Abstract
Introduction
To study the degree to which individuals in different trajectories of cigarette smoking from adolescence to the early 40s are similar or different in terms of lack of preventive health behaviors (e.g., underuse of preventive health services, unhealthy eating habits) in early midlife.
Methods
Participants came from a community-based random sample of residents in two upstate New York counties (N=548). Data were collected from adolescence to early midlife (mean age = 43, SD = 2.8) at seven time points. Using growth mixture modeling, we statistically identified the number of smoking trajectories. Logistic regression analysis was used to study the relationship between the probabilities of participants’ smoking trajectory group membership and lack of preventive behaviors in early midlife.
Results
Five trajectory groups of cigarette smokers were identified. With controls, as compared to the nonsmoker trajectory group, higher probabilities of belonging to the heavy/continuous smoker trajectory group and the late starter trajectory groups were significantly associated with a higher likelihood of lack of preventive health behaviors (Adjusted Odds Ratio [A.O.R.] = 3.49; A.O.R. =4.02, respectively). In addition, as compared to the quitter/decreaser trajectory group, higher probabilities of belonging to the heavy/continuous smoker trajectory group and the late starter trajectory group were also significantly associated with a higher likelihood of lack of preventive health behaviors (A.O.R. = 3.51; A.O.R. = 4.04, respectively).
Conclusions
Intervention programs may consider focusing on heavy/continuous smokers and late starters in programs designed to promote adequate use of preventive health services and healthy general lifestyles in early midlife.
Keywords: Trajectory of cigarette smoking, Lack of preventive health behaviors, Underuse of preventive health services, Unhealthy eating habits, Poor sleeping habits, Lack of exercise
INTRODUCTION
Lack of preventive health behaviors, such as underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise, has become a major public health concern (Frieden, 2012; Moore & Thompson, 2015). The CDC recently published a report (Frieden, 2012) on the underutilization of preventive services. Just half of the adults living in the U.S. received clinical preventive services, such as screenings, from 2007 to 2010. There are serious and alarming consequences of the underuse of preventive health services. Farley, Dalal, Mostashari, and Frieden (2010) estimated that increasing the use of nine clinical prevention services to more optimal levels could prevent 50,000–100,000 deaths each year among adults younger than 80 years of age. As regards general unhealthy lifestyles such as unhealthy eating habits, poor sleeping habits, and lack of exercise, only 13.1% of U.S. respondents met recommendations for fruit intake and 8.9% met vegetable intake recommendations (Moore & Thompson, 2015); approximately one-half of U.S. adults (50.3%) met neither aerobic nor muscle-strengthening guidelines (Schoenborn, Adams, & Peregoy, 2013); and more than one third of U.S. adults (aged 18–60) reported typically sleeping less than 7 hours in a 24–hour period (Liu, 2016). The long-term adverse health consequences of general unhealthy lifestyles have been documented (e.g., Lim, Vos, Flaxman et al., 2013). According to Lim, Vos, Flaxman et al. (2013), dietary risk factors (especially diets low in fruits) and physical inactivity collectively accounted for 10% of global deaths and disability-adjusted life years (DALY) in 2010.
A main risk factor for lack of preventive behaviors is cigarette smoking, which is one of the leading risk factors for chronic diseases and mortality in the U.S (Centers for Disease Control and Prevention [CDC], 2008a, 2008b; U.S. Department of Health and Human Services, 2010), as well as in the world (Beaglehole Bonita, Horton et al., 2011; Lim et al., 2013). Research has found that smoking is often associated with lack of preventive health behaviors, including underuse of preventive health services (Bryan, Westmaas, Alcaraz, & Jemal, 2014; Chao, Connell, Cokkinides et al., 2004). With regards to general unhealthy lifestyles, research has shown that smokers have unhealthy patterns of nutrient intake compared with nonsmokers (Dallongeville, Marécaux, Fruchart, & Amouyel, 1998). Heavy smoking was strongly associated with a poor diet and low level of physical activity (Lohse, Rohrmann, Bopp, & Faeh, 2016). Cigarette smokers were also significantly more likely than nonsmokers to report problems going to sleep, problems staying asleep, and daytime sleepiness (Name deleted to protect the integrity of the review process, 2012; Phillips & Danner, 1995).
Even though the associations between cigarette smoking and lack of preventive health behaviors have been documented (e.g., Name deleted to protect the integrity of the review process, 2012; Bryan et al., 2014; Chao et al., 2004; Dallongeville et al., 1998; Lohse et al., 2016), several important gaps in the literature remain. First, many of the studies are cross-sectional in nature, and thus one is limited in the ability to make inferences regarding the time ordering of cigarette smoking and lack of preventive health behaviors. Second, although other studies have examined the association between cigarette smoking and preventive health behaviors, they do not control for a number of individual vulnerability and family environmental factors. Third, none of the research has examined patterns of different subgroups of cigarette smoking over time as they are associated with lack of preventive health behaviors. Particularly, despite public health relevance, there are no longitudinal studies examining smoking behaviors in adolescence and extending through the early forties and their associations with preventive health behaviors in early midlife. Early midlife is a period when many preventable health problems become manifest (Guralnik, Butterworth, Patel, Mishra, & Kuh, 2009; Pope, Sowers, Welch, & Albrecht, 2001). However, many individuals in midlife are in need of, but do not engage in, preventive health behaviors (Miller, King, Joseph, Richardson, 2012; Schoenborn, Adams, & Peregoy, 2013).
Several individual vulnerabilities in adolescence such as depression may play a role in both later cigarette smoking and later lack of preventive health behaviors (Bogner & Wittink, 2004; Katon, Russo, Heckbert et al., 2010; Pirraglia, Sanyal, Singer, & Ferris, 2004). Studies have shown that earlier low perceived self-control is associated with cigarette smoking (Wills & Dishion, 2004) and health (Skaff, 2007). According to problem behavior theory (Jessor & Jessor, 1977), higher levels of externalizing problem behaviors in adolescence such as delinquency and rebellion are related to smoking behavior. A large body of research has shown that earlier family environment correlates with the lack of preventive health behaviors (Pampel, Krueger, & Denney, 2010). More specifically, high household income is associated with less cigarette smoking and the presence of preventive health behaviors (McLeod & Kessler, 1990; Pampel, Krueger, & Denney, 2010). Thus, we statistically controlled for these demographic and personal behavioral factors in our analysis. In addition, since adult obesity is related to the lack of preventive health behaviors, such as poor diet, and low physical activity, we also statistically controlled for concurrent obesity status.
Operating within a life-span developmental perspective, we applied a prospective longitudinal design and followed youngsters in a community sample from early adolescence into early midlife. In the present research, we used the growth mixture modeling (GMM) approach (Muthén & Shedden, 1999) that differentiates the chronicity and severity of patterns of cigarette smoking spanning several important developmental stages, such as early adolescence, late adolescence, emerging adulthood, and adulthood. This group-based approach is suited to analyzing questions about the developmental trajectories that are inherently categorical, such as cigarette smoking. Differentiation among patterns of development of cigarette smoking may then be used to predict the likelihood of lack of preventive health behaviors in later years. Thus, this approach, which covers several significant developmental periods, has an advantage over an analysis that examines the extent to which cigarette smoking at only one or two points in time during early developmental periods, or average cigarette smoking during lifetime predicts lack of preventive health behaviors.
Several teams of investigators have used trajectory analysis to examine distinctive smoking patterns or trajectory groups and to assess the differential associations of these patterns with predictors and consequences (Chassin et al., 2008; Costello, Dierker, Jones, and Rose, 2008; Riggs, Chou, Li, and Pentz, 2007). Our previous trajectory analyses (Name deleted to protect the integrity of the review process, 2011) have identified five groups of smokers from adolescence (mean age=14) to the late 30s (mean age=37). One of the extreme trajectory groups is characterized by chronic, heavy cigarette smokers, while the other consists of nonsmokers. There are also three intermediate trajectory groups which consist of occasional smokers, late starters, and quitters. In the present study, we extended our previous trajectory analyses by including the measure of cigarette smoking in the early forties.
Hypothesis
Based on the research in the literature and our prior research, our hypothesis is as follows: Trajectories of cigarette smoking predict lack of preventive health behaviors in early midlife, i.e., underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise. Specifically, trajectories of heavy continuous smokers and late starters as compared with nonsmokers and quitters/decreasers will be associated with an increased likelihood of lack of preventive health behaviors despite control on individual vulnerability and family environmental factors in adolescence.
METHODS
Participants and Procedure
Data on the participants in this study came from a community-based random sample residing in two upstate New York counties (Albany and Saratoga) first assessed for drug use in 1983. The sample was taken from an earlier study using maternal interviews in 1975 (T1). The participants’ mothers were interviewed about the participants in 1975 (T1) to assess problem behavior among youngsters. At T1, population data from the census (updated in 1975) for sampling units in Albany and Saratoga counties were obtained. A systematic sample of primary sampling units (blocks) in each county was then drawn with probability proportional to the number of households. At the time the data was collected, the sampled families were generally representative of the population of families in the counties. There was a close match of the participants on family income, maternal education, and family structure with the 1980 census. Mothers with one or more child(ren) in the age range of 1–10 were recruited. When there were multiple children in the family, one child in that age range was randomly selected. With regard to ethnicity, the sample was 90% White, 8% African American, and 2% other ethnic/racial minorities. Forty nine percent of the children were females. The detailed sampling procedures were published elsewhere (Name deleted to protect the integrity of the review process, 1986). Interviews of the participants were conducted in 1983 (T2, N=756), 1985–1986 (T3, N=739), 1992 (T4, N=750), 1997 (T5, N=749), 2002 (T6, N=673), 2005–2006 (T7, N=607), and 2012–2013 (T8, N=548). The mean ages (SDs) of participants at the follow-up interviews were 14.1 (2.8) at T2, 16.3 (2.8) at T3, 22.3 (2.8) at T4, 27.0 (2.8) at T5, 31.9 (2.8) at T6, 36.6 (2.8) at T7, and 43.0 (2.8) at T8, respectively.
At T2-T7, extensively trained and supervised lay interviewers administered interviews in private. The T8 data collection involved an internet-based self-administered questionnaire. Written informed consent was obtained from participants and their mothers in 1983, 1985–1986, and 1992, and from participants only in 1997, 2002, 2005–2006, and 2012–2013. The Institutional Review Board of _______ authorized the use of human subjects in this research study. Earlier waves of the study were approved by the Institutional Review Boards of the _______ and _______. Additional information regarding the study methodology is available in prior publications (e.g., Name deleted to protect the integrity of the review process, 1986).
Measures
Preventive Health Behaviors (2012/2013)
Use of Preventive Health Services
At T8, the participants responded to questions with regards to their frequency of the following doctor visits for a routine physical checkup in the past 5 years: (1) general practitioner/family doctor; (2) internist; (3) ophthalmologist/ optometrist; (4) dentist; (5) dermatologist; (6) urologist (for males only); and (7) obstetrician/ gynecologist (for females only). Each item was scored on a four-point scale: never (0), less than once a year (1), once a year (2), and two times a year or more (3). The mean (SD) of the preventive health services scale was 1.23 (0.53).
General Healthy Lifestyles
We selected three healthy lifestyle areas, i.e., eating habits, sleeping habits, and exercise. At T8, the participants responded to questions with regards to their (1) eating habits (6 items; alpha=.76; e.g., How often do you eat vegetables?; Clarke, O’Malley, Johnston, Schulenberg, & Lantz, 2009), (2) sleeping habits (4 items; alpha=.77; e.g., How often do you get at least 7 hours of sleep? Clarke et al., 2009), and (3) exercise (2 items, e.g., How often do you exercise vigorously? Clarke et al., 2009). Each item was scored on a six-point scale: never (0), seldom (1), sometimes (2), most days (3), nearly every day (4), and every day (5). We reversed the coding of the items which represent unhealthy lifestyles. The mean (standard deviation [SD]) was 3.12 (0.87), 3.09 (0.96), and 2.41 (0.97) for eating habits, sleeping habits, and exercise respectively.
For each lack of preventive health behaviors (i.e., underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise), a participant was assigned a score of 1 for the respective indicator variable if he/she scored 1 standard deviation below its sample mean. We then created a composite indicator variable, i.e., lack of preventive health behaviors. For this variable, a participant was assigned a score 1 if at least 2 of the component indicator variables (i.e., underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise) had a score of 1.
Cigarette Smoking (1983–2012/2013)
The cigarette smoking data were obtained from interviewer-administered questionnaires. At each follow-up wave (T2–T8), questions about tobacco use (adapted from the Monitoring the Future study; Johnston, O’Malley, Bachman, & Schulenberg, 2006) were asked. In order to measure the lifetime quantity and frequency of using tobacco from childhood to the early thirties, the questions used in the analyses asked about the frequency of using tobacco during the period from the last time point through the current time wave. Specifically, the questions used asked about the lifetime frequency and quantity of tobacco use in childhood and early adolescence for T2 (1983; prior to T2), the frequency and quantity of tobacco use during the past two years in adolescence for T3 (1985–1986; T2–T3), the frequency and quantity of tobacco use during the past five years in the early twenties for T4 (1992; T3–T4), the frequency and quantity of tobacco use during the past five years in the late twenties for T5 (1997; T4–T5), the frequency and quantity of tobacco use during the past five years in the late twenties and early thirties for T6 (2002; T5–T6), the frequency and quantity of tobacco use during the past five years in the mid thirties for T7 (2005–2006; T6–T7), and the frequency and quantity of tobacco use during the past five years in the early forties for T8 (2012/2013; T8). The measure of cigarette smoking at each time point had a scale coded as none (0), less than daily (1), 1–5 cigarettes a day (2), about half a pack a day (3), about a pack a day (4), and about 1.5 packs a day or more (5). The mean (SD) tobacco use scores at each point in time were 0.59 (1.10), 0.78 (1.31), 1.37 (1.63), 1.36 (1.62), 1.24 (1.65), 1.22 (1.73), and 0.95 (1.61) for T2–T8 respectively. The measure of cigarette smoking has been found to predict young adult psychiatric disorders (Name deleted to protect the integrity of the review process, 2002) and health problems (Name deleted to protect the integrity of the review process, 2004).
Control Variables
We included demographic factors such as gender (female=0; male=1), T2 age (years), and T2 family income ($US) as control variables. We also controlled for earlier personal attributes such as T2 depressive mood (5 items; alpha=0.75; e.g., “Over the last few years, how much were you bothered by feeling low in energy or slowed down?”; Derogatis, 1994), T2 self control (7 items; alpha=0.62; e.g., “I generally rely on careful reasoning in making up my mind.”; Name deleted to protect the integrity of the review process, 1990), T2 rebellion (8 items; alpha=0.81; e.g., “When rules get in my way, I sometimes ignore them.”; Smith, Fogg, & Simmons, 1979), and T2 delinquency (5 items; alpha=0.65; e.g., “How often have you gotten into a serious fight at school or work?”; Jessor, Graves, Hanson, & Jessor, 1968). In addition, T8 obesity status (Body Mass Index >29.9) was also controlled.
Analysis
Using the Mplus software (Muthén & Muthén, 2010) and the GMM approach (Muthén & Shedden, 1999), we extended our previous trajectory analyses (Name deleted to protect the integrity of the review process, 2011) by including the measure of cigarette smoking in the early forties (T8). We treated the dependent variable (cigarette smoking at each time point) as a censored normal variable. There were 806 participants who participated in the longitudinal study at least twice from 1983 (T2) onward. Among them, 51%, 71%, 85%, 93%, 97% and 100% participated in the study at least seven, six, five, four, three, and two points in time. We used all of these 806 participants in our GMM analyses and applied the full information maximum likelihood (FIML) approach for missing data. We set each of the trajectory polynomials to be cubic. We used the minimum Bayesian Information Criterion (BIC) to determine the number of trajectory groups. We did not consider groups with fewer than 3% of the sample because some investigators have cautioned against over-extraction of latent classes due to the presence of non-normal data (Bauer and Curran 2003). After extracting the latent classes, we assigned each participant to the trajectory group with the largest Bayesian posterior probability (BPP). For each of the trajectory groups, we created an indicator variable, which had a value of 1 if the participants had the largest BPP for that group and 0 otherwise.
Statistical Analysis Software (SAS) programs were then used to conduct χ2 tests to examine the general associations between lack of preventive health behaviors (including the composite index and each component) and the smoker trajectory groups. We also performed separate logistic regression analyses to investigate the associations between the probabilities of smoker trajectory group membership and lack of preventive health behaviors, controlling for gender, and T2 age, T2 family income, T2 depressive mood, T2 self control, T2 rebellion, T2 delinquency, and T8 obesity (N=548). The dependent variables were lack of preventive behaviors (i.e., the composite variable), underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise. Since specifying which trajectory group an individual belongs to is subject to error, we used the BPPs of belonging to each trajectory group as the independent variables (see Datta & Satten, 2000). The BPP of belonging to the nonuser trajectory group was chosen as the reference.
In addition, we directly categorized the mean smoking score (T2–T8) into three categories, i.e., heavy smokers (one standard deviation above the mean), non-smokers, and occasional/light smokers (i.e., neither non-smokers nor heavy smokers). We then performed separate logistic regression analyses using the indictor variables of heavy smokers and occasional/light smokers as the independent variables, controlling for the demographic and behavioral factors cited above. The non-smoking group was treated as the reference.
Results
Table 1 presents the descriptive statistics of the control variables used in the analysis. We compared the T8 participants (N=548) and the participants who did not participate in our study at T8 (N = 258). There was a higher percentage of females (55% in the sample of 548 participants vs. 39.7% in the sample of 258 participants at T2 but not T8; χ2(1) = 16.8, p-value < 0.001). There was no association between those included in the analysis as compared with those who were excluded from it with respect to age (t = −0.16, p-value = 0.87), T2 family income (t = −1.7, p-value = 0.1), and T2 depressive mood (t = −0.62, p-value = 0.53).
Table 1.
Descriptive Statistics of the Control Variables (N=548)
| Variables | Coding | Mean (SD), Median, or % |
|---|---|---|
| Gender | Female (0)–Male (1) | Male=45% |
| Age (1983) | Years | 14.4 (2.8) |
| Family Income (1983) | $US | $25,000 a |
| Depressive Mood (1983) | Not at all (1)–Extremely (5) | 2.1 (0.68) |
| Self Control (1983) | False (1)–True (4) | 2.78 (0.49) |
| Rebellion (1983) | False (1)–True (4) | 2 (0.56) |
| Delinquency (1983) | Never (1)–5 or more times (5) | 1.68 (0.7) |
| Obesity (2012–2013) | No (0)–Yes (1) | Obesity=32% |
Note:
median income.
Trajectories of Cigarette Smoking
We calculated solutions for the two-group trajectory (Likelihood Value = −5773; BIC = 11652; Entropy = 0.92), the three-group trajectory (Likelihood Value = −5563; BIC = 11266; Entropy = 0.88), the four-group trajectory (Likelihood Value = −5487; BIC = 11147; Entropy = 0.86), and the five-group trajectory (Likelihood Value = −5429; BIC = 11064; Entropy = 0.86). We chose the five-group solution, because the BIC value was lower than those for the four-group trajectory. Participants were then assigned to the cigarette smoking trajectory group that best depicted their marijuana use over time. The average classification probabilities for group membership ranged from 0.84 to 0.96, which indicate a satisfactory classification.
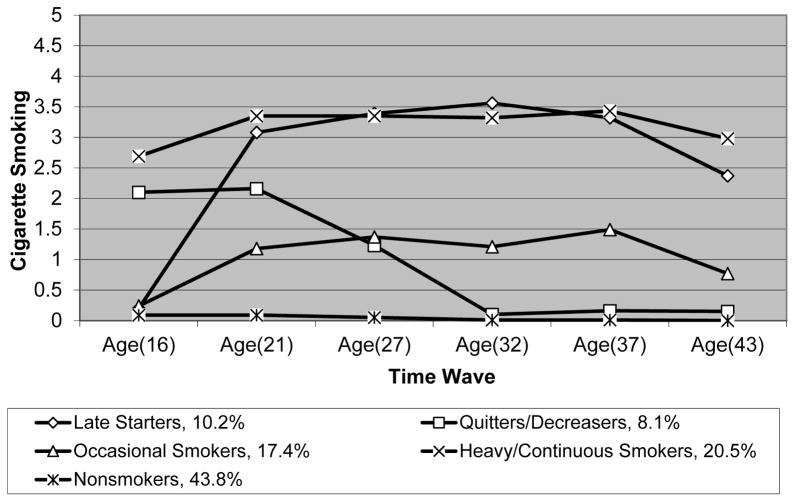
Figure 1 presents the five observed trajectories of cigarette smoking. The observed trajectory for a group was the average of cigarette smoking at each time point for participants assigned to the group. The trajectory smoking groups were named: heavy/continuous smokers (20.5%), late starters (10.2%), occasional smokers (17.4%), quitters/decreasers (8.1%), and nonsmokers (43.8%). As shown in Figure 1, the heavy/continuous smokers started smoking early, smoked about one pack a day in their late twenties and thirties, and tapered off to half a pack a day in their early forties. In contrast, the late starters started smoking in late adolescence but achieved the same amount of smoking (i.e., one pack a day) as the heavy/continuous smokers in the late twenties and during adulthood. The occasional smokers had an increasing frequency of smoking from adolescence to the early twenties and then stayed at an average level of less than daily smoking during adulthood. The quitters/decreasers started smoking as early as the heavy/continuous smokers and achieved the maximum level of smoking (i.e., daily smoking) in the early 20s. The participants then tapered off to non-smoking.
Fig. 1. Developmental trajectories of cigarette smoking extending from adolescence to age 43 (N=806).
Note: The smoking score categories are: 5.00=1.5 packs a day or more; 4.00=one pack per day; 3.00=1/2 pack per day; 2.00=1–5 cigarettes a day; 1.00=less than daily smoking; 0.00=none.
Trajectories of Cigarette Smoking as Predictors of T8 Lack of Preventive Health Behaviors
Table 2 presents the percentages of the original measures of preventive health service use and healthy (unhealthy) lifestyles. Table 3 presents the percentages of lack of preventive health behaviors for the whole sample and by the smoker trajectory groups. The results of the χ2 tests indicated that the associations between the composite index and each component of the lack of preventive health behaviors and the smoker trajectory groups were statistically significant (p<.05). Among the participants, heavy/continuous smokers had the highest percentages of unhealthy eating habits and poor sleeping habits, while later starters had the highest percentage of underuse of preventive health services and quitters/decreasers had the highest percentage of lack of exercise.
Table 2.
Percentagesof Preventive Health Service Uses and Healthy (Unhealthy) Lifestyles (N=548).
| Items | Never | Less than once a Year | Once a year | 2 times a year or more | ||
|---|---|---|---|---|---|---|
| In the past 5 years how often have you visited the following doctors for a routine physical checkup? | ||||||
| General practitioner/family doctor | 10.4% | 24.2% | 42.5% | 22.9% | ||
| Internist | 62.7% | 12.9% | 15.3% | 9.2% | ||
| Ophthalmologist/optometrist | 30.5% | 32% | 33.6% | 3.9% | ||
| Dentist | 8.4% | 14.7% | 21.3% | 55.7% | ||
| Dermatologist | 71% | 17.1% | 9.4% | 2.6% | ||
| Urologist (for males only) | 84.9% | 9% | 4.5% | 1.6% | ||
| Obstetrician (OB)/Gynecologist (for females only) | 11% | 14.4% | 61.5% | 13% | ||
| Never | Seldom | Sometimes | Most days | Nearly every day | Every day | |
| Eating habits: How often do you | ||||||
| eat breakfast? | 3.5% | 16.1% | 17% | 14.3% | 15.8% | 33.3% |
| eat at least some green vegetables? | 1.1% | 5.1% | 20.7% | 27.1% | 22.2% | 23.8% |
| eat at least some fruits? | 1.1% | 10.1% | 28.2% | 22.2% | 16.3% | 22.2% |
| avoid high-fat foods? | 5.7% | 13.2% | 34.1% | 27% | 14.9% | 5.1% |
| eat foods high in sugar? 1 | 2.4% | 25.5% | 47.8% | 15.6% | 5.7% | 3.1% |
| drink beverages high in added sugar? 1 | 1.1% | 5.1% | 20.7% | 27.1% | 22.2% | 23.8% |
| Sleeping habits: How often do you | ||||||
| get at least seven hours of sleep? | 3.3% | 13.6% | 24.7% | 26.2% | 20.2% | 12.1% |
| get less sleep than you should? 1 | 5.7% | 21.5% | 38% | 19.6% | 9% | 6.4% |
| have trouble falling asleep? 1 | 18.7% | 35.4% | 30.6% | 8.2% | 2.6% | 4.6% |
| have trouble staying asleep? 1 | 14.7% | 31.9% | 34.3% | 11% | 4.2% | 3.9% |
| Exercising habits: How often do you | ||||||
| exercise vigorously? | 16.1% | 28.9% | 32.6% | 14.5% | 6.2% | 1.7% |
| engage in moderate physical activity? | 1.8% | 4.4% | 29% | 28.1% | 18.5% | 18.2% |
Code was reversed when creating the healthy general lifestyle scales.
Table 3.
Percentages of Lack of Preventive Health Behaviors for the Whole Sample and by Smoking Trajectory Groups and χ2 tests (N=548).
| Variables | The Whole Sample | Heavy/Continuous Smokers | Late Starters | Occasional Smokers | Quitters/Decreasers | Non-smokers | χ2 Test (degree of freedom =4) |
|---|---|---|---|---|---|---|---|
| Lack of preventive health behaviors | 15.3% | 27.4% | 25.9% | 15.5% | 9.4% | 8.9% | 26.5*** |
| Underuse of preventive health services | 18.6% | 22.6% | 34.5% | 13.1% | 17% | 15.4% | 14.3** |
| Unhealthy eating habits | 16.8% | 33% | 29.3% | 13.1% | 7.6% | 10.1% | 38.4*** |
| Poor Sleeping habits | 14.1% | 25.5% | 13.8% | 15.5% | 7.6% | 10.1% | 16.6** |
| Lack of exercise | 12% | 19.8% | 10.3% | 7.1% | 20.8% | 8.9% | 14.2** |
Note:
p<.001;
p<.01;
For the composite indicator variable of lack of preventive health behaviors, a participant was assigned a score 1 if at least 2 of the component indicator variables (i.e., underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise) had a score of 1.
Table 4 presents the results of the multivariate logistic regression analyses. When controlling for the demographic factors and adolescent behavioral factors: (1) as compared to the probability of belonging to the nonsmoker trajectory group, a higher probability of belonging to the heavy/continuous smoker trajectory group was statistically significantly associated with a higher likelihood of lack of preventive health behaviors, unhealthy eating habits, poor sleeping habits, and lack of exercise (Adjusted Odds Ratio [A.O.R.] = 3.49; A.O.R. = 3.41; A.O.R.=2.55; and A.O.R.=2.61, respectively). A higher probability of belonging to the late starter trajectory group was significantly associated with a higher likelihood of lack of preventive health behaviors, underuse of preventive health services, and unhealthy eating habits (A.O.R. = 4.02; A.O.R. = 2.94; A.O.R. = 4.94, respectively); a higher probability of belonging to the quitters/decreasers was significantly associated with a higher likelihood of lack of exercise (A.O.R. = 3.00); (2) as compared to the probability of belonging to the quitter/decreaser trajectory group, a higher probability of belonging to the heavy/continuous smoker trajectory group was significantly associated with a higher likelihood of lack of preventive health behaviors, unhealthy eating habits, and poor sleeping habits (A.O.R. = 3.51; A.O.R. = 6.58; A.O.R. = 4.13; respectively; data not shown in Table 4); a higher probability of belonging to the late starter trajectory group was significantly associated with a higher likelihood of lack of preventive health behaviors and unhealthy eating habits (A.O.R. = 4.04; A.O.R. = 9.52, respectively; data not shown in Table 4); and (3) as compared to the probability of belonging to the occasional smoker trajectory group, a higher probability of belonging to the heavy/continuous smoker trajectory group was significantly associated with a higher likelihood of underuse of preventive health services, unhealthy eating habits, and lack of exercise (A.O.R. = 2.93; A.O.R. = 3.31; A.O.R. = 3.28, respectively; data not shown in Table 4); a higher probability of belonging to the late starter trajectory group was significantly associated with a higher likelihood of underuse of preventive health services and unhealthy eating habits (A.O.R. = 5.61; A.O.R. = 4.76, respectively; data not shown in Table 4); a higher probability of belonging to the quitters/decreasers was significantly associated with a higher likelihood of lack of exercise (A.O.R. = 3.77; data not shown in Table 4).
Table 4.
Logistic Regressions: Trajectories of Cigarette Smoking from Adolescence to Mean Age 37 as Related to Underuse of Preventive Health Services and General Unhealthy Lifestyles Among Men and Women in the Early Forties (N=548).
| Independent Variables | Composite Index | Component Indicator Variables | |||
|---|---|---|---|---|---|
| Lack of Preventive Health Behaviors | Underuse of Preventive Health Services | Unhealthy Eating Habits | Poor Sleeping Habits | Lack of Exercise | |
| A.O.R. (95% C.I.) (15.3%)a | A.O.R. (95% C.I.) (18.6%)a | A.O.R. (95% C.I.) (16.8%)a | A.O.R. (95% C.I.) (14.1%)a | A.O.R. (95% C.I.) (12%)a | |
| BPP of Heavy/Continuous Smokers | 3.49 (1.71–7.12)*** | 1.53 (0.76–3.09) | 3.41 (1.75–6.67)*** | 2.55 (1.22–5.31)* | 2.61 (1.21–5.63)* |
| BPP of Late Starters | 4.02 (1.73–9.34)** | 2.94 (1.31–6.57)* | 4.94 (2.18–11.20)*** | 1.38 (0.50–3.80) | 1.20 (0.42–3.44) |
| BPP of Quitters | 1.00 (0.32–3.11) | 0.94 (0.36–2.46) | 0.52 (0.15–1.77) | 0.62 (0.18–2.13) | 3.00 (1.17–7.71)* |
| BPP of Occasional Smokers | 1.64 (0.71–3.78) | 0.52 (0.23–1.20) | 1.03 (0.43–2.46) | 2.22 (0.98–5.03) | 0.80 (0.28–2.26) |
Note:
A.O.R.= Adjusted Odds Ratio; C.I.=Confidence Interval; BPP = Bayesian posterior probability;
p<.001;
p<.01;
p<0.05;
percentage of the sample that the dependent variable = 1;
The following variables were included as control variables in the regression analysis: gender, T2 age, T2 family income, T2 depressive mood, T2 self-control, T2 rebellion, T2 delinquency, and T8 obesity;
BPP of belonging to the non-user trajectory group serves as the reference;
For the composite indicator variable of lack of preventive health behaviors, a participant was assigned a score 1 if at least 2 of the component indicator variables (i.e., underuse of preventive health services, unhealthy eating habits, poor sleeping habits, and lack of exercise) had a score of 1.
In addition, using the three categories (i.e., heavy smokers, occasional/light smokers, and non-smokers) directly derived from the mean smoking score (T2–T8), the results showed that, as compared to the non-smokers, heavy smokers had significantly higher likelihood of lack of preventive health behaviors, unhealthy eating habits, and poor sleeping habits. However, occasional/light smokers were not significantly different from non-smokers in terms of these outcomes.
Discussion
This study is among the first to describe the long-term trajectories of cigarette smoking and its relation to lack of preventive health behaviors using prospective, longitudinal follow-up data covering 29 years of multiple developmental stages, including early adolescence, late adolescence, emerging adulthood, young adulthood, and early midlife. Overall, our hypothesis was partially supported.
With regard to the smoking trajectory groups, Chassin et al. (2008) identified nine trajectory groups. Costello, Dierker, Jones, and Rose (2008) identified six trajectory groups, and Riggs, Chou, Li, and Pentz (2007) identified four trajectory groups. In our earlier trajectory analyses (Name deleted to protect the integrity of the review process, 2011), we found five trajectory groups. The trajectory groups vary in terms of their quantity of smoking, as well as in terms of the growth, stability, or decline in smoking over time. Similar to the national data (Farley, Dalal, Mostashari, and Frieden, 2010; Liu, 2016; Moore & Thompson, 2015; Schoenborn, Adams, & Peregoy, 2013), we found evidence of underuse of preventive health services. In addition, many of the participants had relatively unhealthy lifestyles. Particularly, 46% of the participants drank beverages high in added sugar nearly every day or every day; 41.6% reported typically sleeping less than 7 hours a day; and 45% of the participants never or seldom exercised vigorously.
The present research provides evidence for a relationship between the trajectories of heavy continuous smoking and late starting smoking from adolescence to late 30s and the likelihood of lack of preventive health behaviors, as compared with the non-user trajectory group and quitter/decreaser trajectory group. These associations were maintained despite control on a number of demographic and behavioral factors, including gender, age, family income of origin, depressive mood, self-control, rebellion, and delinquency in adolescence, and current obesity status. In addition, even though the results were similar, the GMM approach has an advantage over the approach using the mean scores of lifetime cigarette smoking in terms of testing the associations between distinct developmental patterns of cigarette smoking and later lack of preventive health behaviors.
Operating within a public health framework, the heavy continuous smoker trajectory group and the late starter trajectory group are significant targets for promoting preventive health behaviors. Several psychosocial factors may account for the associations. First, cigarette use has been linked to adverse life events, including unemployment (De Vogli & Santinello, 2005), loss of health insurance coverage, and financial stress (Siahpush, Borland, & Scollo, 2003), which, in turn, may be associated with lack of preventive health behaviors. Using data from a survey of the civilian, non-institutionalized population of adults (age 18 and older) in the United States between 1987 and 2010, Tefft and Kageleiry (2014) found that a 1% point increase in the state-level unemployment rate is associated with a 1.58 percent decrease in use of preventive health services. Women and economically disadvantaged populations are particularly vulnerable to macroeconomic fluctuations. Second, health beliefs may serve as a mediator between smoking and lack of preventive health behaviors (Mantler, 2013; Rosenstock, 1974). Health beliefs are the values, attitudes and knowledge that individuals possess regarding health and healthcare which influence their perception of their need for preventive healthcare and preventive health behaviors. An important step for future research would be to determine whether life stressors and health beliefs serve to mediate the association of trajectories of cigarette smoking and underuse of preventive health services and general unhealthy lifestyles. In addition, we did not find significant differences between heavy continuous smoking and late starting smoking in terms of lack of preventive health behaviors.
With regard to the quitters/decreasers as compared to their counterparts who are chronic cigarette smokers, cigarette smokers who quit may be more likely to be more effective in using coping strategies (Brodbeck, Bachmann, & Znoj, 2013; Frosch, Dierker, Rose, & Waldinger, 2009), and consequently, less likely to underuse preventive health services and less likely to have general unhealthy lifestyles (Kwasnicka, Presseau, White, & Sniehotta, 2013). Another possible mechanism is family social support (Westmaas, Bontemps, & Bauer, 2010). Individuals who quit smoking cigarettes may be more likely to experience emotionally rewarding and supportive relationships, which, in turn, may be associated, in part, with a lower likelihood of underuse of preventive health services and having general unhealthy lifestyles. Wang, Pbert, and Lemon (2014) found that, among adult employees, friend and coworker support for healthy eating and family support for physical activity predicted improved weight management. Several other factors may serve to mediate the relationship between cigarette smoking and lack of preventive health behaviors. Individuals who stop smoking may experience fewer psychological conditions (e.g., depression), which, in turn, are associated with a lower likelihood of lack of preventive health behaviors. Several studies have also found a direct association between a history of depressive mood and later underuse of preventive medical services (Bogner & Wittink, 2004; Pirraglia, Sanyal, Singer, & Ferris, 2004). For example, Pirraglia et al. (2004) reported that patients with depressive symptoms are less likely to adhere to the preventive health recommendations for breast cancer screening.
With one exception (i.e., lack of exercise), the quitters/decreasers were similar to the non-smokers in terms of lack of preventive health behaviors. The occasional cigarette smokers in the present study were also similar to the non-smokers in terms of lack of preventive health behaviors. The reasons for these findings are not clear at the present time.
Limitations and Strengths
Although this study made several novel contributions to the literature, several limitations must be acknowledged. First, while our sample includes socioeconomic diversity, it lacked a representation of ethnic minorities. We can only generalize our findings to a population of primarily white adolescents and adults. It is well-known that ethnicity is related to underuse of preventive health services. Consequently, non-white users are likely to have different experiences of underuse of preventive health services and/or general unhealthy lifestyles. Future research with diverse samples may enhance the generalizability of the findings. Second, caution must be exercised in the interpretation of the results. Due to a relatively small sample size and relatively large time span between waves, we may have missed trajectory patterns (or periods) of cigarette smoking shorter than the time intervals between waves of data collection. Future research should include a larger sample observed with shorter intervals between waves of data collection. Third, although we included a number of confounding factors in the analyses, we were not able to include other factors which may explain the associations between the trajectories of cigarette smoking and underuse of preventive health services and general unhealthy lifestyles. For example, we did not include life events and genetic factors. Fourth, the present study does not enable us to provide inferences regarding causality. Future research should focus on assessing the causal ordering of the trajectories of cigarette smoking and adult underuse of preventive health services.
Despite these limitations, this study has several strengths. First, the participants were followed from the second to the fifth decades of life. The age range of this study spans several developmental stages. Second, the study takes a life-course perspective, which allows us to time-order the associations between the trajectories of cigarette smoking and lack of preventive health behaviors. Third, we controlled for a wide array of behavioral and social factors.
Conclusions and Implications
In sum, this is the first research to examine the relation between trajectories of cigarette smoking, covering several developmental stages, and lack of preventive health behaviors. As such, these developmental stages offer promising windows of opportunity for prevention and treatment where access to smoking cessation programs, particularly among the heavy chronic cigarette smokers and late starters may decrease the potentially adverse effect on use of preventive health services and general unhealthy lifestyles. We provide a snapshot of a few mechanisms that may explain the association between trajectories of cigarette smoking and lack of preventive health behaviors. Our results suggest that interventions that address the underuse of preventive health services and general unhealthy lifestyles may also benefit from attention directed at the use of cigarettes or cigarette smoking.
Acknowledgments
This research was supported by NIH Grants XXXXX and XXXXX from the National Institute on Drug Abuse awarded to Dr. XXXXX.
Glossary
- Growth mixture modeling (GMM)
GMM is a statistical modeling technique that can be used to identify unobserved differences in growth trajectories. GMM explores qualitative differences in longitudinal growth trajectories, which are based on differences in growth parameter means (e.g., intercept and slope)
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for over extraction of latent trajectory classes. Psychological Methods. 2003;8:338–363. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, … Cecchini M. Priority actions for the non-communicable disease crisis. The Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- Bogner HR, Wittink MN. Editorial: Depression as a risk factor for underuse of mammography. Journal of Womens Health. 2004;13(6):739–742. doi: 10.1089/1540999041783136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodbeck J, Bachmann MS, Znoj H. Distinct coping strategies differentially predict urge levels and lapses in a smoking cessation attempt. Addictive behaviors. 2013;38(6):2224–2229. doi: 10.1016/j.addbeh.2013.02.001. [DOI] [PubMed] [Google Scholar]
- Bryan L, Westmaas L, Alcaraz K, Jemal A. Cigarette smoking and cancer screening underutilization, by State, BRFSS 2010. Nicotine & Tobacco Research. 2014;16:1183–1189. doi: 10.1093/ntr/ntu047. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Health, United States, 2008. Hyatsville, MD: U.S. Department of Health and Human Services; 2008a. Retrieved from http://www.cdc.gov/nchs/data/hus/hus08.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008b;57:1226–1228. [PubMed] [Google Scholar]
- Chao A, Connell CJ, Cokkinides V, Jacobs EJ, Calle EE, Thun MJ. Underuse of screening sigmoidoscopy and colonoscopy in a large cohort of US adults. American Journal of Public Health. 2004;94(10):1775–1781. doi: 10.2105/ajph.94.10.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson C, Seo D, Sherman SJ, Macy J, Wirth RJ, et al. Multiple trajectories of cigarette smoking and the intergenerational transmission of smoking: A multigenerational, longitudinal study of a midwestern community sample. Health Psychology. 2008;27:819–828. doi: 10.1037/0278-6133.27.6.819. [DOI] [PubMed] [Google Scholar]
- Clarke PJ, O’Malley PM, Johnston LD, Schulenberg JE, Lantz P. Differential trends in weight-related health behaviors among American young adults by gender, race/ethnicity, and socioeconomic status: 1984–2006. American journal of public health. 2009;99(10):1893–1901. doi: 10.2105/AJPH.2008.141317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello DM, Dierker LC, Jones BL, Rose JS. Trajectories of smoking from adolescence to early adulthood and their psychosocial risk factors. Health Psychology. 2008;27:811–818. doi: 10.1037/0278-6133.27.6.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallongeville J, Marécaux N, Fruchart JC, Amouyel P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: a meta-analysis. The Journal of nutrition. 1998;128(9):1450–1457. doi: 10.1093/jn/128.9.1450. [DOI] [PubMed] [Google Scholar]
- Datta S, Satten GA. Estimating future stage entry and occupation probabilities in a multistage model based on randomly right-censored data. Statistics and Probability Letters. 2000;50:89–95. [Google Scholar]
- Derogatis LR. Symptom Checklist 90-R: Administration, scoring, and procedures manual. 3. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- De Vogli R, Santinello M. Unemployment and smoking: does psychosocial stress matter? Tobacco Control. 2005;14(6):389–395. doi: 10.1136/tc.2004.010611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. American Journal of Preventive Medicine. 2010;38(6):600–609. doi: 10.1016/j.amepre.2010.02.016. [DOI] [PubMed] [Google Scholar]
- Frieden TR. Use of selected clinical preventive services among adults--United States, 2007–2010. Morbidity and Mortality Weekly Report. 2012;61:1–2. [PubMed] [Google Scholar]
- Frosch ZA, Dierker LC, Rose JS, Waldinger RJ. Smoking trajectories, health, and mortality across the adult lifespan. Addictive behaviors. 2009;34(8):701–704. doi: 10.1016/j.addbeh.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Butterworth S, Patel K, Mishra G, Kuh D. Reduced midlife physical functioning among never married and childless men: Evidence from the 1946 British Birth Cohort Study. Aging Clinical and Experimental Research. 2009;21(2):174–181. doi: 10.1007/bf03325226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessor R, Graves TD, Hanson RC, Jessor SL. Society, Personality, and Deviant Behavior: A Study of a Tri-Ethnic Community. New York, NY: Holt, Rinehart & Winston; 1968. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development. New York: Academic Press; 1977. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future, National Survey Results on Drug Use, 1975–2006: Volume I, secondary school students. Bethesda, MD: National Institute on Drug Abuse; 2006. (NIH publication no. 06–5883) Retrieved from Monitoring the Future website. http://www.monitoringthefuture.org/pubs/monographs/vol1_2006.pdf. [Google Scholar]
- Katon WJ, Russo JE, Heckbert SR, Lin EH, Ciechanowski P, Ludman E, … Von Korff M. The relationship between changes in depression symptoms and changes in health risk behaviors in patients with diabetes. International journal of geriatric psychiatry. 2010;25(5):466–475. doi: 10.1002/gps.2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwasnicka D, Presseau J, White M, Sniehotta FF. Does planning how to cope with anticipated barriers facilitate health-related behaviour change? A systematic review. Health psychology review. 2013;7(2):129–145. [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, … Aryee M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet. 2013;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR. Morbidity and mortality weekly report. 2016;65 doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- Lohse T, Rohrmann S, Bopp M, Faeh D. Heavy smoking is more strongly associated with general unhealthy lifestyle than obesity and underweight. PloS one. 2016;11(2):e0148563. doi: 10.1371/journal.pone.0148563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantler T. A systematic review of smoking youths’ perceptions of addiction and health risks associated with smoking: Utilizing the framework of the health belief model. Addiction Research & Theory. 2013;21(4):306–317. [Google Scholar]
- McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. Journal of health and social behavior. 1990:162–172. [PubMed] [Google Scholar]
- Miller JW, King JB, Joseph DA, Richardson LC. Centers for Disease Control and Prevention (CDC) Breast cancer screening among adult women—Behavioral risk factor surveillance system, United States, 2010. Morbidity and Mortality Weekly Report. 2012;61(Suppl):46–50. [PubMed] [Google Scholar]
- Moore LV, Thompson FE. Adults meeting fruit and vegetable intake recommendations—United States, 2013. MMWR. Morbidity and mortality weekly report. 2015;64(26):709–713. [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. (Retrieved from http://www.statmodel.com/download/usersguide/Mplus%20Users%20Guide%20v6.pdf) [Google Scholar]
- Muthén B, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annual review of sociology. 2010;36:349. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Archives of internal medicine. 1995;155(7):734–737. [PubMed] [Google Scholar]
- Pirraglia PA, Sanyal P, Singer DE, Ferris TG. Depressive symptom burden as a barrier to screening for breast and cervical cancers. Journal of Womens Health. 2004;13(6):731–738. doi: 10.1089/jwh.2004.13.731. [DOI] [PubMed] [Google Scholar]
- Pope SK, Sowers M, Welch GW, Albrecht G. Functional limitations in women at midlife: The role of health conditions, behavioral and environmental factors. Womens Health Issues. 2001;11:494–502. doi: 10.1016/s1049-3867(01)00089-5. [DOI] [PubMed] [Google Scholar]
- Riggs NR, Chou C, Li C, Pentz MA. Adolescent to emerging adulthood trajectories: When do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine & Tobacco Research. 2007;9:1147–1154. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. The health belief model and preventive health behavior. Health Education & Behavior. 1974;2(4):354–386. [Google Scholar]
- Schoenborn CA, Adams PF, Peregoy JA. Health behaviors of adults: United States, 2008–2010. National Center for Health Statistics. Vital Health Stat. 2013;10(257) [PubMed] [Google Scholar]
- Siahpush M, Borland R, Scollo M. Smoking and financial stress. Tobacco Control. 2003;12(1):60–66. doi: 10.1136/tc.12.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaff MM. Sense of control and health: A dynamic duo in the aging process. In: Aldwin CM, Park CL, Spiro A, editors. Handbook of health psychology and aging. New York: Guilford Press; 2007. pp. 186–209. [Google Scholar]
- Smith GE, Fogg CP, Simmons R. Psychological antecedents of teen-age drug use. In: Simmons R, editor. Research in Community and Mental Health: An Annual Compilation of Research. Vol. 1. Greenwich, CT: JAI Press; 1979. pp. 87–120. [Google Scholar]
- Tefft N, Kageleiry A. State-Level unemployment and the utilization of preventive medical services. Health services research. 2014;49(1):186–205. doi: 10.1111/1475-6773.12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. Retrieved from http://www.surgeongeneral.gov/library/tobaccosmoke/index.html. [PubMed] [Google Scholar]
- Wang ML, Pbert L, Lemon SC. Influence of family, friend and coworker social support and social undermining on weight gain prevention among adults. Obesity. 2014;22(9):1973–1980. doi: 10.1002/oby.20814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmaas JL, Bontemps–Jones J, Bauer JE. Social support in smoking cessation: reconciling theory and evidence. Nicotine & tobacco research. 2010;12(7):695–707. doi: 10.1093/ntr/ntq077. [DOI] [PubMed] [Google Scholar]
- Wills TA, Dishion TJ. Temperament and adolescent substance abuse: A transactional analysis of emerging self-control. Journal of Clinical Child and Adolescent Psychiatry. 2004;33:69–81. doi: 10.1207/S15374424JCCP3301_7. [DOI] [PubMed] [Google Scholar]
- Name deleted to protect the integrity of the review process (2011).
- Name deleted to protect the integrity of the review process (2002).
- Name deleted to protect the integrity of the review process (2004).
- Name deleted to protect the integrity of the review process (2012).
- Name deleted to protect the integrity of the review process (1986).
- Name deleted to protect the integrity of the review process (1990).