Figure 2.
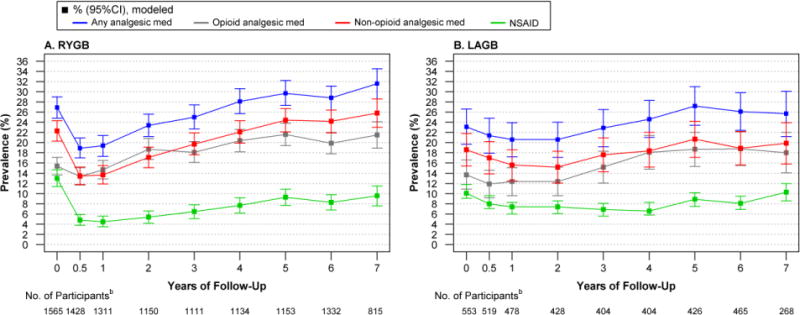
Modeled Prevalence of Prescribed Analgesic Use in Relation to Bariatric Surgery, by Surgical Procedurea
A. Among participants who underwent RYGB, the prevalence of any prescription analgesic use, and specifically non-opioid analgesic use, increased over time (P for both <.001), first decreasing from baseline to 6 months (P for both<.001) and then increasing such that year-7 prevalence was higher than baseline (P for both<0.05). The prevalence of NSAID use followed a quadratic trend (P<.001), decreasing from baseline to 6 months (P<.001) before increasing over time. However, post-surgery prevalence remained lower than baseline through year-7 (P=0.01). B. Among participants who underwent LAGB, the prevalence of any prescription analgesic use increased over time (P=0.01), but was not significantly different from baseline at 6 months (P=0.45) or year-7 (P=0.50). The prevalence of non-opioid analgesic use did not differ over time (p=0.34) or differ from baseline at 6-month (P=0.50) or 7-year (P=0.83). The prevalence of NSAID use followed a quadratic trend over time (P=0.01) but was not significantly different from baseline at 6 months (P=0.23) or year-7 (P=0.99).
Abbreviations: Laparoscopic adjustable gastric banding (LAGB); non-steroidal anti-inflammatory drugs (NSAID); Roux-en-Y gastric bypass (RYGB).
aModels were adjusted for baseline factors related to missing follow-up data (i.e., site, age, smoking status). Observed and modeled data for these and “other” procedures is reported in eTables 5 and 6 [Supplement], respectively. bData are based on observations until January 31, 2015; data collection ended before 429 RYGB and 173 LAGB participants were eligible for a 7 year assessment.
