Abstract
Melkersson-Rosenthal Syndrome (MRS) is a rare disorder consisting of a triad of persistent or recurrent orofacial edema, relapsing facial paralysis and fissured tongue. It is rarely possible to observe all aspects of the classical triad at the same time, since these symptoms may appear in different times of life cycle. The most common symptom is orofacial edema. Although etiology of MRS is unclear, various factors such as infections, genetic predisposition, immune deficiency, food intolerance and stress have been held responsible. MRS is diagnosed based on clinical features. This case report describes a 39 years old male patient with recurrent swelling of the upper lip. Clinical examinations showed classical triad of MRS. The diagnosis and treatment procedures were presented with special emphasis to the clinical features of this rare condition.
Keywords: Melkersson-Rosenthal Syndrome, orofacial edema, fissured tongue, steroid use
Introduction
Melkersson Syndrome was first described in 1928 as peripheral facial paralysis and swelling of lips. In 1931, Rosenthal completed the triad by adding the presence of fissural tongue. The classical form of the Melkersson Rosenthal Syndrome (MRS) consists of the clinical triad of recurring facial nerve paralysis, swelling of one or both lips and fissural tongue (1). Cases displaying the entire triad are very rare. The mono-symptomatic or oligo-symptomatic form is more common. Presence of granulomatous cheilitis in the biopsy together with one or two of these clinical findings could be sufficient for MRS diagnosis (2). The characteristic histopathological features of MRS include granulomas with epithelioid cells, Langerhans type giant cells with multiple nuclei, perivascular mononuclear infiltration, non-caseating granulomas, lymphedema and fibrosis (3). It can be difficult to detect these features; however, their absence should not exclude the MRS diagnosis (4, 5). Since MRS is a clinical syndrome, histopathologic findings are not required for diagnosis. While biopsy helps the diagnosis, it is also helpful in the differential diagnosis of Crohn disease and sarcoidosis (6). Diagnosis is mostly based on clinical findings (1, 7). In this case report, a patient with MRS who had applied with complaints related to recurring swelling of the upper lip is presented.
Case Report
39 years-old male patient who had no systemic diseases and regular drug use applied to the Oral Diagnosis Clinic, Faculty of Dentistry, Gazi University, with painless and recurring swelling of the right side of his upper lip. Patient’s history revealed that he had suffered facial paralysis on the left side of his face many years ago. During extra-oral examination, swelling of the right side of the upper lip, cheilitis and asymmetry were observed. The patient has reported that the swelling in the upper lip had repeated with certain intervals (Figure 1). During intraoral examination it was observed that the patient had fissural tongue (Figure 2).
Figure 1.

(a) Swelling and asymmetry in the right side of the upper lip of the patient, (b) Cheilitis in the right side of the upper lip.
Figure 2.

Patient’s fissural tongue.
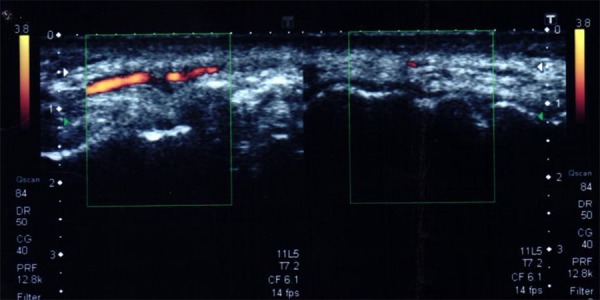
Ultrasound image was taken to exclude any possible pathology in the right side of the upper lip of the patient (Figure 3).
Figure 3.

Upper lip ultrasonography of the patient, gray scale: thickness thought to be consistent with the edema-inflammation of the nasolabial subcutaneous soft tissue on the right side, and the increase of blood supply together with the increase in the echogenicity observed in the Doppler examination.
Patient was consulted with the Dermatology Department, Faculty of Medicine, Gazi University and he was diagnosed with Melkersson Rosthenthal Syndrome based on the clinical and radiological findings. Oral corticosteroid therapy was administered to the patient for 26 days in total, with doses of 80 g in the first five days, 60 g in the following seven days, 40 g for the second seven days and 20 g in the last seven days. Swelling of the lip was disappeared after the steroid therapy (Figure 4).
Figure 4.
Clinical photograph of the patient after steroid therapy of 26 days.
Discussion
MRS is a rare disease characterized with a clinical triad consisting of permanent or recurring orofacial edema, recurring facial paralysis and fissural tongue. Diagnosis and treatment of this disease is difficult (8) since its etiology is not clear. Some authors suggest a genetic tendency (with autosomal dominant inheritance). In addition, allergic reactions against cobalt or some food stuff including monosodium glutamate, lymphogranulomatosis, paradental infections, tonsillitis, adenoid hypertrophy, viral infections including herpes simplex, and other bacterial or viral infections have been considered as causative factors. However, there is still no evidence showing that this disease has whether infective, allergic or hereditary origin (9).
Classical triad of MRS can only be observed in 8% to 18% of the patients, which makes it difficult to diagnose this condition (10, 11). All clinical findings can be seen all at once or at different times. Presence of at least one of the findings of idiopathic facial paralysis or fissural tongue together with permanent or recurring orofacial edema is sufficient for MRS diagnosis (10, 12, 13, 14). Even though our patient has suffered facial paralysis years ago, all the elements of the characteristic triad were observed.
The most frequent finding of MRS is acute, diffuse, painless and non-pitting orofacial edema which is most frequently seen on lips (10, 11, 15, 16). The upper lip is involved more frequently. Edema has a tendency for recurrence and usually disappears within few hours to few weeks (3, 17). MRS resembles angioedema, but it can be differentiated with the lack of response to antihistaminic drugs, tendency to last longer and by causing fibrosis in the involved tissues (18). Fissures can be observed in the central area (central cheilitis), corners of the mouth (angular cheilitis) or other areas of the involved lip (19). In our patient, cheilitis was seen on the right side of the upper lip together with swelling. The second characteristic finding of MRS is facial paralysis which can be observed in 30% to 35% of the patients (20). Paralysis can be transient, or can become permanent in time. It can be unilateral as well as bilateral or partial. The paralysis has been related either to the pressure of the edema on the nerve passing through the facial canal within the temporal bone or the granulomatous infiltration of the nerve (19, 21). The facial paralysis related to MRS may appear after months or years before or after the orofacial edema (17). According to patient’s history, he had experienced facial paralysis years ago which was healed completely. The third finding of MRS is the fissural tongue. Since fissural tongue is a widespread abnormality in the society, it is of lesser importance in the MRS diagnosis (22). Fissural tongue was also observed in our patient. Other findings of MRS can be listed as trigeminal neuralgia, ocular palsy, paresthesia, dysfunction of the lacrimal and saliva glands, migraine, keratitis, increases of secretions and psychological episodes (19, 23).
Although the disease can be controlled with treatment, it can recur in the future (24). Edema in the orofacial area can be cured or recede with the systemic use of steroids or intra-lesional corticosteroid administration (25, 26). It has been reported that in most patients idiopathic facial paralysis can heal spontaneously within the first three weeks (27).
Conclusion
Diagnosis of MRS is difficult as it is a rare disease. Its most frequent finding is the edema in the orofacial area. Dentists should keep the MRS in mind for the patients who have recurrent or permanent swelling in lips, and they should refer them to relevant departments for consultation.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
This case report was presented as a poster at the 17th International Congress on Oral Pathology and Medicine: Joint Meeting with the British Society for Oral&Maxillofacial Pathology, May 25-30, 2014, Harbiye Military Museum and Cultural Centre, Istanbul, Turkey.
References
- 1.Ang KL, Jones NS. Melkersson-rosenthal syndrome. J Laryngol Otol. 2002;116(5):386–388. doi: 10.1258/0022215021910861. [DOI] [PubMed] [Google Scholar]
- 2.Dodi I, Verri R, Brevi B, Bonetti L, Balestrier A, Saracino A, Akamin R, Izzi G C, Vanelli M, Sesenna E. A monosymptomatic melkersson-rosenthal syndrome in an 8-year old boy. Acta Biomed. 2006;77(1):20–23. [PubMed] [Google Scholar]
- 3.Pisanty S, Sharav Y. The melkersson-rosenthal syndrome. Oral Surg Oral Med Oral Pathol. 1969;27(6):729–733. doi: 10.1016/0030-4220(69)90139-X. [DOI] [PubMed] [Google Scholar]
- 4.Greene RM, Rogers RS. Melkersson-rosenthal syndrome: A review of 36 patients. J Am Acad Dermatol. 1989;21(6):1263–1270. doi: 10.1016/S0190-9622(89)70341-8. [DOI] [PubMed] [Google Scholar]
- 5.Sakuntabhai A, MacLeod RI, Lawrence CM. Intralesional steroid injection after nerve block anesthesia in the treatment of orofacial granulomatosis. Arch Dermatol. 1993;129(4):477–480. doi: 10.1001/archderm.1993.01680250089013. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro M, Peters S, Spinelli HM. Melkersson-rosenthal syndrome in the periocular area: A review of the literature and case report. Ann Plast Surg. 2003;50(6):644–648. doi: 10.1097/01.SAP.0000069068.03742.48. [DOI] [PubMed] [Google Scholar]
- 7.Apaydin R, Bilen N, Bayramgurler D, Efendi H, Vahaboglu H. Detection of mycobacterium tuberculosis DNA in a patient with melkersson-rosenthal syndrome using polymerase chain reaction. Br J Dermatol. 2000;142(6):1251–1252. doi: 10.1046/j.1365-2133.2000.03569.x. [DOI] [PubMed] [Google Scholar]
- 8.Liu R, Yu S. Melkersson-rosenthal syndrome: A review of seven patients. J Clin Neurosci. 2013;20(7):993–995. doi: 10.1016/j.jocn.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Ziem PE, Pfrommer C, Goerdt S, Orfanos CE, Blume-Peytavi U. Melkersson-rosenthal syndrome in childhood: A challenge in differential diagnosis and treatment. Br J Dermatol. 2000;143(4):860–863. doi: 10.1046/j.1365-2133.2000.03791.x. [DOI] [PubMed] [Google Scholar]
- 10.Balevi B. Melkersson-rosenthal syndrome: Review of the literature and case report of a 10-year misdiagnosis. Quintessence Int. 1997;28(4):265–269. [PubMed] [Google Scholar]
- 11.Zimmer WM, Rogers RS, Reeve CM, Sheridan PJ. Orofacial manifestations of melkersson-rosenthal syndrome. A study of 42 patients and review of 220 cases from the literature. Oral Surg Oral Med Oral Pathol. 1992;74(5):610–619. doi: 10.1016/0030-4220(92)90354-S. [DOI] [PubMed] [Google Scholar]
- 12.Levenson MJ, Ingerman M, Grimes C, Anand KV. Melkersson-rosenthal syndrome. Arch Otolaryngol. 1984;110(8):540–542. doi: 10.1001/archotol.1984.00800340052015. [DOI] [PubMed] [Google Scholar]
- 13.Wadlington WB, Riley HD, Lowbeer L. The melkersson-rosenthal syndrome. Pediatrics. 1984;73(4):502–506. [PubMed] [Google Scholar]
- 14.Winnie R, DeLuke DM. Melkersson-rosenthal syndrome. Review of literature and case report. Int J Oral Maxillofac Surg. 1992;21(2):115–117. doi: 10.1016/S0901-5027(05)80546-6. [DOI] [PubMed] [Google Scholar]
- 15.Kesler A, Vainstein G, Gadoth N. Melkersson-rosenthal syndrome treated by methylprednisolone. Neurology. 1998;51(5):1440–1441. doi: 10.1212/WNL.51.5.1440:1526-632X. [DOI] [PubMed] [Google Scholar]
- 16.Orlando MR, Jr Atkins JS. Melkersson-Rosenthal syndrome. Arch Otolaryngol Head Neck Surg. 1990;116(6):728–729. doi: 10.1001/archotol.1990.01870060086017. [DOI] [PubMed] [Google Scholar]
- 17.Vistnes LM, Kernahan DA. The melkersson-rosenthal syndrome. Plast Reconstr Surg. 1971;48(2):126–132. [PubMed] [Google Scholar]
- 18.Alexander RW, James RB. Melkersson-rosenthal syndrome: Review of literature and report of case. J Oral Surg. 1972;30(8):599–604. [PubMed] [Google Scholar]
- 19.Sciubba JJ, Said-Al-Naief N. Orofacial granulomatosis: Presentation, pathology and management of 13 cases. J Oral Pathol Med. 2003;32(10):576–585. doi: 10.1034/j.1600-0714.2003.t01-1-00056.x. [DOI] [PubMed] [Google Scholar]
- 20.Gerressen M, Ghassemi A, Stockbrink G, Riediger D, Zadeh MD. Melkersson-rosenthal syndrome: Case report of a 30-year misdiagnosis. J Oral Maxillofac Surg. 2005;63(7):1035–1039. doi: 10.1016/j.joms.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Leao JC, Hodgson T, Scully C, Porter S. Review article: Orofacial granulomatosis. Aliment Pharmacol Ther. 2004;20(10):1019–1027. doi: 10.1111/j.1365-2036.2004.02205.x. [DOI] [PubMed] [Google Scholar]
- 22.van der Waal RI, Schulten EA, van de Scheur MR, Wauters IM, Starink TM, van der Waal I. Cheilitis granulomatosa. J Eur Acad Dermatol Venereol. 2001;15(6):519–523. doi: 10.1046/j.1468-3083.2001.00353.x. [DOI] [PubMed] [Google Scholar]
- 23.Dupuy A, Cosnes J, Revuz J, Delchier JC, Gendre JP, Cosnes A. Oral crohn disease: Clinical characteristics and long-term follow-up of 9 cases. Arch Dermatol. 1999;135(4):439–442. doi: 10.1001/archderm.135.4.439. [DOI] [PubMed] [Google Scholar]
- 24.Kemal O, Özgürsoy OB, Dursun G, Tulunay O. Melkersson-rosenthal sendromu klinik ve patolojik bulgular ve tedavi yaklaşımları. Turkiye Klinikleri J Med Sci. 2007;27(1):128–131. [Google Scholar]
- 25.Cerimele D, Serri F. Intralesional injection of triamcinolone in the treatment of cheilitis granulomatosa. Arch Dermatol. 1965;92(6):695–696. doi: 10.1001/archderm.1965.01600180087017. [DOI] [PubMed] [Google Scholar]
- 26.Krutchkoff D, James R. Cheilitis granulomatosa. Successful treatment with combined local triamcinolone injections and surgery. Arch Dermatol. 1978;114(8):1203–1206. doi: 10.1001/archderm.1978.01640200057015. [DOI] [PubMed] [Google Scholar]
- 27.Patel DK, Levin KH. Bell palsy: Clinical examination and management. Cleve Clin J Med. 2015;82(7):419–426. doi: 10.3949/ccjm.82a.14101. [DOI] [PubMed] [Google Scholar]


