REPLY
Tantibhedhyangkul et al. speculate that the data presented in our recent study (1) may have been influenced by Mycoplasma sp. contaminating the Karp strain of Orientia tsutsugamushi.
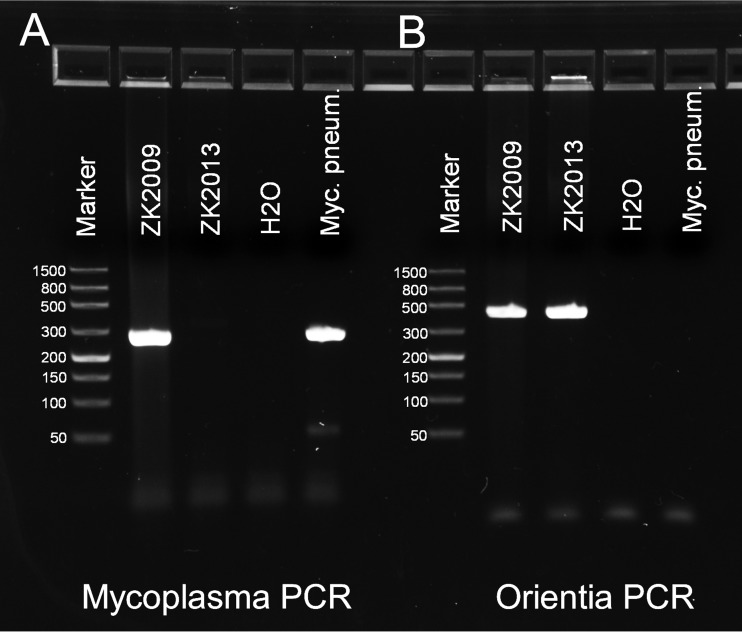
They raise attention to a relevant point that was addressed by us before the Toll-like receptor 2 (TLR2) study was conducted. The O. tsutsugamushi Karp strain, which we obtained from the Australian Rickettsial Reference Laboratory, was propagated and tested for the presence of mycoplasma DNA in the preparatory phase of the study, using a Mycoplasma sp. 16S-specific PCR (2). This PCR yielded a positive result for mycoplasma, as demonstrated from a reference sample (Fig. 1A, sample ZK2009). Sequencing revealed the highest homology of the amplicon with Mycoplasma orale. As shown in Fig. 1B, the presence of Orientia DNA in the sample was verified by using an Orientia-specific PCR targeting the 56-kDa protein-encoding gene (3).
FIG 1.
Decontamination of O. tsutsugamushi Karp from Mycoplasma sp. by mouse passage before the study of TLR2 involvement by Gharaibeh et al. O. tsutsugamushi Karp was propagated in L929 mouse fibroblasts (ZK2009). To decontaminate the strain from Mycoplasma sp., it was inoculated i.p. into a BALB/c mouse, reisolated from the spleen in L929 cell culture, and continuously propagated (ZK2013). DNA was prepared from reference samples ZK2009 and ZK2013 that had been stored at −20°C or Mycoplasma pneumoniae as a positive control (EZ1; Qiagen, Hilden, Germany) and eluted in 60 μl of AVE buffer (Qiagen). (A) A mycoplasma-specific PCR was run with the GPO-3/MGSO primer pair (MGSO, 5′-TGCACCATCTGTCACTCTGTTAACCTC-3′; GPO-3, 5′-GGGAGCAAACAGGATTAGATACCCT-3′) (2). The reaction mixture contained, in a total reaction volume of 25 μl, 5 μl of template, 400 nM GPO-3, 200 nM MGSO (both from MWG-Biotech, Ebersberg, Germany), 0.2 mM deoxynucleoside triphosphates, and 0.5 U of HotStarTaq DNA polymerase (Qiagen, Hilden, Germany). The cycling protocol was 94°C for 15 min; 35 cycles of 94°C for 20 s, 58°C for 30 s, and 72°C for 30 s; and 72°C for 7 min. (B) To detect O. tsutsugamushi-specific DNA, a PCR targeting a 409-bp fraction of the 56-kDa protein-encoding gene with the primer pair OtsuF/OtsuR was used (OtsuF, 5′-AATTGCTAGTGCAATGTCTG-3′; OtsuR, 5′-GGCATTATAGTAGGCTGAG-3′) (3). The reaction mixture contained, in a total reaction volume of 25 μl, 2 μl of template, 400 nM OtsuF, 400 nM OtsuR (both from TIB MOLBIOL, Berlin, Germany), 0.2 mM deoxynucleoside triphosphates, and 0.5 U of HotStarTaq DNA polymerase (Qiagen, Hilden, Germany). The cycling protocol was 94°C for 15 min; 40 cycles of 94°C for 20 s, 58°C for 30 s, and 72°C for 30 s; and 72°C for 7 min. Amplification products were visualized on a 2.2% agarose gel (Lonza, Basel, Switzerland). The values to the left of the marker lanes are molecular sizes in kilodaltons.
To purify the pathogenic Orientia strain contaminated with mycoplasma, we conducted a mouse passage, as was later suggested and discussed by Ogawa et al. (4). The strain was inoculated intraperitoneally (i.p.) into a female BALB/c mouse and reisolated from spleen homogenates taken during the acute infection phase. From then on, Orientia cell culture samples consistently tested negative by mycoplasma PCR, as shown by a representative sample from the end of the project phase (Fig. 1A, sample ZK2013). We thus exclude the possibility that our results were influenced by the presence of mycoplasma lipoproteins.
With regard to the fact that Mycoplasma spp. provide potent lipopeptide ligands for TLR2, e.g., macrophage-activating lipopeptide 2 (5), it is little surprising that Tantibhedhyangkul et al. found increased TLR2-dependent responses when using them to spike Orientia cultures. However, the authors neither experimentally addressed nor discussed other reasons for their failure to reproduce our findings. Specifically, they did not include heat-inactivated mycoplasma in their experiments to test their own hypothesis that “bacterial lysis and the subsequent release of more lipopeptides into the extracellular milieu” could induce a stronger inflammatory response in mouse dendritic cells. Additionally, we reported that the TLR2 ligand was, inter alia, proteinase K sensitive, unlike the synthetic lipopeptide Pam3Cys (1). Since digestion of lipoproteins with proteinase K preserves TLR2-ligating ability (6), this finding cannot be reconciled with mycoplasma lipoprotein contamination.
Moreover, Tantibhedhyangkul et al. claim that live Orientia bacteria generally induce higher levels of cytokines in monocytes and macrophages than inactivated organisms do (7, 8). This is in contrast not only to our data (1) but also to previous work that demonstrated increased production of tumor necrosis factor alpha (TNF-α) and interleukin-6 by murine macrophages that were stimulated with heat-killed Orientia organisms rather than infected with live Orientia organisms (9). A reason that could explain the authors' failure to observe downregulation of inflammatory responses by live Orientia bacteria may be the exclusive use of very high multiplicities of infection (MOIs) of >50 to 1,000/cell. A recent work by Tsai et al. showed that small infection doses (MOIs of <20) suppress TNF-α production, while larger doses (MOIs of >20 to 1,000) are strong inducers of TNF-α (10). Thus, the experimental conditions selected by Tantibhedhyangkul et al.—a restricted range of MOIs and no investigation of inactivated organisms—may have precluded the detection of TLR2-dependent recognition of Orientia. Instead, other recognition pathways may have become more relevant upon infection with high MOIs, associated with active suppression of all TLR2-mediated signals.
The authors were furthermore concerned about the timing of cytopathic effects. We do observe the onset of cytopathic effects in Orientia-infected L929 cell cultures between days 7 and 10 p.i. For the experiments presented in the paper, however, the cultures were harvested late in infection, at 14 days p.i. In light of this timing, it appears possible that TLR2 ligands are perhaps not stably expressed by Orientia but that their synthesis sets in late in infection. Similarly, it has been shown for Staphylococcus aureus lipoproteins that environmental factors such as an acidic pH or a postlogarithmic growth phase cause enrichment of diacyl rather than triacyl forms, which are known to have diverging TLR2 heterodimer specificities (11–13).
In summary, we demonstrate that the O. tsutsugamushi Karp strain used for the study by Gharaibeh et al. (1) was not contaminated by Mycoplasma sp. The limited investigation by Tantibhedhyangkul et al. leaves many questions unanswered and does not warrant concluding that TLR2 ligands are absent from O. tsutsugamushi. We would, however, like to emphasize that further research is required for a better understanding of the synthesis of TLR2 ligands by O. tsutsugamushi and their recognition.
Footnotes
This is a response to a letter by Tantibhedhyangkul et al. (https://doi.org/10.1128/IAI.00269-17).
REFERENCES
- 1.Gharaibeh M, Hagedorn M, Lilla S, Hauptmann M, Heine H, Fleischer B, Keller C. 2016. Toll-like receptor 2 recognizes Orientia tsutsugamushi and increases susceptibility to murine experimental scrub typhus. Infect Immun 84:3379–3387. doi: 10.1128/IAI.00185-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Kuppeveld FJM, Van der Logt JTM, Angulo AF, Van Zoest MJ, Quint WGV, Niesters HGM, Galama JMD, Melchers WJG. 1992. Genus- and species-specific identification of mycoplasmas by 16S rRNA amplification. Appl Environ Microbiol 58:2606–2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahajan SK, Rolain JM, Kashyap R, Bakshi D, Sharma V, Prasher BS, Pal LS, Raoult D. 2006. Scrub typhus in Himalayas. Emerg Infect Dis 12:1590–1592. doi: 10.3201/eid1210.051697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogawa M, Uchiyama T, Satoh M, Ando S. 2013. Decontamination of mycoplasma-contaminated Orientia tsutsugamushi strains by repeating passages through cell cultures with antibiotics. BMC Microbiol 13:32. doi: 10.1186/1471-2180-13-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takeuchi O, Kaufmann A, Grote K, Kawai T, Hoshino K, Morr M, Muhlradt PF, Akira S. 2000. Cutting edge: preferentially the R-stereoisomer of the mycoplasmal lipopeptide macrophage-activating lipopeptide-2 activates immune cells through a Toll-like receptor 2- and MyD88-dependent signaling pathway. J Immunol 164:554–557. doi: 10.4049/jimmunol.164.2.554. [DOI] [PubMed] [Google Scholar]
- 6.Hashimoto M, Tawaratsumida K, Kariya H, Aoyama K, Tamura T, Suda Y. 2006. Lipoprotein is a predominant Toll-like receptor 2 ligand in Staphylococcus aureus cell wall components. Int Immunol 18:355–362. doi: 10.1093/intimm/dxh374. [DOI] [PubMed] [Google Scholar]
- 7.Tantibhedhyangkul W, Ben Amara A, Textoris J, Gorvel L, Ghigo E, Capo C, Mege JL. 2013. Orientia tsutsugamushi, the causative agent of scrub typhus, induces an inflammatory program in human macrophages. Microb Pathog 55:55–63. doi: 10.1016/j.micpath.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Tantibhedhyangkul W, Prachason T, Waywa D, El Filali A, Ghigo E, Thongnoppakhun W, Raoult D, Suputtamongkol Y, Capo C, Limwongse C, Mege JL. 2011. Orientia tsutsugamushi stimulates an original gene expression program in monocytes: relationship with gene expression in patients with scrub typhus. PLoS Negl Trop Dis 5:e1028. doi: 10.1371/journal.pntd.0001028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MK, Kang JS. 2001. Orientia tsutsugamushi suppresses the production of inflammatory cytokines induced by its own heat-stable component in murine macrophages. Microb Pathog 31:145–150. doi: 10.1006/mpat.2001.0457. [DOI] [PubMed] [Google Scholar]
- 10.Tsai MH, Chang CH, Tsai RK, Hong YR, Chuang TH, Fan KT, Peng CW, Wu CY, Hsu WL, Wang LS, Chen LK, Yu HS. 2016. Cross-regulation of proinflammatory cytokines by interleukin-10 and miR-155 in Orientia tsutsugamushi-infected human macrophages prevents cytokine storm. J Investig Dermatol 136:1398–1407. doi: 10.1016/j.jid.2015.11.034. [DOI] [PubMed] [Google Scholar]
- 11.Takeuchi O, Sato S, Horiuchi T, Hoshino K, Takeda K, Dong Z, Modlin RL, Akira S. 2002. Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins. J Immunol 169:10–14. doi: 10.4049/jimmunol.169.1.10. [DOI] [PubMed] [Google Scholar]
- 12.Kang JY, Nan X, Jin MS, Youn SJ, Ryu YH, Mah S, Han SH, Lee H, Paik SG, Lee JO. 2009. Recognition of lipopeptide patterns by Toll-like receptor 2-Toll-like receptor 6 heterodimer. Immunity 31:873–884. doi: 10.1016/j.immuni.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 13.Kurokawa K, Kim MS, Ichikawa R, Ryu KH, Dohmae N, Nakayama H, Lee BL. 2012. Environment-mediated accumulation of diacyl lipoproteins over their triacyl counterparts in Staphylococcus aureus. J Bacteriol 194:3299–3306. doi: 10.1128/JB.00314-12. [DOI] [PMC free article] [PubMed] [Google Scholar]