Abstract
The increased focus on patient and family-centered care in adult intensive care units (ICUs) has generated multiple platforms for clinician–family communication beyond traditional interdisciplinary family meetings (family meetings)—including family-centered rounds, bedside or telephone updates, and electronic family portals. Some clinicians and administrators are now using these platforms instead of conducting family meetings. For example, some institutions are moving toward using family-centered rounds as the main platform for clinician–family communication, and some physicians rely on brief daily updates to the family at the bedside or by phone, in lieu of family meetings. We argue that although each of these platforms is useful in some circumstances, there remains an important role for family meetings. We outline five goals of clinician–family communication—establishing trust, providing emotional support, conveying clinical information, understanding the patient as a person, and facilitating careful decision making—and we examine the extent to which various communication platforms are likely to achieve the goals. We argue that because no single platform can achieve all communication goals, an integrated strategy is needed. We present a model that integrates multiple communication platforms to effectively and efficiently support families across the arc of an ICU stay. Our framework employs bedside/telephone conversations and family-centered rounds throughout the admission to address high informational needs, along with well-timed family meetings that attend to families’ emotions as well as patients’ values and goals. This flexible model uses various communication platforms to achieve consistent, efficient communication throughout the ICU stay.
Keywords: family conference, family meetings, intensive care unit, family-centered rounds, communication, decision-making
The last decade has seen a major focus on improving clinician–family communication in intensive care units (ICUs) as a way to mitigate well-documented problems with family members’ understanding of their loved ones’ condition and treatment options (1–4), high rates of emotional distress that often progress to post-traumatic stress disorder (5–7), and concerns that treatment is inconsistent with patients’ preferences and values (8–11). These problems have motivated the development and implementation of various platforms for clinician–family communication in the ICU. The platforms include family-centered rounds, daily updates, electronic patient portals, and interdisciplinary family meetings (Table 1).
Table 1.
Common platforms for clinician–family communication
| Platform | Definition | |
|---|---|---|
| Family-centered rounds | Family-centered rounds involve adapting the traditional multidisciplinary team rounding process to include family members. There are different versions of family-centered rounds described in the literature, but they share several core elements: families are invited to be at the bedside when multidisciplinary team rounds are conducted; they are provided a brief lay summary of the patient’s condition and allowed to listen in as the patient is discussed; and they are permitted a brief opportunity to ask questions. Family-centered rounds were first described in the pediatric setting (25, 37, 38), and then in the adult trauma ICU setting (24, 39), and have expanded to other general and specialty adult ICU settings (26, 27) |
|
| Daily updates | Daily updates involve physicians providing clinical information to family members. This may occur at the bedside—when an individual physician is conducting a patient visit, or he or she might stop by because the family has requested an update or has additional questions. Alternatively, the daily update can be conducted via telephone call. Daily updates at the bedside may or may not involve other physicians (residents, interns, etc.) or nursing staff and updates via telephone occur exclusively between the physician and a family member |
|
| Electronic patient portals | Electronic applications that allow family members to remotely access patient updates, receive general health/illness information, and possibly “message” clinicians. They have also been proposed as a vehicle to allow family members to input information about patient values and preferences (29) |
|
| Interdisciplinary family meeting | A meeting in a private place including the nurse, physician, and other members of the team to offer the family information about prognosis and treatment, hear questions, discuss the patient as a person, guide decision-making as needed, and provide emotional support (31, 32) |
Definition of abbreviation: ICU = intensive care unit.
We have observed that some clinicians have begun using family-centered rounds or brief daily updates to the family, at the bedside or by phone, in lieu of family meetings. The impact of such substitutions cannot be assessed without a clear framework for understanding the roles that different communication platforms play in achieving overall communication goals. A better understanding of these roles is critical for determining how best to use the various communication platforms.
In this article we propose five overarching goals of clinician–family communication and examine the extent to which various platforms for communication are likely to achieve them. We argue that each communication platform can serve an important role, but none are adequate in isolation. We propose a model for how these different platforms can be integrated to effectively and efficiently support the family members of critically ill ICU patients and foster collaborative decision making.
Five Goals of Clinician–Family Communication
On the basis of a review of the literature on family experience in the ICU, decision theory, decision psychology, and ICU decision-making, we propose five major goals of clinician–family communication in the ICU setting.
Establishing a Trusting Relationship
In a survey of family members of seriously ill patients, having trust and confidence in the patient’s physician was the most highly ranked element of care quality (12). Shared decision-making, the recommended model for decision-making in the ICU (13), requires that families have trust in the clinical team to engage in collaborative decision-making and to genuinely consider the team’s recommendations (14, 15). Likewise, clinicians must depend on family members to provide an accurate portrayal of the patient’s values and preferences.
Providing Emotional Support to Families
Research with the family members of critically ill ICU patients consistently demonstrates that they have high levels of emotional stress (6, 7, 16) and experience intense negative emotions such as fear and anxiety in response to both the present threat (critical illness) and the anticipation of decision-making (17, 18). Research from the field of decision science suggests that strong negative emotions such as fear and anxiety can substantially impair information processing and deliberation if there is no pause to acknowledge emotions and reflect on them (19). By providing emotional support (e.g., allowing opportunities for families to express their fears and acknowledging the emotional intensity of the situation through empathetic statements [18]) clinicians may be able to lessen emotional distress and thereby improve information processing and deliberation.
Helping Families to Understand Diagnosis, Prognosis, and Treatment Options
In order for families to be informed participants in decision-making, they need a clear and timely understanding of the patient’s diagnosis, prognosis, and treatment options (2, 20, 21). This allows families to consider the potential outcomes of treatment in light of patient preferences and values. Without adequate information, families’ decisions may not serve the patient’s interests because they may not be based on a solid grasp of the clinical situation. A lack of honest, understandable, and consistent information is also a great source of stress and frustration to families (2).
Allowing Clinicians to Understand the Patient as a Person
To make patient-centered treatment recommendations, clinicians need to understand a patient’s values and preferences. When clinicians understand patients’ values—what was important to the person before this ICU admission—they can help families understand how various treatments and care outcomes may be more or less consistent with those values (13, 22).
Creating Conditions for Careful Deliberation about Difficult Decisions
Given the complexity of decisions that arise in patients with advanced illness, it is important to ensure that clinicians and families have the opportunity to deliberate carefully about treatment options. Deliberation is a process that requires understanding the relevant clinical facts; appreciating how different choices impact the patient’s individual situation; and reasoning, or weighing the risks and benefits, to arrive a final choice (23).
In the setting of shared decision-making, deliberation is an interactive process that requires adequate time and attention to the task. Family members create for clinicians a picture of the patient—how she spends her time, what is important to her—and clinicians translate treatment options and their attendant outcomes into pictures of health states that will have varying concordance with patient values and preferences (13). During this process there are multiple cognitive-emotional dynamics at work that threaten to preclude a full exploration of each option and precipitate a premature decision (17). For example, individuals experiencing high levels of anxiety or conflict are often motivated to make decisions to decrease their level of arousal (17). In the context of decision-making about life-sustaining treatment, a surrogate may declare a final choice before fully exploring all options to avoid emotional distress. Individuals also tend to equate a decision’s outcomes (honoring a loved one’s wishes) with the resulting emotions (sadness or regret on her death). Therefore, families might struggle to recognize the choice that honors the patient’s wishes, because it is associated with negative emotions. By creating a setting in which family members are guided and supported through a discussion of all potential choices, clinicians help to avoid hasty decisions that are not patient-centered.
Platforms for Clinician–Family Communication
Table 1 presents a brief description of the most commonly used platforms for clinician–family communication in the ICU.
Strengths and Weaknesses of Each Communication Platform
We examine each platform to understand its benefits and drawbacks. No one achieves all five communication goals.
Family-centered rounds: Family-centered rounds are valuable in achieving several important communication goals. Daily communication with the clinical team helps to build trust by allowing the family to see the clinical team’s efforts on behalf of the patient (2, 12). Family-centered rounds are a good platform for delivering clinical information and may foster improved understanding because families have the opportunity to hear the plan of care on a daily basis, with input from multiple clinicians. Because the bedside nurse is included, he or she is able to clarify questions and concerns after rounds, should they arise. Including family members on rounds is an efficient strategy and adds only a little time to rounds (24, 25).
However, family-centered rounds may be a less effective platform for achieving other communication goals. Rounds are a highly cognitive, information-oriented activity. To shift the discussion from clinical facts to an examination of values and preferences would require considerable reframing, especially in the very public setting of rounds. Although it is possible to demonstrate empathy and sensitivity during rounds, they are an awkward setting for the delivery of prognostic information or for addressing family conflict.
In addition, it is difficult to consider how family deliberation about difficult decisions could occur during time-pressured multidisciplinary rounds. Not all family members report feeling comfortable participating in family-centered rounds; and some express uncertainty regarding how to participate in this clinician-centric activity (26). Without a comfortable, private space where participants are giving their full attention to the larger picture of the patient and his/her situation, the deliberation process is shortchanged. This may explain why, in a study evaluating family-centered rounds, family members reported relatively high satisfaction with the frequency of communication and support for decision-making, but less satisfaction with time for decision-making (27).
Finally, attendance at family-centered rounds is not feasible for all family members. Families express dissatisfaction with needing to be at rounds at a specific time (24), as this can interfere with work or caregiving responsibilities (26, 28).
Daily updates: Daily updates allow clinicians to keep family members informed about treatment and progress. Because they are more private than family-centered rounds, family members may feel more comfortable asking questions. Daily updates are also time flexible, and may be the best option for families with work or caregiving responsibilities that prevent them from attending family-centered rounds. Likewise, phone updates are especially valuable to family members who cannot travel to the hospital because of health issues, distance, or transportation difficulties. Daily communication via updates, both bedside and telephone, can help to build trust with clinicians.
However, there are several disadvantages to bedside updates. Because they are typically short conversations, they are not suitable for discussions of values or deliberation about difficult decisions. In addition, clinicians and family members may feel uncomfortable talking about the patient, in front of the patient (21). And although bedside updates can build trust, they can also erode it: one of the most frustrating experiences family members describe is having different clinicians stop in to update them, each offering a different (and conflicting) report (2).
Patient portals: Patient portals offer a promising means of providing families with clinical information and offering them a place to direct their questions. Portals allow family members to receive updates on the patient and review accurate, scientifically sound information at a time and in a place that is convenient for them. Preliminary surveys demonstrate predominantly favorable responses from family members regarding the use of electronic patient portals, although there is some variation by demographic group (29). Clinicians are generally positive about the use of portals, but stress the need for careful design of such systems (30). Portals also offer the opportunity to gather preliminary information about preferences and values, enabling clinicians to better understand the patient as a person.
However, portals are limited because the exchange of information is asynchronous, and the application of information about values and preferences to decision-making requires skilled, in-person facilitation. Furthermore, portals are unable to provide timely emotional support. Although patient portals are used in a variety of other health care settings, they are a recent development for use in the ICU and not widely available; and it is unclear how patient updates would be entered into the system or how labor-intensive “messaging” might be for clinicians.
Interdisciplinary family meetings: Interdisciplinary family meetings can be a good platform for providing information, because the meeting brings together multiple members of the clinical team (attending, consultants, bedside nurses, and other members of the team). Interdisciplinary family meetings provide a private space for families to share information about the patient’s preferences and values, and they are an especially good setting for delivering difficult news. But perhaps the most important feature of the family meeting is its suitability for facilitating high-quality deliberation about difficult decisions (31, 32). The platform is uniquely positioned to help families consider how the outcomes of various treatment options align (or don’t align) with patient preferences and values while being supported emotionally. The inclusion of social work or pastoral care staff can provide focused psychosocial and spiritual support. There is evidence that family meetings are effective in improving multiple patient and family-centered outcomes (33–36).
However, family meetings have several major limitations. First it is difficult to schedule a time when family members and all necessary members of the clinical team can attend. Second, they are time-consuming, and because they require the undivided attention of multiple clinicians, they are resource intensive. This makes them a poor choice for daily communication.
A Multimodal Strategy for Clinician–Family Communication
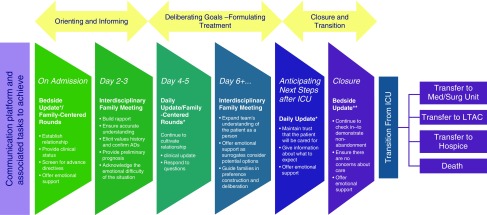
Given that no single communication platform is able to achieve all the goals of clinician–family communication, the best approach may be to strategically combine platforms in a deliberate way to efficiently achieve the five proposed communication goals. In Figure 1, we offer a model of how the multiple platforms for communication can be integrated across the ICU stay.
Figure 1.
*Bedside updates offer clinical information, empathetic acknowledgment of the emotional difficulty of the situation, and an opportunity for families to ask questions. If families are unable to be at the bedside, a phone update may be given, although it may be more difficult to relate to family emotionally. Family-centered rounds help achieve similar goals, and families should be invited to attend from the time of admission. However, on the day of admission, an in-person update is a more personal approach. **During closure and transition from the intensive care unit, bedside visits may also be made by social work, pastoral care, or palliative care staff, depending on the patient situation. ADs = advance directives; ICU = intensive care unit; LTAC = long-term acute care.
In the model we propose, the goals for communication build on each other. For example, when a patient is admitted, family are often overwhelmed and do not know the extent of the patient’s illness, and clinicians know little about the patient as a person. Therefore, the early goals focus on establishing a trusting relationship and allowing both clinicians and families to gather the information they need, respectively. This can be achieved through an update (optimally in-person) on Day 1, an invitation to join family-centered rounds, and a family meeting on Days 2–3, depending on availability of family and staff. In this phase the primary goals are orienting the family, exchanging basic information, and establishing trust.
As the family becomes less overwhelmed and there is greater clarity about the patient’s condition, we move into the phase of deliberation about goals and formulation of a treatment plan, with an appropriately timed family meeting. The family is encouraged to attend family-centered rounds if able. If not, a daily update can be provided at the bedside or by phone. On the basis of the patient’s status and any decision points, clinicians assess the need for additional family meetings and follow up after each family meeting to see whether the family has any outstanding questions or concerns and to ensure that any decisions have been integrated into the plan of care.
By the third phase, when goals of care have been solidified and clinical outcomes are more apparent, the family and the clinical team can plan for transition from the ICU. For some patients this may involve moving to a different level of care within the hospital; for others it will entail transfer to a care setting outside the hospital, such as long-term care, rehabilitation, or hospice; and finally, some patients will die in the ICU. The support provided to families in this phase will vary widely depending on the individual trajectory, but the overarching objective is to maintain communication and support through departure from the ICU. Other members of the clinical team may be helpful in providing information and support. Social workers or care managers can offer specific details about the transfer process to an outside facility, and palliative care or pastoral care staff may give emotional support or facilitate particular religious observances in accordance with family needs and wishes.
The timeframes for this model are fluid and may be compressed or expanded, depending on the patient’s status and the needs of the family. For example, when a patient is acutely ill, or when it is clear from the first encounter that further curative care is inconsistent with the patient’s prior expressed preferences, a family meeting is warranted as early as possible. Likewise, if there is an abrupt change in the patient’s clinical course or new insights on the part of family members, a meeting should be scheduled. Family situations involving great geographic distance or surrogates with health problems or caregiving responsibilities will necessitate accommodations, employing creative solutions such as phone or video-conferencing. Finally, there are challenging circumstances—language and cultural barriers, ICU care after a serious adverse event, or intractable conflict within families—which will require additional resources.
Conclusion
Multiple platforms have been developed and implemented to enhance clinician–family communication. Rather than rely on a single platform, there are compelling reasons for clinicians to use them in combination. Models that combine interdisciplinary family meetings with other platforms can leverage the unique contribution of each to efficiently achieve all core elements of clinician–family communication.
Supplementary Material
Footnotes
Supported by a departmental T-32 postdoctoral scholarship (T32-HL007820; PI, Michael R. Pinsky) (J.B.S.); by the University of Pittsburgh’s Claude D. Pepper Older Americans Independence Center (P30 AG024827; PI, Susan Greenspan) (L.P.S.); and by grants from the National Institutes of Health, National Institute on Aging (4R01AG045176; PI, D.B.W.) and the National Institutes of Health, National Institute of Nursing Research (5R01NR014663; PI, D.B.W.).
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, Canoui P, Le Gall JR, Schlemmer B. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–3049. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 2.Nelson JE, Puntillo KA, Pronovost PJ, Walker AS, McAdam JL, Ilaoa D, Penrod J. In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med. 2010;38:808–818. doi: 10.1097/ccm.0b013e3181c5887c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson JE, Mercado AF, Camhi SL, Tandon N, Wallenstein S, August GI, Morrison RS. Communication about chronic critical illness. Arch Intern Med. 2007;167:2509–2515. doi: 10.1001/archinte.167.22.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White DB, Ernecoff N, Buddadhumaruk P, Hong S, Weissfeld L, Curtis JR, Luce JM, Lo B. Prevalence of and factors related to discordance about prognosis between physicians and surrogate decision makers of critically ill patients. JAMA. 2016;315:2086–2094. doi: 10.1001/jama.2016.5351. [DOI] [PubMed] [Google Scholar]
- 5.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336–346. doi: 10.7326/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 6.McAdam JL, Dracup KA, White DB, Fontaine DK, Puntillo KA. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med. 2010;38:1078–1085. doi: 10.1097/CCM.0b013e3181cf6d94. [DOI] [PubMed] [Google Scholar]
- 7.McAdam JL, Fontaine DK, White DB, Dracup KA, Puntillo KA. Psychological symptoms of family members of high-risk intensive care unit patients. Am J Crit Care. 2012;21:386–393, quiz 394. doi: 10.4037/ajcc2012582. [DOI] [PubMed] [Google Scholar]
- 8.Danis M, Patrick DL, Southerland LI, Green ML. Patients’ and families’ preferences for medical intensive care. JAMA. 1988;260:797–802. [PubMed] [Google Scholar]
- 9.Lynn J, Teno JM, Phillips RS, Wu AW, Desbiens N, Harrold J, Claessens MT, Wenger N, Kreling B, Connors AF, Jr SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. perceptions by family members of the dying experience of older and seriously ill patients. Ann Intern Med. 1997;126:97–106. doi: 10.7326/0003-4819-126-2-199701150-00001. [DOI] [PubMed] [Google Scholar]
- 10.Barnato AE, Herndon MB, Anthony DL, Gallagher PM, Skinner JS, Bynum JP, Fisher ES. Are regional variations in end-of-life care intensity explained by patient preferences? A study of the US Medicare population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998;158:1163–1167. doi: 10.1164/ajrccm.158.4.9801108. [DOI] [PubMed] [Google Scholar]
- 12.Heyland DK, Dodek P, Rocker G, Groll D, Gafni A, Pichora D, Shortt S, Tranmer J, Lazar N, Kutsogiannis J, et al. Canadian Researchers End-of-Life Network (CARENET) What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174:627–633. doi: 10.1503/cmaj.050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kon AA, Davidson JE, Morrison W, Danis M, White DB. Shared decision-making in intensive care units: executive summary of the American College of Critical Care Medicine and American Thoracic Society policy statement. Am J Respir Crit Care Med. 2016;193:1334–1336. doi: 10.1164/rccm.201602-0269ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, Cox CE, Wunsch H, Wickline MA, Nunnally ME, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 15.Johnson SK, Bautista CA, Hong SY, Weissfeld L, White DB. An empirical study of surrogates’ preferred level of control over value-laden life support decisions in intensive care units. Am J Respir Crit Care Med. 2011;183:915–921. doi: 10.1164/rccm.201008-1214OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al. FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 17.Power TE, Swartzman LC, Robinson JW. Cognitive-emotional decision making (CEDM): a framework of patient medical decision making. Patient Educ Couns. 2011;83:163–169. doi: 10.1016/j.pec.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 18.Selph RB, Shiang J, Engelberg R, Curtis JR, White DB. Empathy and life support decisions in intensive care units. J Gen Intern Med. 2008;23:1311–1317. doi: 10.1007/s11606-008-0643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dionne-Odom JN, Willis DG, Bakitas M, Crandall B, Grace PJ. Conceptualizing surrogate decision making at end of life in the intensive care unit using cognitive task analysis. Nurs Outlook. 2015;63:331–340. doi: 10.1016/j.outlook.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999;319:780–782. doi: 10.1136/bmj.319.7212.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson WG, Cimino JW, Ernecoff NC, Ungar A, Shotsberger KJ, Pollice LA, Buddadhumaruk P, Carson SS, Curtis JR, Hough CL, et al. A multicenter study of key stakeholders’ perspectives on communicating with surrogates about prognosis in intensive care units. Ann Am Thorac Soc. 2015;12:142–152. doi: 10.1513/AnnalsATS.201407-325OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med. 2012;186:480–486. doi: 10.1164/rccm.201204-0710CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grisso T, Appelbaum PS. Assessing competence to consent to treatment: a guide for physicians and other health professionals. New York: Oxford University Press; 1998. [Google Scholar]
- 24.Mangram AJ, Mccauley T, Villarreal D, Berne J, Howard D, Dolly A, Norwood S. Families’ perception of the value of timed daily “family rounds” in a trauma ICU. Am Surg. 2005;71:886–891. [PubMed] [Google Scholar]
- 25.Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832. doi: 10.1542/peds.2006-2528. [DOI] [PubMed] [Google Scholar]
- 26.Fanning JB, Farkas CM, DeWitt PM, Webster TH, Burnam J, Piras SE, Schenck D, Miller A. Obstacles to shared expectations in a burn intensive care unit. Qual Health Res. 2015;27:351–362. doi: 10.1177/1049732315616619. [DOI] [PubMed] [Google Scholar]
- 27.Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19:421–430. doi: 10.4037/ajcc2010656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stelson EA, Carr BG, Golden KE, Martin N, Richmond TS, Delgado MK, Holena DN. Perceptions of family participation in intensive care unit rounds and telemedicine: a qualitative assessment. Am J Crit Care. 2016;25:440–447. doi: 10.4037/ajcc2016465. [DOI] [PubMed] [Google Scholar]
- 29.Brown SM, Bell SK, Roche SD, Dente E, Mueller A, Kim TE, O’Reilly K, Lee BS, Sands K, Talmor D. Preferences of current and potential patients and family members regarding implementation of electronic communication portals in intensive care units. Ann Am Thorac Soc. 2016;13:391–400. doi: 10.1513/AnnalsATS.201509-638OC. [DOI] [PubMed] [Google Scholar]
- 30.Bell SK, Roche SD, Johansson AC, O’Reilly KP, Lee BS, Sands KE, Talmor DS, Brown SM. Clinician perspectives on an electronic portal to improve communication with patients and families in the intensive care unit. Ann Am Thorac Soc. 2016;13:2197–2206. doi: 10.1513/AnnalsATS.201605-351OC. [DOI] [PubMed] [Google Scholar]
- 31.Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest. 2008;134:835–843. doi: 10.1378/chest.08-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curtis JR, Patrick DL, Shannon SE, Treece PD, Engelberg RA, Rubenfeld GD. The family conference as a focus to improve communication about end-of-life care in the intensive care unit: opportunities for improvement. Crit Care Med. 2001;29(2) Suppl:N26–N33. doi: 10.1097/00003246-200102001-00006. [DOI] [PubMed] [Google Scholar]
- 33.Cypress BS. Family conference in the intensive care unit: a systematic review. Dimens Crit Care Nurs. 2011;30:246–255. doi: 10.1097/DCC.0b013e3182277001. [DOI] [PubMed] [Google Scholar]
- 34.Lilly CM, De Meo DL, Sonna LA, Haley KJ, Massaro AF, Wallace RF, Cody S. An intensive communication intervention for the critically ill. Am J Med. 2000;109:469–475. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 35.Glavan BJ, Engelberg RA, Downey L, Curtis JR. Using the medical record to evaluate the quality of end-of-life care in the intensive care unit. Crit Care Med. 2008;36:1138–1146. doi: 10.1097/CCM.0b013e318168f301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powazki R, Walsh D, Hauser K, Davis MP. Communication in palliative medicine: a clinical review of family conferences. J Palliat Med. 2014;17:1167–1177. doi: 10.1089/jpm.2013.0538. [DOI] [PubMed] [Google Scholar]
- 37.Lewis C, Knopf D, Chastain-Lorber K, Ablin A, Zoger S, Matthay K, Glasser M, Pantell R. Patient, parent, and physician perspectives on pediatric oncology rounds. J Pediatr. 1988;112:378–384. doi: 10.1016/s0022-3476(88)80316-0. [DOI] [PubMed] [Google Scholar]
- 38.Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83:292–297. doi: 10.1097/ACM.0b013e3181637e21. [DOI] [PubMed] [Google Scholar]
- 39.Schiller WR, Anderson BF. Family as a member of the trauma rounds: a strategy for maximized communication. J Trauma Nurs. 2003;10:93–101. doi: 10.1097/00043860-200310040-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.