795). (Fig. 2a and b). The cut-offs for waist circumference to predict prediabetes were calculated as ≥82.5 cm for boys and ≥80.3 cm for girls. The sensitivity and specificity of the cut-off for BMI in boys was 73.1% and 95.3% respectively, and the same in girls was 70.8% and 94.6%, respectively. The sensitivity and specificity of the cut-off for waist circumference in boys was 75.3% and 92.4% respectively, and the same in girls was 72.7% and 94.8% respectively. Adolescents with raised BMI or increased waist circumference had a greater prevalence of prediabetes.
Fig. 2.
(a) Waist circumference as predictor of pre-diabetes in adolescent boys.
ROC analysis for waist circumference showed that it was a good predictor of prediabetes for boys −area under the ROC curve 0.804. The cut-off for waist circumference for predicting prediabetes was estimated as ≥82.5 cm for boys.
(b) Waist circumference as predictor of pre-diabetes in adolescent girls.
ROC analysis for waist circumference showed that it was a good predictor of prediabetes for girls − area under the ROC curve 0.795.The cut-off for waist circumference for predicting prediabetes was estimated as ≥80.3 cm for girls.
Multiple logistic regression analysis of the determinants of pre-diabetes showed that BMI,waist circumference and physical activity were significantly associated with pre-diabetes in adolescents. For every 1 kg/m2 increase in BMI, there was a 1.067 times increased risk of pre-diabetes and for every 1 cm increase in waist circumference, there was a 1.028 times higher risk of pre-diabetes. The risk of developing pre-diabetes was higher in sedentary worker and decreased in moderate and heavy workers. There was no significant association between pre-diabetes and age, family history of diabetes and dietary pattern (Table 2).
Table 2.
Multiple logistic regression analysis of determinants of pre-diabetes.
| Determinants | β | SE | OR | 95% CI:Lower limit of OR | 95% CI:Upper limit of OR | P value |
|---|---|---|---|---|---|---|
| Age(per year) | 0.071 | 0.044 | 1.074 | 0.986 | 1.170 | 0.102 |
| BMI(per kg/m[2]) | 0.065 | 0.018 | 1.067 | 1.031 | 1.105 | <0.001 |
| Waist Circumference(per cm) | 0.028 | 0.008 | 1.028 | 1.013 | 1.044 | <0.001 |
| Physical activity(0 = Sedentary,2 = Moderate worker, 2 = Heavy worker) | −0.875 | 0.203 | 0.417 | 0.280 | 0.620 | <0.001 |
| Family history of diabetes (0 = Absent,1 = Present) | 0.059 | 0.045 | 1.061 | 0.971 | 1.159 | 0.191 |
| Dietary pattern (0 = Vegetarian,1 = Non-vegetarian) | 0.062 | 0.063 | 1.064 | 0.941 | 1.203 | 0.32 |
4. Discussion
The present study revealed that the prevalence of prediabetes was 32.1% and that of diabetes was 0.8% among the study subjects. A study conducted in USA revealed that 21% of the adolescents with obesity, between the age of 11 and 18 years, had impaired glucose tolerance as estimated by measuring the blood glucose level 2 h after an oral glucose tolerance test(OGTT).19 Another study from Bangladesh showed that around 20% subjects between the age of 11 and 18 years, having a BMI more than 95th percentile of age and gender according to CDC, had impaired glucose tolerance two hours after an OGTT.20 The variation from the present study may be due to the different criteria being used for estimating glucose intolerance as we have measured fasting plasma glucose levels, whereas the other studies have assessed the plasma glucose levels two hours following OGTT. In the ICMR-INDIAB study, the weighted prevalence of diabetes was 10.4% in Tamil Nadu, 8.4% in Maharashtra, 5.3% in Jharkhand and 13.6% in Chandigarh and the prevalence of prediabetes in these states was 8.3%, 12.8%, 8.1% and 14.6%, respectively.17 The difference from the present study may be because of the fact that the ICMR study included the adult population which was more prone to full blown diabetes.
In the present study, the cut-off value of BMI for predicting prediabetes was ≥22.8 kg/m2 in boys and ≥20.5 kg/m2 in girls.World Health Organization reported that the Asian population had a varied association between BMI, body fat percentage and health hazards than their
counterparts in the West.21 It is proposed that at BMIs lesser than the WHO cut-off for overweight (25 kg/m2), the percentage of Asian population with a greater risk of type 2 diabetes and cardiovascular disease was higher than that in the West. However, studies have not mentioned an exact BMI cut-off point for the Asian population. In different Asian populations, the cut-off for moderate risk varies from 22 kg/m2 to 25 kg/m2, whereas that for high risk ranges from 26 kg/m2 to 31 kg/m2.21 Cut-off points have not be defined separately for different population groups. In another study, it was observed that South Asian, Chinese, and black populations developed diabetes at a higher rate, in younger age groups, and at BMI values that were significantly lower than the western populations. Their results highlighted the fact that there was room for determining individualized prevention strategies and for redefining population-wise cut-offs for non-white populations.22
In our study, the ROC analysis for waist circumference showed that the cut-offs for waist circumference to predict prediabetes were calulated as ≥82.5 cm for boys and ≥80.3 cm for girls. In another Indian study, receiver operator characteristic curve analysis of waist circumference cut-offs for males was 90 cm with a sensitivity and specificity of 71% and 96%, respectively, and for females was 85 cm with a sensitivity and specificity of 86% and 93%, respectively, having a positive association with metabolic syndrome.23 However, these findings were observed in adults and no similar studies among adolescents are available. In the present study, multiple logistic regression analysis revealed that BMI,waist circumference and physical activity were significantly associated with pre-diabetes in adolescents, even after acounting for other confounding factors.
The highlighting feature of this study is that the BMI cut-off for predicting prediabetes is ≥22.8 kg/m2 in boys and ≥20.5 kg/m2 in girls, which is substantially lower than that recommended by WHO as 25 kg/m2, therefore we need to rethink and redefine the criteria for normal BMI for the Indian population so as to prevent the occurrence of diabetes and its complications.
One limitation of the present study was that the classification of diabetes was done on the basis of a single measurement of fasting blood glucose level. Oral gluose tolerance test (OGTT) and HbA1c estimation could not be done, so few subjects without impaired fasting glucose but having impaired gluose tolerance may have been missed.
Very few studies have been conducted on glucose intolerance among Indian adolescents. The findings of this study are important as they provide anthropometric cut-offs to identify high risk adolescents in the Indian population who should be screened for glucose intolerance. The National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke envisages to address the problem of chronic non-communicable diseases(NCDs) like cancer, diabetes, CVDs and stroke through early diagnosis, treatment and follow up by setting up of NCD clinics. Another component of the programme is to provide support for diagnosis and cost effective treatment at primary, secondary and tertiary levels of health care. The results of the present study can be used formulate guidelines to decide the cutoffs of anthropometric indicators to identify adolescents to be screened for glucose intolerance at the primary and secondary levels. In a resource poor country like India, where health professionals are not available at the grass root level, simple, cost effective anthropometric indicators will be very useful for screening of glucose intolerance as these can be easily and effectively used by the peripheral health workers like ASHAs and ANMs.
5. Conclusion
In conclusion, it can be said that BMI and waist circumference are easy-to-use tools that can be applied for screening of pre-diabetes in adolescents. Since the beginning of non-communicable diseases like diabetes can be traced to childhood and adolescence, early diagnosis and timely management can go a long way to prevent the morbidity and mortality arising as a consequence of the disease.
Sources of funding
None.
Conflict of interest
None.
References
- 1.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diab Care. 2004;27(Suppl. 1):S5–S10. doi: 10.2337/diacare.27.2007.s5. [PMID. 14693921] [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization: Global Report on Diabetes. http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf (Accessed 18, January 2017).
- 3.Danaei G., Finucane M.M., Lu Y. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [PMID 21705069] [DOI] [PubMed] [Google Scholar]
- 4.Global health risks . World Health Organization; Geneva: 2009. Mortality and burden of disease attributable to selected major risks. [Google Scholar]
- 5.Mathers C.D., Loncar D. Projections of global mortality and burden of diseasefrom 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [PMID 17132052] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joshi S.R., Parikh R.M. India-Diabetes capital of the world: now heading towards hypertension. J Assoc Phys India. 2007;55:323–324. [PMID. 17844690] [PubMed] [Google Scholar]
- 7.Sahay B.K. API-ICP guidelines on diabetes 2007. J Assoc Phys India. 2007;55:1–50. [Google Scholar]
- 8.Molnar D. The prevalence of metabolic syndrome and type 2 diabetes mellitus in children and adolescents. Int J Obes Relat Metab Disord. 2004;28(Suppl. 3):S70–S74. doi: 10.1038/sj.ijo.0802811. [DOI] [PubMed] [Google Scholar]
- 9.Amutha A., Datta M., Unnikrishnan R., Anjana R.M., Mohan V. Clinical profile and complications of childhood and adolescent onset type 2 diabetes seen at a diabetes centre in South India. Diab Technol Ther. 2012;14:497–504. doi: 10.1089/dia.2011.0283. [DOI] [PubMed] [Google Scholar]
- 10.Amutha A., Manjula D., Unnikrishnan I.R. Clinical profile of diabetes in the young seen between 1992 and 2009 at a specialist diabetes centre in South India. Prim Care Diab. 2011;5:223–229. doi: 10.1016/j.pcd.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 11.American diabetes association: type 2 diabetes in children and adolescents. Diab Care. 2000;23:381–389. doi: 10.2337/diacare.23.3.381. [DOI] [PubMed] [Google Scholar]
- 12.Rev. 2nd ed. Jaypee Brothers Medical Publishers; New Delhi: 2012. RSSDI textbook of diabetes mellitus. [p. 235] [Google Scholar]
- 13.Roche M.M., Wang P.P. Factors associated with a diabetes diagnosis and late diabetes diagnosis for males and females. J Clin Transl Endocrinol. 2014;3(1):77–84. doi: 10.1016/j.jcte.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Praveen P.A., Roy A., Prabhakaran D. Cardiovascular disease risk factors: a childhood perspective. Ind J Pediatr. 2013;80(Suppl. 1):S3–12. doi: 10.1007/s12098-012-0767-z. Epub 2012 May 27.[PMID. 22638996] [DOI] [PubMed] [Google Scholar]
- 15.Expert committee on the diagnosis and classification of diabetes mellitus of the american diabetes association. Diab Care. 2005;28:S4–S36. [Google Scholar]
- 16.http://care.diabetesjournals.org/content/39/Supplement_1/S13 (last accessed on 9th July 2017).
- 17.Anjana R.M., Pradeepa R., Deepa M., Datta M., Sudha V., Unnikrishnan R. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes(ICMR-INDIAB) study. Diabetologia. 2011;54(12):3022–3027. doi: 10.1007/s00125-011-2291-5. [Epub 2011 Sep 30] [DOI] [PubMed] [Google Scholar]
- 18.Report of a Joint WHO/FAO/UNU Expert Consultation, 1985.
- 19.Sinha R., Fisch G., Teague B. Prevalence of impaired glucose tolerance among children and adolescents with mar ked obesity. N Engl J Med. 2002;346(11):802–810. doi: 10.1056/NEJMoa012578. [PMID. 11893791] [DOI] [PubMed] [Google Scholar]
- 20.Mohsin F., Mahbuba S., Begum T., Azad K., Nahar N. Prevalence of impaired glucose tolerance among children and adolescents with obesity. Mymensingh Med J. 2012;21(4):684–690. [PMID. 23134918] [PubMed] [Google Scholar]
- 21.WHO Expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 22.Chiu M., Austin P.C., Manuel D.G., Shah B.R., Tu J.V. Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diab Care. 2011;34(8):1741–1748. doi: 10.2337/dc10-2300. [Epub 2011 Jun 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pratyush D.D., Tiwari S., Singh S., Singh S.K. Waist circumference cutoff and its importance for diagnosis of metabolic syndrome in Asian Indians: a preliminary study. Ind J Endocrinol Metab. 2012;16(1):112–115. doi: 10.4103/2230-8210.91205. [DOI] [PMC free article] [PubMed] [Google Scholar]