Abstract
Acute care hospitals have a role in managing the health care needs of people affected by cancer when they are at the end of life. However, there is a need to provide end-of-life care in other settings, including at home or in hospice, when such settings are more appropriate. Using data from 9 provinces, we examined indicators that describe the current landscape of acute care hospital use at the end of life for patients who died of cancer in hospital in Canada.
Interprovincial variation was observed in acute care hospital deaths, length of stay in hospital, readmission to hospital, and intensive care unit use at the end of life. High rates of acute care hospital use near the end of life might suggest that community and home-based end-of-life care might not be suiting patient needs.
Keywords: End of life, palliative care, acute care, home care
INTRODUCTION
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual”1. The definition continues, saying that palliative care is “applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life.” Early integration of palliative care can greatly reduce unplanned visits to the emergency department and multiple admissions to hospital, can shorten hospital stays, and can increase the number of home deaths for patients with advanced cancer2–4. As well, palliative care has been shown to significantly improve patient outcomes and quality of life in the domains of pain, anxiety, and symptom control5,6. Those results all suggest that palliative care can optimize patient outcomes and greatly affect the use of health services.
Admission to an acute care hospital could be appropriate for many cancer patients because of disease progression or because of a need for optimal management of treatment complications or for intensive care. Overuse of acute hospital care could signal that available outpatient, primary, or community care might not be addressing patient needs, but might also indicate a potential gap in palliative care services.
Measuring and reporting patterns of acute care hospital use at the end of life and making comparisons by province can help to advance jurisdictional initiatives meant to fill gaps in palliative care services. The Canadian Partnership Against Cancer is leading efforts to collect more pan-Canadian data about palliative care and end-of-life care, with the aim of developing a suite of measures that will lead to a better understanding of the experiences of Canadians with advanced and life-threatening cancer and will identify opportunities for system improvement.
METHODS
Records for cancer patients who died in acute care hospitals were extracted based on the Discharge Abstract Database provided by the Canadian Institute for Health Information, which collects data for separations with a discharge date between 1 April and 31 March of a given fiscal year. With respect to data storage and protection, readers can consult “Data Requests: Frequently Asked Questions” at the Canadian Institute for Health Information (https://www.cihi.ca/en/faq/data-request-frequently-asked-questions—see the Data Storage, Retention and Secure Destruction subsection). Cancer patients were identified using codes from the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada, for either a significant diagnosis of malignant neoplasm or neoplasms of uncertain or unknown behaviour; or a “most responsible” diagnosis of palliative care, with a secondary diagnosis of malignant neoplasm. The study aimed to capture records for all cancer patients (identified using significant or primary diagnosis codes for cancer or a combination of palliative care and cancer codes) who died in acute care hospitals. Patients who did not fit those criteria were excluded—for example, patients with only a secondary diagnosis of cancer or a history of cancer. In that respect, the study cohort might underestimate the true population of all cancer patients who died in acute care hospitals. However, a sensitivity analysis showed that any such effect was limited. Only facilities designated or considered to be acute care facilities were included in the analysis.
Intensive care unit (icu) data are reported only for acute care hospitals that have icu facilities. Data for emergency department (ed) visits were obtained from the National Ambulatory Care Reporting System. Ontario and Alberta are the only two provinces that have comprehensive and full-coverage ed data that are reported to the National Ambulatory Care Reporting System at the Canadian Institute for Health Information. Emergency department visits that resulted in an admission to acute care were included in the analysis.
Total cancer deaths were obtained from the national vital statistics database. The analysis was restricted to adults 18 years of age or older who died in an acute care hospital in fiscal years 2014–2015 and 2015–2016 for 9 provinces. Quebec was not included in the study because acute inpatient facilities in Quebec are not mandated by their provincial ministry of health to submit to the Discharge Abstract Database. Because of small patient counts, data from the Canadian territories are not included. Individual provincial numbers do not include the territories.
Provinces vary in how they categorize the location of death and the various care settings (for example, how hospital-based hospices or palliative care units are designated). Some provinces have palliative care units within certain acute care hospitals. Deaths in the palliative care units are therefore categorized as deaths in an acute care hospital, and so the ratio of hospital deaths in those provinces could appear higher in comparison with other provinces.
No ethics approval was sought for this study.
RESULTS
Results are presented here as ratios; percentages are provided to aid in interpretation.
Cancer Patients Dying in Acute Care Hospitals
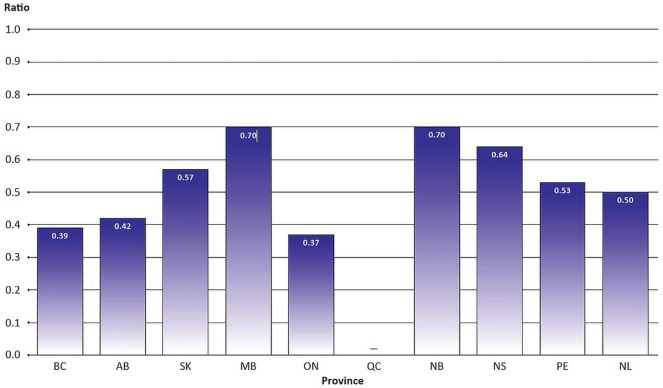
Data suggest that, in many reporting provinces, more than half of all cancer deaths occurred in an acute care hospital. The ratio of cancer patients dying in hospitals ranged from 0.70 (70%) in Manitoba and New Brunswick to 0.37 (37%) in Ontario (Figure 1, Table i).
FIGURE 1.
Ratio of cancer deaths in acute care hospitals to cancer mortality, by province, 2014–2015 and 2015–2016 fiscal years combined.
TABLE I.
Ratio of cancer deaths in an acute care hospital to cancer mortality, 2014–2015 and 2015–2016 fiscal years combined
| Province | Cancer deaths (n) | Ratio | |
|---|---|---|---|
|
| |||
| In acute care hospitala | Projectedb | ||
| British Columbia | 7,839 | 20,000 | 0.39 |
| Alberta | 5,458 | 12,900 | 0.42 |
| Saskatchewan | 2,695 | 4,700 | 0.57 |
| Manitoba | 3,832 | 5,500 | 0.70 |
| Ontario | 20,845 | 56,600 | 0.37 |
| Quebec | NA | NA | NA |
| New Brunswick | 2,695 | 3,870 | 0.70 |
| Nova Scotia | 3,421 | 5,350 | 0.64 |
| Prince Edward Island | 396 | 750 | 0.53 |
| Newfoundland and Labrador | 1,513 | 3,030 | 0.50 |
Cancer deaths in acute care hospitals numbered 48,987. Included are all adults 18 years of age or older discharged in fiscal years 2014–2015 and 2015–2016. Provinces differ in the configuration of palliative care units and the designation of “acute care.”
Includes all cancer deaths in patients age 0 or older in 2014 and 2015. Data source: Canadian Institute for Health Information, Discharge Abstract Database; Canadian Cancer Society, Canadian Cancer Statistics.
NA = not available.
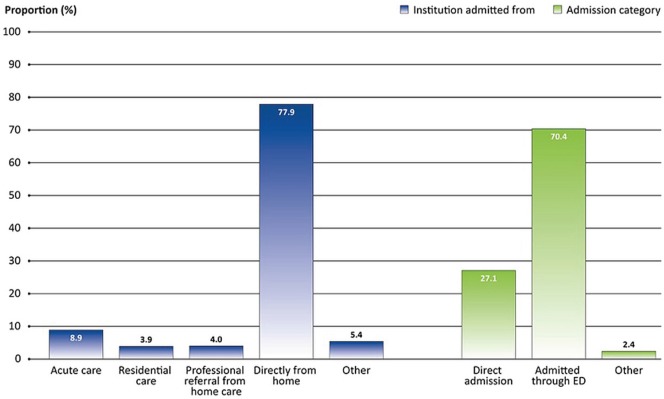
Most cancer patients who died in an acute care hospital were admitted to hospital directly from home (77.9%, Figure 2, Table ii). The remaining patients were transferred from another health care facility or were referred by home care or another level of care. Also, 70.4% of cancer patients were admitted through the ed at their final acute care admission (Figure 2, Table ii).
FIGURE 2.
Hospital admissions for patients with cancer who died in acute care hospitals, by admitting institution and admission category, 2014–2015 and 2015–2016 fiscal years combined.
TABLE II.
Hospital admissionsa for patients with cancer who died in an acute care hospital, 2014–2015 and 2015–2016 fiscal years combined
| Institution or admission category | Subcategory | Patientsb | |
|---|---|---|---|
|
| |||
| (n) | (%) | ||
| Admitted from | Acute care | 4,340 | 8.9 |
| Residential care | 1,933 | 3.9 | |
| Professional referral from home care | 1,939 | 4.0 | |
| Directly from homec | 38,143 | 77.9 | |
| Other | 2,632 | 5.4 | |
| Admission type | Direct admission | 13,280 | 27.1 |
| Admitted through emergency department | 34,508 | 70.4 | |
| Other | 1,199 | 2.4 | |
Data represent all provinces and territories except Quebec.
Includes all adults 18 years of age and older discharged in fiscal years 2014–2015 and 2015–2016.
Includes patients with missing values in the “admitted from institution type” field in the Discharge Abstract Database.
Data source: Canadian Institute for Health Information, Discharge Abstract Database.
Acute Care Hospital Use Near End of Life
Cumulative Length of Stay in Hospital in the Last 6 Months of Life
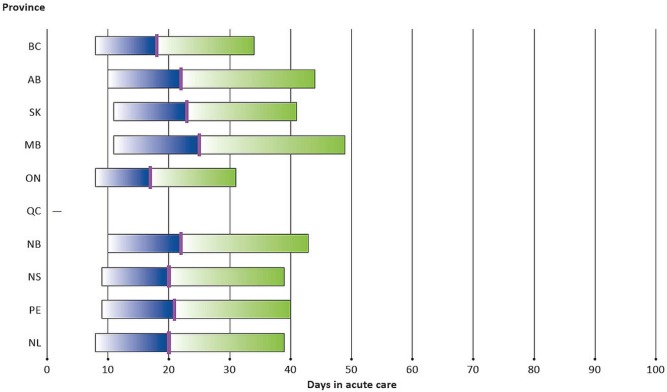
In the last 6 months of life, 50% of cancer patients dying in hospital had a cumulative length of stay ranging from 17 days in Ontario to 25 days in Manitoba. The median length of stay (50th percentile) was not observably different in the studied provinces (Figure 3, Table iii). Interprovincial variation was observed in the cumulative length of stay in hospital for 75% of the cancer patients, ranging from a low of 31 days in Ontario to a high of 49 days in Manitoba.
FIGURE 3.
Cumulative length of stay in acute care hospitals by patients with cancer in the 6 months before death, by province, 2014–2015 and 2015–2016 fiscal years combined. Each bar represents the range from the 25th to the 75th percentile, with a short line marking the median (50th percentile).
TABLE III.
Cumulative length of stay in an acute care hospital for patients with cancer in the 6 months before deatha, 2014–2015 and 2015–2016 fiscal years combined
| Province | Percentile (days) | ||
|---|---|---|---|
|
| |||
| 25th | 50th | 75th | |
| British Columbia | 8 | 18 | 34 |
| Alberta | 10 | 22 | 44 |
| Saskatchewan | 11 | 23 | 41 |
| Manitoba | 11 | 25 | 49 |
| Ontario | 8 | 17 | 31 |
| Quebec | NA | NA | NA |
| New Brunswick | 10 | 22 | 43 |
| Nova Scotia | 9 | 20 | 39 |
| Prince Edward Island | 9 | 21 | 40 |
| Newfoundland and Labrador | 8 | 20 | 39 |
Includes all adults 18 years of age and older discharged in fiscal years 2014–2015 and 2015–2016.
Data source: Canadian Institute for Health Information, Discharge Abstract Database.
NA = not available.
Multiple Admissions to Hospital in the Last Month of Life
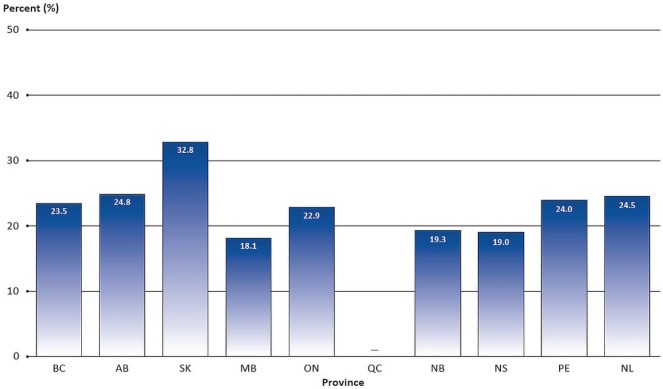
Of the studied patients, between 18.1% (in Manitoba) and 32.8% (in Saskatchewan) experienced 2 or more admissions to hospital in the last month of life (Figure 4, Table iv).
FIGURE 4.
Percentage of cancer patients who had 2 or more acute care inpatient admissions in the last 28 days of life and who died in hospital, by province, 2014–2015 and 2015–2016 fiscal years combined.
TABLE IV.
Cancer patients who had 2 or more acute care inpatient admissions in the last 28 days of life and who died in hospitala, 2014– 2015 and 2015–2016 fiscal years combined
| Province | Patients | |
|---|---|---|
|
| ||
| (n) | (%) | |
| British Columbia | 1,842 | 23.5 |
| Alberta | 1,351 | 24.8 |
| Saskatchewan | 884 | 32.8 |
| Manitoba | 694 | 18.1 |
| Ontario | 4,771 | 22.9 |
| Quebec | NA | NA |
| New Brunswick | 521 | 19.3 |
| Nova Scotia | 649 | 19.0 |
| Prince Edward Island | 95 | 24.0 |
| Newfoundland and Labrador | 370 | 24.5 |
Includes all adults 18 years of age and older discharged in fiscal years 2014–2015 and 2015–2016.
Data source: Canadian Institute for Health Information, Discharge Abstract Database.
NA = not available.
ED Use in the Last Month of Life
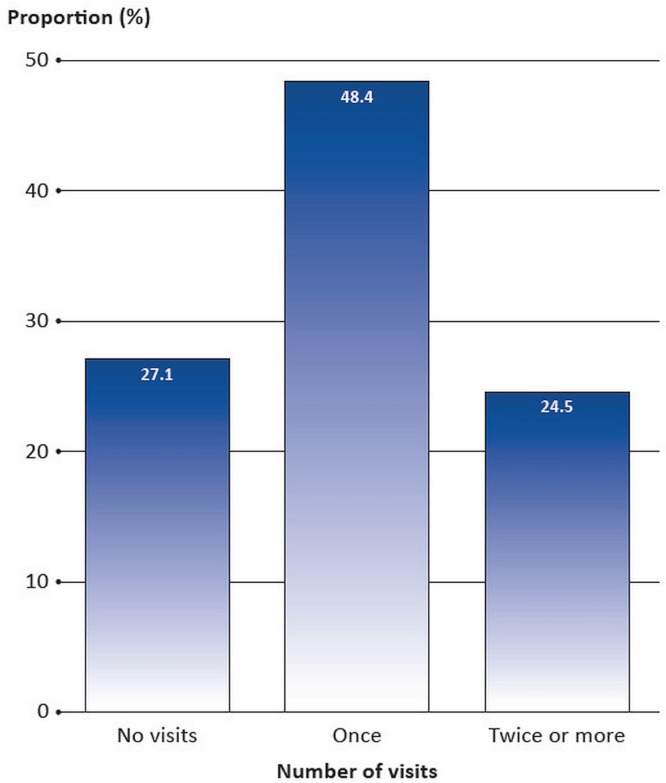
In Ontario and Alberta (the only provinces from which data are available), most cancer patients visited the ed only once (48.4%) in the last 28 days of life. A significant proportion visited the ed 2 or more times (24.5%, Figure 5, Table v).
FIGURE 5.
Distribution of emergency department visits in the last 28 days of life for cancer patients who died in hospital, Ontario and Alberta combined, 2014–2015 and 2015–2016 fiscal years combined.
TABLE V.
Emergency department visits in the last 28 days of life by cancer patients who died in hospital, Ontario and Alberta combineda, 2014–2015 and 2015–2016 fiscal years combined
| Visit frequency | Patients | |
|---|---|---|
|
| ||
| (n) | (%) | |
| Noneb | 7,125 | 27.1 |
| One | 12,722 | 48.4 |
| Two or more | 6,448 | 24.5 |
Includes only patients with a cancer diagnosis in Ontario and Alberta (where comprehensive emergency department data are available) who died in an acute care hospital.
Includes cancer patients already admitted to hospital in the 28 days before death.
Data source: Canadian Institute for Health Information, Discharge Abstract Database, 2014–2015 and 2015–2016; National Ambulatory Care Reporting System, 2013–2014 to 2015–2016.
ICU Use in the Last 14 Days of Life
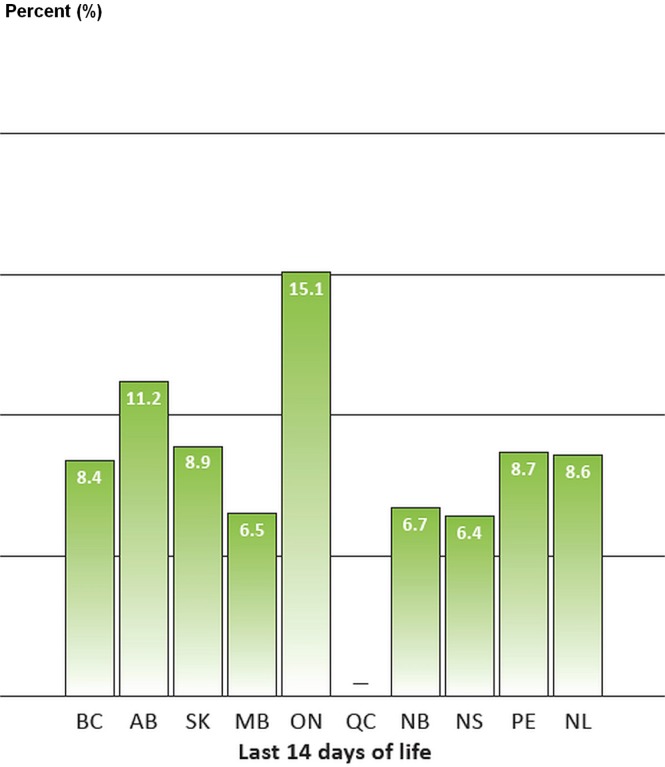
A relatively small proportion of patients dying of cancer in an acute care hospital received icu care in the last 14 days of life: between 6.4% in Nova Scotia and 15.1% in Ontario (Figure 6, Table vi).
FIGURE 6.
Percentage of cancer patients who were admitted to an intensive care unit in the last 14 days of life and who died in hospital, by province, 2014–2015 and 2015–2016 fiscal years combined.
TABLE VI.
Cancer patientsa who were admitted to an intensive care unitb in the last 14 days of life and who died in hospital, 2014–2015 and 2015–2016 fiscal years combined
| Province | Patients | |
|---|---|---|
|
| ||
| (n) | (%) | |
| British Columbia | 571 | 8.4 |
| Alberta | 363 | 11.2 |
| Saskatchewan | 177 | 8.9 |
| Manitoba | 165 | 6.5 |
| Ontario | 2,973 | 15.1 |
| Quebec | NA | NA |
| New Brunswick | 158 | 6.7 |
| Nova Scotia | 176 | 6.4 |
| Prince Edward Island | 24 | 8.7 |
| Newfoundland and Labrador | 106 | 8.6 |
Includes all adults 18 years of age and older discharged in fiscal years 2014–2015 and 2015–2016.
Includes only facilities that report intensive care unit data.
Data source: Canadian Institute for Health Information, Discharge Abstract Database.
NA = not available.
DISCUSSION AND CONCLUSIONS
The present study provides information about the current landscape of acute care hospital use by cancer patients near the end of life across Canada, examining variation in use by province. Those data will add to the existing body of research about end-of-life care for patients with cancer and offer new findings about interprovincial variation in the management of end-of-life care.
An international comparative study of hospital use during the last 30 days of life found that, of 7 countries, Canada fell into the middle range for hospital use, including number of hospital days at the end of life for patients dying from cancer7. Patients spent 7.7 days in hospital at the end of life in Canada. The number of hospital days was higher in Belgium (10.6 days) and lower in Germany and England (7.4 days). It is possible that the cost of a hospital stay influences the need to find alternatives to hospitalization such as home or hospice. As reported in that study, the per diem cost for a hospital stay is relatively high in the United States, which could be one factor influencing hospital use7.
A systematic review of the evidence for effective palliative care revealed that jurisdictions with earlier palliative care intervention had higher hospice enrolment, fewer hospital admissions, and fewer days spent in hospital near the end of life8. Further study is required to examine other factors influencing hospital use, including social determinants of health (for example, the patient’s supportive care networks and ethnicity) and hospital-specific factors.
The Canadian data examined in the present study suggest wide variation in cancer patient deaths occurring in acute care hospitals. Several Canadian surveys have shown that many cancer patients would prefer to spend their final days and to die at home or in a hospice rather than in a hospital9. However, a lack of awareness about, or availability of, appropriate palliative care resources or services at home (for example, to ensure effective symptom management) could make death at home or in a hospice less achievable10. Enablers of dying at home could include provincial coverage of medication and equipment in the home setting, home care, caregiver benefits, respite care, having people at home to help care for the patient, and access to 24/7 medical care. In reality, symptom management resources, emotional support from caregivers or loved ones, and family caregiving to support dying at home are not always available or realistically achievable at home. It is important to be aware that patient and caregiver preferences or needs can change over time as a result of clinical, psychological, or practical challenges. For some people, the preferred end-of-life setting might eventually be the hospital or a hospital-like setting. Although small studies have been published, no national data are (as of 2016) routinely collected to identify a person’s care needs or preferred location of death.
Data from two provinces that have comprehensive data are available provide insight into ed use at the end of life. Those data suggest that most cancer patients are admitted to the hospital through the ed in their final acute care admission. Examining that finding, together with other data, could help to evaluate the adequacy of and access to primary care and community-based services, including home care, that can help reduce avoidable ed visits. Studies have signalled that a relatively high proportion of ed visits are potentially unnecessary, indicating an opportunity to reduce avoidable ed visits11,12. In the present study, the reason for an ed visit was not available. However, an Ontario study showed that symptoms such as pain, dyspnea, malaise, and fatigue were the main reasons for visits to the ed at the end of life3. Symptom assessment tools might help to identify patient distress earlier and to reduce unnecessary visits to the ed.
The data also show that between 18.1% and 32.8% of patients are being admitted to hospital 2 or more times in the last month of life. Multiple admissions to hospital might signal limited access to community resources, including caregiver supports and palliative care services that can be provided in a home environment. Clarity about a patient’s goals for care and good communication between physicians and the patient and family can be important to reduce avoidable admissions and to promote the integration of palliative care earlier in the patient journey.
Although the use of the icu for cancer patients at the end of life is relatively low in Canada, provincial variations are evident. Given that variation, it is likely that a portion of icu stays could be avoided and that some patients could benefit more from supportive therapy.
Differences in acute care hospital use at the end of life were examined by patient age, urban compared with rural residence, and type of cancer. The preliminary analysis suggests that hospital use was, in general, higher for younger patients, rural residents, and patients with hematologic cancers (leukemia and non-Hodgkin lymphoma) (Data not shown). Those specific subgroups might have unique needs and considerations that have to be better addressed to ensure that they receive equitable access to palliative and end-of-life care services. For example, lack of access for rural residents to community-based services after clinical hours likely increases reliance on hospital care. That finding is supported by numerous studies13–15.
Further work is needed to better understand the landscape of end-of-life care in Canada:
■ Patterns of end-of-life care for cancer patients across all health settings
■ Concordance between patient preference and goals for care and the care received
■ Interprovincial variations in access to community-based palliative care services
Continued measurement of those indicators could potentially identify opportunities for increasing the use of more suitable settings for end-of-life care delivery, and thus improve quality of life for patients and their families.
More information about the Canadian Partnership Against Cancer’s System Performance Initiative and its reports and indicators can be found at http://www.systemperformance.ca/.
Limitations
In this study examining indicators related to end-of-life care (a component of palliative care) in the Canadian context in a single sector (acute care institutions), the indicators do not currently evaluate palliative care and the quality of care throughout the entire disease course. Also, indicators were restricted to patients who had a cancer diagnosis and who died in an acute care hospital. Data concerning hospital use by cancer patients who died outside of hospital were not available. Our hope is that reporting on the currently available data will provide incentives to enhance data quality and to address the data knowledge gap system-wide in end-of-life care delivery in Canada.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.World Health Organization(who) WHO Definition of Palliative Care [Web page] Geneva, Switzerland: WHO; 2016. [Available at: http://www.who.int/cancer/palliative/definition/en; cited 1 August 2017] [Google Scholar]
- 2.Bainbridge D, Seow H, Sussman J, Pond G, Barbera L. Factors associated with not receiving homecare, end-of-life homecare, or early homecare referral among cancer decedents: a population-based cohort study. Health Policy. 2015;119:831–9. doi: 10.1016/j.healthpol.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182:563–8. doi: 10.1503/cmaj.091187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ananth P, Melvin P, Berry JG, Wolfe J. Trends in hospital utilization and costs among pediatric palliative care recipients. J Palliat Med. 2017 doi: 10.1089/jpm.2016.0496. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–42. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 6.Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383:1721–30. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 7.Bekelman JE, Halpern SD, Blankart C, et al. on behalf of the International Consortium for End-of-Life Research Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315:272–83. doi: 10.1001/jama.2015.18603. [DOI] [PubMed] [Google Scholar]
- 8.Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I. Effectiveness of specialized palliative care: a systematic review. JAMA. 2008;299:1698–709. doi: 10.1001/jama.299.14.1698. [DOI] [PubMed] [Google Scholar]
- 9.Murray MA, Fiset V, Young S, Kryworuchko J. Where the dying live: a systematic review of determinants of place of end-of-life cancer care. Oncol Nurs Forum. 2009;36:69–77. doi: 10.1188/09.ONF.69-77. [DOI] [PubMed] [Google Scholar]
- 10.Canadian Hospice Palliative Care Association (chpca) The Pan-Canadian Gold Standard for Palliative Home Care: Toward Equitable Access to High Quality Hospice Palliative and End-of-Life Care at Home. Ottawa, ON: CHPCA; 2006. [Available online at: http://www.chpca.net/media/7652/Gold_Standards_Palliative_Home_Care.pdf; cited 1 August 2017] [Google Scholar]
- 11.Delgado-Guay MO, Kim YJ, Shin SH, et al. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49:497–504. doi: 10.1016/j.jpainsymman.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Lawson BJ, Burge FI, McIntyre P, Field S, Maxwell D. Can the introduction of an integrated service model to an existing comprehensive palliative care service impact emergency department visits among enrolled patients? J Palliat Med. 2009;12:245–52. doi: 10.1089/jpm.2008.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hui D, Didwaniya N, Vidal M, et al. Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer. 2014;120:1572–8. doi: 10.1002/cncr.28614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–6. doi: 10.1200/JCO.2007.15.8253. [Errata in: J Clin Oncol 2011;29:4472; J Clin Oncol 2010;28:3205] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henson L, Gao W, Higginson I, et al. Emergency department attendance by patients with cancer in the last month of life: a systematic review and meta-analysis. Lancet. 2015;385(suppl 1):S41. doi: 10.1016/S0140-6736(15)60356-7. [DOI] [PubMed] [Google Scholar]