Fig. 1.
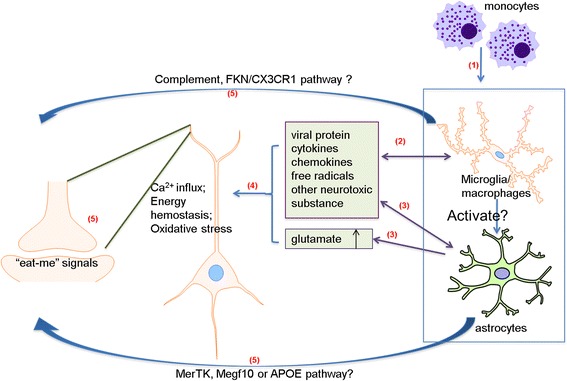
Potential mechanisms of HIV-induced synaptic degeneration. (1) HIV-1 infection of the CNS initiates from transmigration of HIV-1-infected peripheral blood monocytic cells/macrophages across the blood-brain barrier (BBB). Subsequently, microglia and astrocytes become infected and reactivated. (2) The immune-activated and HIV-1-infected microglia/macrophages release viral proteins (e.g. gp120, Tat, Vpr), cytokines (e.g. IL-1β, IL-6, TNF-α), chemokines (e.g. CXCL12, MCP1) and other neurotoxic factors. (3) Infected/reactivated astrocytes can also release neurotoxic substances and pathogenically enhance synaptic activity with increased transmitter release and impaired glutamate re-uptake. (4) The released neurotoxins and extracellular glutamate can cause excessive Ca2+ influx, disturbance of energy metabolism and production of reactive oxidative species, which then lead to the disruption of normal neuronal function. On the other hand, the released viral proteins, cytokines, chemokines and free radicals can activate more glial cells and macrophages. (5) These damaged neurons may mark the abnormal synapses with some kind of “eat-me” signals, which can be recognized and eliminated by microglia and/or astrocytes through phagocytotic pathways such as the complementary and FKN/CX3CR1 pathways in microglia or the MerTK, Megf10 and APOE pathway in astrocytes
