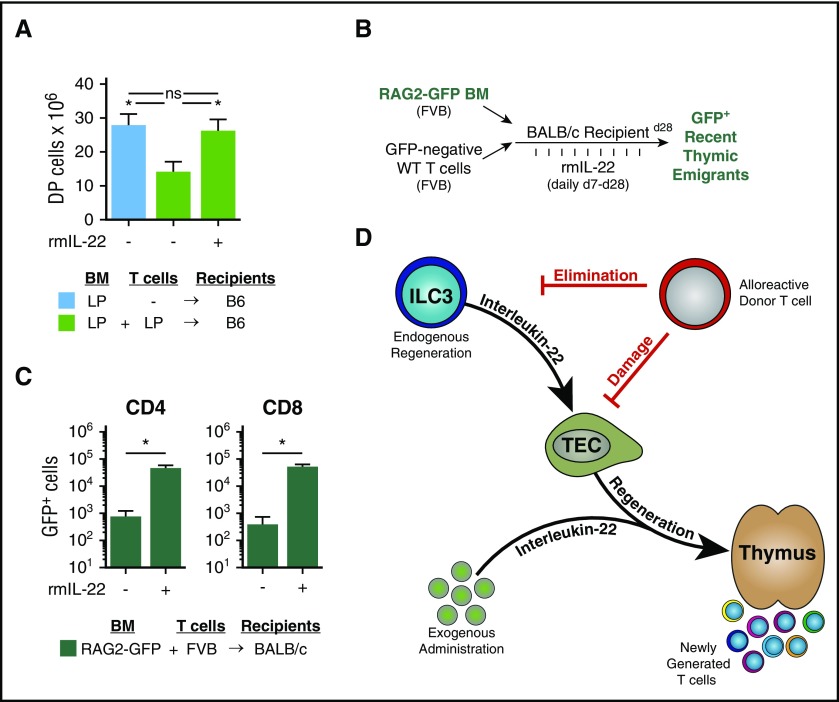
Figure 6.
Exogenous administration of IL-22 improves thymopoiesis and T-cell reconstitution after allo-BMT. (A) WT B6 recipients (H-2b) were transplanted with LP TCD BM (H-2b; 5 × 106) and WT LP T cells (4 × 106) (n = 9-10 recipients per group). GVHD mice were treated once per day with either phosphate-buffered saline (PBS) or rmIL-22 (200 mg/kg) starting on day 7 post-BMT; CD4+CD8+ DP thymocytes were assessed 3 weeks post-BMT. (B) Experimental model of FVB→BALB/c BMT (H-2q→H-2d) with RAG2-GFP marrow to evaluate thymic export of donor marrow–derived new peripheral T cells after IL-22 treatment. (C) BALB/c mice were transplanted with 5 × 106 RAG2-GFP (FVB background) TCD BM cells and 0.1 × 106 FVB T cells. Recipient mice (n = 5 per group) were treated once per day with either PBS or rmIL-22 (200 mg/kg) starting on day 7 post-BMT, and GFP+ T cells were enumerated in the spleen at 28 days post-BMT. (D) Thymic injury and depletion of thymocytes trigger ILC3 production of IL-22, which acts directly on TECs to induce their proliferation and survival. Through this trophic effect on TECs, IL-22 can promote endogenous immune regeneration. During GVHD, alloreactive T cells eliminate ILCs, thereby abrogating their production of IL-22 and impairing IL-22–mediated recovery of thymic epithelium. Administration of exogenous recombinant IL-22 can circumvent the loss of ILCs to enhance thymopoiesis and improve immune reconstitution after allo-BMT. Bar graphs represent mean ± SEM. *P < .05.