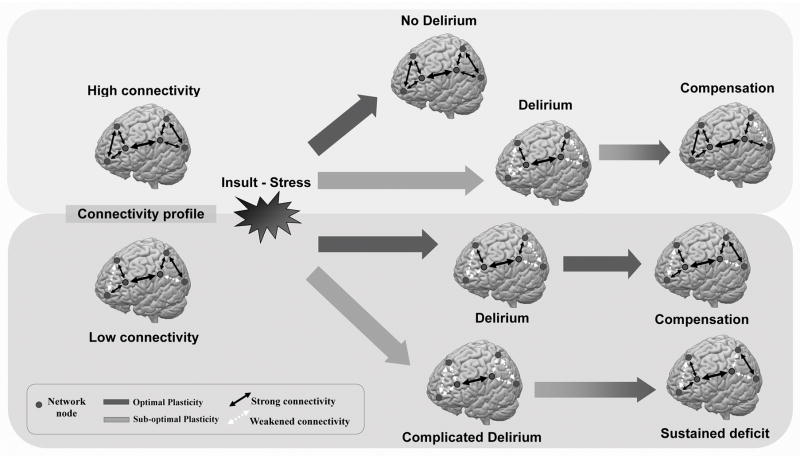
Figure 1. Conceptual Model of Brain Connectivity, Plasticity and Delirium.
The figure depicts a conceptual model illustrating how premorbid individual brain connectivity between brain regions (network nodes, grey circles) and the integrity of mechanism of brain plasticity (thick gray arrows) may relate to the susceptibility to delirium in response to exogenous (e.g. anesthesia) or endogenous (e.g. systemic infection) insults or stressors, and long-term outcome after recovery from delirium. Individuals with robust (high) baseline connectivity and preserved (optimal) cerebral plasticity (dark gray arrow, top) can accommodate stressors without changes in the integrity of brain networks, and thus do not experience delirium. Individuals with high baseline connectivity but impaired plasticity (light gray arrow, second row) cannot quickly accommodate to insults or stressors, and develop a significant decrease in connectivity and impairments in brain network integrity, which produce the symptoms of delirium. As the stressor resolves and normal brain connectivity is mostly reestablished, behavioral compensation occurs and normal cognitive function is restored. In individuals with low baseline connectivity but preserved plasticity (dark gray arrow, third row), insults/stressors acutely overwhelm normal plasticity processes, resulting in acute delirium. Over time, the baseline brain connectivity pattern is restored, and delirium resolves. In individuals with impairments in both baseline connectivity and plasticity (light gray arrow, bottom row), insults lead to severe disruptions in brain connectivity and function (complicated delirium). Brain network connectivity remains weakened even after resolution of the stressor, leading to sustained deficits.