Abstract
IMPORTANCE
As the American population ages, effective healthcare planning requires understanding changes in hearing loss prevalence.
OBJECTIVE
Determine if age- and sex-specific prevalence of adult hearing loss changed during the past decade.
DESIGN
Analysis of 2011–2012 National Health and Nutrition Examination Survey (NHANES) audiometric data compared to NHANES 1999–2004. NHANES is a cross-sectional, nationally-representative interview and examination survey of the civilian, non-institutionalized population.
PARTICIPANTS
A stratified random sample of 3,831 adults aged 20–69 years
INTERVENTIONS
Audiometry and questionnaires
MAIN OUTCOMES AND MEASURES
Speech-frequency hearing impairment (HI) defined by pure-tone average (PTA) of thresholds across 0.5–1–2–4 kHz greater than 25 dB hearing level (HL); high-frequency HI defined by PTA across 3–4–6 kHz >25 dB HL. Logistic regression was used to examine unadjusted, age- and sex-adjusted, and multivariable-adjusted associations with demographic, noise exposure, and cardiovascular risk factors.
RESULTS
The 2011–2012 unadjusted adult prevalence of unilateral and bilateral speech-frequency HI was 14.1%, compared to 16% for 1999–2004; after age- and sex-adjustment, the difference was significant, odds ratio (OR)=0.70 (95% confidence interval [95% CI]: 0.56–0.86). Men had nearly twice the prevalence of speech-frequency HI, 18.6% (17.8 million), compared to women, 9.6% (9.7 million). For 60–69 year-olds, speech-frequency HI prevalence was 39.3% (95% CI: 30.7%–48.7%). In multivariable analyses for bilateral speech-frequency HI, age was the major risk factor; however, men, non-Hispanic (NH) white and NH Asian race, lower educational attainment, and heavy use of firearms all had significant associations. Additional associations for high-frequency HI were Mexican-American and Other Hispanic race/ethnicity and the combination of loud and very loud noise exposure occupationally and outside of work, OR=2.4 (95% CI: 1.4–4.2).
CONCLUSIONS AND RELEVANCE
Adult hearing loss is common and strongly associated with age and other demographic factors (sex, race/ethnicity, education). Noise exposure, which is preventable, was less strongly associated. Cardiovascular risk factors – heavy smoking, hypertension, and diabetes – were significant only in unadjusted analyses. Age- and sex-specific HI prevalence continues to decline. Despite the benefit of delayed onset of HI, hearing healthcare needs will increase as the U.S. population grows and ages.
Keywords: prevalence, hearing impairment, speech frequency pure-tone average, high frequency pure-tone average, age-related hearing loss, noise-induced hearing loss, NHANES
Introduction
Since 1959, the U.S. has conducted exam-based health surveys measuring hearing thresholds in nationally-representative samples across the age range. Hearing testing in adults has been accomplished in four surveys. The National Health Examination Survey (NHES I) conducted air-conduction hearing threshold tests, each ear, at six frequencies (0.5–1–2–3–4–6 kHz) in adults aged 18–74 years, 1959–1962. The first National Health and Nutrition Examination Survey (NHANES I) tested hearing, each ear, at four frequencies (0.5–1–2–4 kHz) in adults aged 25–74 years, 1971–1975. Since 1999, NHANES has operated continuously in two-year cycles; in 1999–2004 and 2011–2012, NHANES conducted hearing tests in each ear at seven frequencies (0.5–1–2–3–4–6–8 kHz) in adults aged 20–69 years. We previously reported that high-frequency (3 to 6 kHz) hearing thresholds for people of specified age and sex groups were better in 1999–2004 than in 1959–1962; most of these differences were statistically significant.1
In this paper, we report the prevalence of hearing impairment (HI) in more recent 2011–2012 NHANES data compared to 1999–2004, to determine whether hearing in American adults has continued to improve. In addition, we report the relationships between well known risk factors (demographic, noise exposure, and cardiovascular) and HI prevalence in NHANES 2011–2012.
Materials and Methods
The National Health and Nutrition Examination Survey is conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC) to monitor the health and nutritional status of the civilian, non-institutionalized U.S. population. The survey includes an in-person interview covering socio-demographic characteristics, health status, risk factors, and other health-related information including a physical examination. Race/ethnicity was self-reported using Federal guidelines. The survey uses a complex, multi-stage, stratified, cluster design with over-sampling of targeted subgroups to produce nationally-representative estimates. During 1999–2004, NHANES over-sampled non-Hispanic (NH) black and Mexican-American, low-income, adolescents 12–19 years, and adults 60+ years, in an effort to obtain reliable data for these subgroups.2 In 2011–2012, NHANES over-sampled Hispanic, NH Asian, NH black, as well as NH white (and “other” race/ethnicities) at or below 130% of the poverty index and/or aged 80 years or over.3
NHANES 1999–2004 conducted audiometric exams on a half-sample of interviewed adults aged 20–69; audiometric exams in NHANES 2011–2012 were conducted on a full sample of interviewed adults in the same age range. Participation rates for audiometry in NHANES 1999–2004 were 67.5% of the eligible sample (i.e., those selected for the survey) and 87.8% of participants who actually agreed to participate and completed the household interview. Response rates for NHANES 2011–2012 were 57.4% and 81.9% respectively; the lower response rates coincided with the NHANES decision to begin oversampling non-Mexican-American/Other Hispanic and NH Asian subgroups. Both surveys were approved by the NCHS Institutional Review Board and all participants provided written consent. In both time periods, the audiometry examination was conducted by trained NHANES health technicians and included otoscopy, tympanometry, and air-conduction, pure-tone audiometry.
Audiometric testing was conducted in sound booths (Acoustic Systems, model Delta 142) in a Mobile Examination Center (MEC), which were transported to each survey location. Ambient noise met the ANSI S3.1 standards for maximum permissible ambient noise levels.4,5 During testing, background noise was monitored continuously. Thresholds were obtained using an Interacoustics AD226™ microprocessor audiometer, which met the specifications of ANSI S3.6-1996.6 The audiometric testing protocols are available on the NCHS website.7,8
Thresholds were obtained using a pulsed-tone stimulus and modified Hughson-Westlake procedure.9 Thresholds were obtained, each ear, at 0.5–1–2–3–4–6–8 kHz. Retest thresholds were obtained at 1 kHz, each ear to confirm consistency; the second 1 kHz threshold was used in this analysis. The first test ear was alternated and tones were initially presented at 40 dB hearing level (HL), then followed by the “up 5-dB/down 10-dB" threshold search method. Threshold was defined as the level at which the subject responded at least 50% of the time to ascending or descending presentations. Thresholds were usually obtained using supra-aural (TDH) headphones; insert transducers (EARtone 3A) were used when participants had collapsing ear canals. Masking was not used; however, thresholds were retested in the poorer ear with insert earphones when marked interaural asymmetry was found. When available, insert thresholds were used in the analysis.
The audiometric test protocol was identical during both survey periods. However, the supra-aural headphones changed from model TDH-39P to TDH-49P to avoid potential calibration errors at 6 kHz when using an NBS-9A style coupler.10 This change might have improved thresholds at 6 kHz; however, we could not find statistically significant evidence of this occurring. A recent study examined threshold measurements using TDH-39P headphones and found negligible evidence of spurious 6 kHz notches.11
The NHANES household questionnaire was administered by trained interviewers in the participant’s home via computer-assisted personal interview (CAPI). The 1999–2004 and the 2011–2012 survey questionnaires included similar questions on hearing health and risk factors, including self-assessed hearing ability, hearing aid use, tinnitus, and both occupational and non-occupational noise exposure. Other NHANES questionnaires collected information on important co-variates, including cardiovascular disease risk factors.
Relevant questionnaire differences between NHANES 1999–2004 and 2011–2012 were:
Work-related noise exposure in the 1999–2004 NHANES was defined as exposure for “at least 3 months” in the “current job” and/or the “job held the longest”; duration of exposure was inferred from length of time each job was held. Noise exposure in other jobs was assessed by asking about noise exposure lasting at least 3 months “in any job” with no further measure of duration. In 2011–2012, respondents were asked if they “ever had a job, or combination of jobs” which included noise exposure “for 4 or more hours a day, several days a week?” and, if so, “for how many months or years?” the exposure occurred.
In 1999–2004, participants were asked about non-occupational noise such as “power tools or loud music” that occurred “on average at least once per month for a year.” In 2011–2012, participants were asked about non-occupational “noise or music” exposures such as from “power tools, lawn mowers, farm machinery, cars, trucks, motorcycles, motorboats, or loud music” that lasted “10 or more hours a week.”
The 1999–2004 questionnaire asked about exposure to “loud” occupational or non-occupational noise, defined as noise “so loud that you had to speak in a raised voice to be heard.” In 2011–2012, participants were asked additionally about “very loud” noise, defined as “noise so loud you have to shout in order to be understood by someone standing 3 feet away.”
In 1999–2004, only non-occupational firearms noise was assessed, “Outside of work, have you ever been exposed to firearms noise for an average of at least once a month for a year?” Both occupational and non-occupational firearms noise were assessed in 2011–2012, and participants were asked to “estimate the total lifetime number of rounds fired.”
In both survey periods, participants were classified positive for diabetes if they answered “yes” to “ever been told by a doctor or other health professional that you have diabetes” or “now taking diabetic pills to lower blood sugar” or had a two hour fasting glucose ≥200 mg/dl. Participants were classified positive for hypertension if they answered “yes” to “Have you ever been told you have high blood pressure?” or “Are you taking a prescription for hypertension?” or, if during the MEC exam, the average of four blood pressure measurements was >140 mmHg (systolic) or >90 mmHg (diastolic). Smoking history was defined as “nonsmoker” if the respondent answered “no” to “Have you smoked at least 100 cigarettes in your life?” Current and former smokers were divided into two groups, <20 pack-years and ≥20 pack-years, i.e., smoked one pack (20 cigarettes) daily for less than or ≥20 years. Additional information is available on the NCHS website.3
Statistical Analysis
The statistical programs SAS™ version 9.2 (SAS Institute, Inc., Cary, NC) and SUDAAN™ (Research Triangle Institute [RTI] International, Research Triangle Park, NC) were used in the analysis to incorporate the NHANES examination sample weights, which accounted for differential probabilities of selection and adjustments for over-sampling of selected populations, non-response, and non-coverage (for groups in the population that do not appear in the sample).
Based on 3,831 adults with complete threshold measurements, the speech frequency pure-tone average (PTA) was calculated across 0.5–1–2–4 kHz test frequencies and the high frequency PTA was calculated across 3–4–6 kHz in each ear. The ear with the lower PTA was the better ear for that set of frequencies. Hearing impairment (HI) was defined by PTAs greater than 25 dB HL. This criterion for “mild or worse” hearing impairment has been used in other surveys;12 it is strongly related to self-reported hearing difficulty.13 Bilateral HI is defined as better ear PTA greater than 25 dB HL and unilateral HI is defined as worse ear PTA greater than 25 dB HL and better ear PTA less than or equal to 25 dB HL. Overall HI includes both unilateral and bilateral HI and is equivalent to worse ear HI.
We calculated HI prevalences across several demographic, noise exposure, and cardiovascular risk factors. We also compared HI prevalences for individual frequencies and PTAs between 1999–2004 and 2011–2012. The hearing threshold data from the two time periods were combined, maintaining appropriate survey weights, and then HI odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using SUDAAN™ logistic regression adjusting for age and sex.
The SUDAAN™ logistic regression procedure was also used to calculate odds ORs and 95% CIs for bilateral (better ear) speech-frequency HI and high-frequency HI in three different analyses: a) unadjusted (each variable separately in the predictive model), b) age- and sex-adjusted (each variable plus age and sex in the predictive model), and c) multivariable adjusted (all variables included in the predictive model).
Results
In 2011–2012, unilateral speech-frequency HI prevalence was 6.6% (13.0 million) and bilateral speech-frequency HI prevalence was 7.5% (14.7 million). As shown in Table 1, overall (unilateral plus bilateral) or “worse ear”, speech-frequency HI prevalence in 2011–2012 among adults aged 20 to 69 years was 14.1% (27.7 million), which is reduced from the 16% prevalence published for NHANES 1999–2004.14 In Table 2, after age- and sex-adjustment, the speech-frequency HI worse ear comparison (2011–2012 vs 1999–2004) shows a significant reduction, OR=0.70 (95% CI: 0.56–0.86).
Table 1.
Prevalence of Speech-Frequency and High-Frequency Hearing Impairment (HI) Among U.S. Adults, 20–69 Years, by Demographic Characteristics, Noise Exposures, and Cardiovascular Risks, NHANES, 2011–2012
|
Speech Frequency HIa % (95% Confidence Intervals) |
High Frequency HIb % (95% Confidence Intervals) |
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Sample Number |
(Population- weighted %)c |
Overalld | Unilaterale | Bilateralf | Overalld | Unilaterale | Bilateralf | |
| Total (2011–2012) | 3,831 | (100.0) | 14.1 (11.6–17.1) | 6.6 (5.4–8.1) | 7.5 (5.8–9.6) | 31 (28–34) | 12 (11–14) | 19 (17–22) |
| Sex | ||||||||
| Male | 1,953 | (50.0) | 18.6 (14.8–23.1) | 8.7 (6.6–11.4) | 9.9 (7.2–13.3) | 42 (37–48) | 15 (12–17) | 28 (23–33) |
| Female | 1,878 | (50.0) | 9.6 (7.2–12.7) | 4.5 (3.3–6.1) | 5.1 (3.6–7.3) | 20 (17–23) | 9 (8–11) | 11 (9–13) |
| Age, years | ||||||||
| 20–29 | 840 | (21.6) | 2.2 (1.3–3.7) | 1.4 (0.7–2.6) | 0.8 (0.3–2.3) | 7 (5–10) | 5 (3–8) | 2 (1–4) |
| 30–39 | 758 | (19.0) | 3.3 (2.1–5.2) | 2.4 (1.3–4.2) | 0.9 (0.4–2.1) | 11 (9–13) | 8 (6–10) | 3 (2–5) |
| 40–49 | 739 | (21.5) | 7.8 (5.5–11.0) | 4.4 (3.2–5.9) | 3.4 (2.1–5.6) | 26 (21–32) | 11 (9–15) | 15 (11–19) |
| 50–59 | 772 | (22.1) | 23.1 (18.7–28.1) | 11.8 (8.7–15.9) | 11.2 (7.5–16.6) | 50 (44–56) | 19 (16–24) | 31 (25–37) |
| 60–69 | 722 | (15.9) | 39.3 (30.7–48.7) | 14.6 (9.6–21.6) | 24.7 (20.2–29.9) | 68 (59–76) | 17 (13–21) | 51 (44–58) |
| Race/ethnicity | ||||||||
| NHg white | 1,334 | (66.5) | 15.9 (12.8–19.6) | 6.9 (5.2–9.1) | 9.0 (7.1–11.5) | 34 (31–37) | 12 (11–14) | 21 (19–24) |
| NHg black | 1,063 | (11.6) | 9.0 (7.5–10.9) | 5.0 (4.1–5.9) | 4.1 (2.7–6.2) | 22 (19–26) | 11 (9–13) | 12 (9–15) |
| Mexican-American | 397 | (7.9) | 9.2 (6.5–13.0) | 4.9 (2.7–8.7) | 4.3 (3.3–5.7) | 28 (24–32) | 13 (11–15) | 15 (13–18) |
| NHg Asian | 538 | (4.9) | 10.8 (7.2–15.8) | 6.1 (3.9–9.2) | 4.7 (2.8–7.8) | 25 (19–31) | 11 (9–14) | 14 (10–18) |
| Other Hispanic | 378 | (6.3) | 9.1 (6.3–13.0) | 5.2 (2.8–9.5) | 3.9 (1.9–7.7) | 26 (21–31) | 9 (7–12) | 17 (12–23) |
| Other race | 121 | (2.8) | 22.6 (10.3–42.6) | 15.2 (6.9–30.1) | 7.4 (2.3–21.2) | 34 (18–54) | 13 (5–26) | 22 (13–34) |
| Education | ||||||||
| <High school | 737 | (13.8) | 19.2 (15.6–23.3) | 7.9 (6.1–10.1) | 11.3 (8.5–14.8) | 42 (39–46) | 14 (11–18) | 28 (24–33) |
| High school | 805 | (19.7) | 19.1 (13.9–25.8) | 9.7 (6.8–13.6) | 9.5 (6.5–13.5) | 40 (34–46) | 15 (11–19) | 25 (22–29) |
| Some college/AA | 1,246 | (33.7) | 14.8 (11.3–19.3) | 6.6 (4.8–8.9) | 8.3 (5.5–12.4) | 27 (21–34) | 11 (8–14) | 16 (12–22) |
| ≥College graduate | 1,043 | (32.9) | 8.3 (6.0–11.3) | 4.3 (2.4–7.6) | 4.0 (2.6–6.0) | 27 (21–30) | 11 (8–14) | 15 (11–18) |
| Smoking, pack-years | ||||||||
| Nonsmoker | 2,206 | (55.8) | 11.1 (8.9–13.7) | 5.3 (4.3–6.4) | 5.8 (4.2–7.9) | 26 (22–30) | 11 (9–13) | 15 (12–18) |
| <20 | 623 | (17.2) | 7.6 (5.1–11.0) | 4.8 (3.1–7.5) | 2.7 (1.6–4.6) | 23 (18–28) | 10 (7–15) | 13 (9–19) |
| ≥20 | 874 | (23.5) | 26.4 (22.0–31.3) | 11.8 (9.2–15.0) | 14.6 (12.0–17.7) | 50 (45–55) | 15 (12–18) | 35 (31–39) |
| Unknown | 128 | (3.4) | 12.5 (5.6–25.7) | 1.8 (0.7–4.4) | 10.7 (4.2–24.9) | 24 (17–34) | 12 (7–23) | 13 (7–21) |
| Hypertension | ||||||||
| No | 2,481 | (68.3) | 10.9 (8.5–13.7) | 5.3 (4.1–6.7) | 5.6 (4.1–7.6) | 24 (21–28) | 10 (9–12) | 14 (12–17) |
| Yes | 1,350 | (31.7) | 21.1 (17.7–25.0) | 9.6 (7.4–12.3) | 11.6 (9.1–14.6) | 46 (42–50) | 16 (13–20) | 30 (26–33) |
| Diabetes mellitush | ||||||||
| No | 3,331 | (90.5) | 12.5 (10.1–15.3) | 5.7 (4.6–7.1) | 6.8 (5.1–8.9) | 28 (25–31) | 11 (10–13) | 17 (15–19) |
| Yes | 499 | (9.5) | 29.8 (22.6–38.2) | 15.2 (9.0–24.5) | 14.6 (12.0–17.6) | 60 (53–67) | 21 (16–26) | 39 (30–50) |
| Occupationali | ||||||||
| No | 2,477 | (63.7) | 11.3 (9.0–14.1) | 5.8 (4.5–7.5) | 5.5 (4.1–7.3) | 25 (23–28) | 11 (9–13) | 14 (13–16) |
| Yes, “loud” only (<5 years) | 234 | (6.3) | 8.9 (4.9–15.6) | 3.5 (1.3–9.1) | 5.0 (3.0–9.6) | 29 (20–39) | 12 (8–19) | 16 (11–23) |
| Yes, “loud” only (≥5 years) | 233 | (6.3) | 19.2 (12.2–29.0) | 9.2 (4.6–17.7) | 10.0 (6.7–14.7) | 45 (38–52) | 16 (9–27) | 28 (21–37) |
| Yes, “very loud” (<5 years) | 406 | (11.5) | 14.4 (8.1–24.4) | 5.5 (3.1–9.8) | 8.9 (4.5–16.7) | 34 (27–41) | 13 (7–21) | 21 (15–28) |
| Yes, “very loud” (≥5 years) | 427 | (11.2) | 30.7 (25.1–36.8) | 12.8 (8.8–18.4) | 17.8 (11.9–25.7) | 57 (46–67) | 14 (10–19) | 43 (35–51) |
| Unknown | 54 | (1.0) | 6.9 (2.7–16.6) | 4.6 (1.5–13.4) | 2.3 (0.5–10.8) | 27 (14–47) | 17 (7–37) | 10 (5–21) |
| Outside of work,j “very loud” | ||||||||
| No | 3,359 | (87.3) | 13.6 (10.7–17.1) | 6.2 (4.7–8.2) | 7.3 (5.8–9.3) | 30 (27–33) | 12 (10–14) | 18 (16–21) |
| Yes | 470 | (12.7) | 18.1 (11.3–27.8) | 9.4 (5.7–15.3) | 8.6 (4.2–17.0) | 37 (28–46) | 12 (9–18) | 25 (18–33) |
| Firearms, includes use for recreation, job, or military | ||||||||
| No | 2,433 | (54.3) | 11.4 (9.1–14.2) | 6.0 (4.5–8.0) | 5.4 (4.3–6.8) | 26 (24–29) | 12 (10–13) | 14 (13–16) |
| Yes | 1,395 | (45.7) | 17.3 (13.6–21.9) | 7.3 (5.7–9.5) | 10.0 (7.3–13.6) | 37 (32–43) | 12 (9–16) | 25 (21–29) |
| Rounds fired (firearms) | ||||||||
| None | 2,433 | (54.3) | 11.4 (9.1–14.2) | 6.0 (4.5–8.0) | 5.4 (4.3–6.8) | 26 (24–29) | 12 (10–13) | 14 (13–16) |
| 1 to <1,000 | 977 | (32.6) | 14.0 (10.6–18.2) | 6.0 (4.2–8.4) | 8.0 (5.8–10.9) | 32 (27–38) | 10 (6–16) | 22 (18–27) |
| 1,000 or more | 401 | (12.9) | 26.0 (19.7–33.4) | 10.8 (8.4–13.7) | 15.2 (9.4–23.6) | 50 (40–59) | 18 (13–24) | 32 (22–43) |
Speech-frequency hearing impairment (HI) is defined as pure-tone average (PTA) of thresholds across 0.5–1–2–4 kHz greater than 25 dB hearing level (HL).
High-frequency HI is defined as PTA of thresholds across 3–4–6 kHz greater than 25 dB HL.
The total number of U.S. civilian, non-institutionalized adults aged 20–69 years in the 2011–2012 NHANES was 196.6 million.
“Overall” sums unilateral and bilateral HI; this means hearing HI in either or both ears, i.e., a “worse ear” definition of HI.
“Unilateral” HI means the PTA in only one ear exceeds 25 dB HL.
“Bilateral” HI means the PTAs in both ears exceed 25 dB HL, i.e., a “better ear” definition of HI.
NH is an abbreviation for non-Hispanic.
Diabetes was defined by a positive response to: (a) ‘Yes’ to “Ever been told by a doctor or other health professional that you have diabetes?”, (b) ‘Yes’ to “Now taking diabetic pills to lower blood sugar”, or (c) a two hour fasting glucose ≥200 mg/dl.
Occupational noise exposure is defined as: “exposed at work to loud sounds or noise for 4 or more hours, several days a week”; “how long” this exposure is categorized as “< 5 years” or “≥ 5 years”. In addition, separate categories distinguish adults who “only” had loud noise exposure at work (“so loud that they had to raise their voice to be heard”) versus those who also had very loud noise exposure at work (“so loud that they had to shout to be heard”); see complete wording of the question in the Methods section.
Noise exposure outside of work is defined as: “Outside of a job, ever exposed to very loud noise or music for 10 or more hours a week?” Examples are noise from power tools, lawn mowers, farm machinery, cars, trucks, motorcycles, motor boats or loud music.
Table 2.
Sex- and Age-Adjusted Odds Ratios (OR) and 95% Confidence Intervals (CI) for Hearing Impairment (>25 dB Hearing Level [HL]) Comparisons of NHANES 2011–2012 Versus the Reference Population, NHANES 1999–2004, for Each Pure-Tone Frequency and for the Speech-Frequency and High-Frequency Pure-Tone Average (PTA) by Better and Worse Ear
| U.S. Adults, Aged 20–69 Years | ||||||
|---|---|---|---|---|---|---|
| Ear | Pure-Tone Frequency (ies) |
Survey (Reference: NHANES 1999–2004) |
OR | Lower 95% CI |
Upper 95% CI |
P-Value |
| BETTER | 0.5 kHz | NHANES 2011–2012 | 0.63 | 0.41 | 0.96 | .03 |
| 1 kHz | NHANES 2011–2012 | 1.22 | 0.88 | 1.70 | .23 | |
| 2 kHz | NHANES 2011–2012 | 0.79 | 0.60 | 1.05 | .10 | |
| 3 kHz | NHANES 2011–2012 | 0.88 | 0.71 | 1.09 | .23 | |
| 4 kHz | NHANES 2011–2012 | 0.72 | 0.60 | 0.88 | .002 | |
| 6 kHz | NHANES 2011–2012 | 0.82 | 0.69 | 0.98 | .03 | |
| 8 kHz | NHANES 2011–2012 | 1.04 | 0.80 | 1.37 | .75 | |
| PTA of 0.5, 1, 2, & 4 kHz | NHANES 2011–2012 | 0.75 | 0.56 | 1.00 | .05 | |
| PTA of 3, 4, & 6 kHz | NHANES 2011–2012 | 0.78 | 0.64 | 0.94 | .01 | |
| WORSE | 0.5 kHz | NHANES 2011–2012 | 0.62 | 0.50 | 0.76 | <.001 |
| 1 kHz | NHANES 2011–2012 | 0.94 | 0.76 | 1.17 | .59 | |
| 2 kHz | NHANES 2011–2012 | 0.78 | 0.62 | 0.97 | .02 | |
| 3 kHz | NHANES 2011–2012 | 0.85 | 0.71 | 1.01 | .07 | |
| 4 kHz | NHANES 2011–2012 | 0.81 | 0.69 | 0.95 | .01 | |
| 6 kHz | NHANES 2011–2012 | 0.84 | 0.71 | 0.98 | .03 | |
| 8 kHz | NHANES 2011–2012 | 1.19 | 0.95 | 1.49 | .14 | |
| PTA of 0.5, 1, 2, & 4 kHz | NHANES 2011–2012 | 0.70 | 0.56 | 0.86 | .001 | |
| PTA of 3, 4, & 6 kHz | NHANES 2011–2012 | 0.75 | 0.65 | 0.88 | .001 | |
High-frequency HI was more prevalent than speech-frequency HI, affecting 31% (61 million) as compared to 32% in 1999–2004.14 While the apparent reduction between 2011–2012 and 1999–2004 appears slight, after adjustment for age and sex (Table 2), the decline in high-frequency, worse ear HI is also statistically significant, OR=0.75 (95% CI: 0.65–0.88).
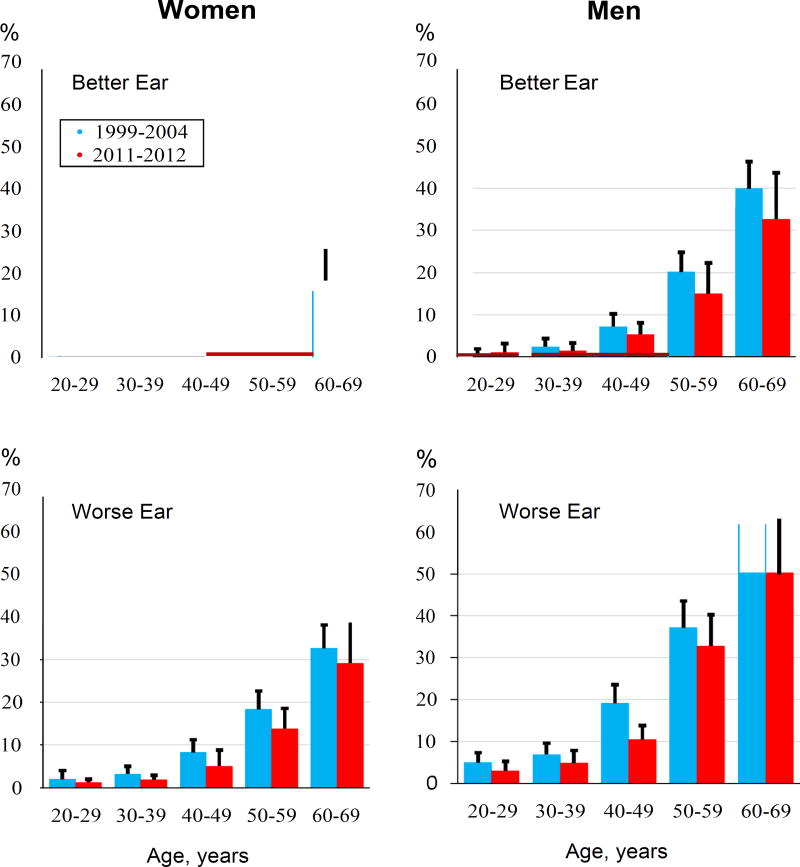
The overwhelming effect of age is apparent in all four panels of the Figure in which the 2011–2012 and 1999–2004 data are shown graphically for speech-frequency HI, by age (in decades), with separate panels for men and women, better and worse ears. For almost all age groups and both sexes, prevalence is lower in the more recent survey, although most 95% CIs overlap. A more informative comparison of 2011–2012 to 1999–2004 NHANES data is shown in Table 2, which adjusts for age and sex, since there were relatively more adults aged 50–59 and 60–69 years in 2011–2012. For most audiometric frequencies except 1 kHz (better ear) and 8 kHz (both ears), the age- and sex-adjusted ORs in Table 2 were less than one, suggesting better hearing in 2011–2012. Statistical significance was found for high-frequency HI, better and worse ear, and for speech-frequency HI in the worse ear, while the better ear was borderline significant (p=.053).
Figure. Speech-Frequency HI Prevalence, NHANES 1999–2004 versus 2011–2012.
Comparison of adult speech-frequency hearing impairment (HI) prevalences for U.S. NHANES 1999–2004 versus 2011–2012 by age (decades: 20–29, 30–39, 40–49, 50–59, 60–69) for: i) men, better ear (top left panel); ii) women, better ear (top right); iii) men, worse ear (bottom left); and iv) women, worse ear (bottom right).
Nearly twice as many men, 18.6% (17.8 million) had speech-frequency HI, compared to women, 9.6% (9.7 million). Bilateral high-frequency HI prevalence was even greater in men, 28% (26.9 million), compared to women, 11% (11.1 million). The speech-frequency HI prevalence reaches 39.3% for age 60–69 and, for all categories of HI, prevalence rises sharply above age 30–39. The prevalence of bilateral speech-frequency HI rises almost 25-fold over three decades of age, roughly three-fold per decade.
Other factors significantly associated with hearing impairment were NH white race, lower educational attainment, occupational noise exposure, use of firearms (≥1000 rounds), smoking (≥20 pack-years), hypertension, and diabetes. Many of these risk factors are correlated with one another; for example, diabetes is more prevalent in older people.
A clearer understanding of HI risks requires multivariable analysis (Table 3). All demographic, noise exposure, and cardiovascular risk factors are analyzed with logistic regression models showing associations for bilateral (better ear) speech-frequency HI in the unadjusted, age- and sex-adjusted, and multivariable-adjusted analyses in the last three columns. Unadjusted odds ratios confirm that each of the risk factors listed in the previous paragraph is associated with increased HI prevalence. The next column shows ORs adjusted for age and sex; odds ratios for hypertension and diabetes are no longer significant.
TABLE 3.
Prevalence (%) and Odds Ratios (OR) and 95% Confidence Intervals (CI) of Bilateral (Better Ear) Speech-Frequency Hearing Impairment (HI) for U.S. Adults Aged 20–69 Years by Demographic Characteristics, Noise Exposures, and Cardiovascular Risk Factors, NHANES, 2011–2012
| Bilateral (Better Ear) Speech-Frequency Hearing Impairment (HI)a | ||||
|---|---|---|---|---|
|
|
||||
| Prevalence | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| %b (95% CI) | Unadjusted | Adjusted for age and sex |
Adjusted for all variables shown |
|
| Total | 7.5 (5.8–9.6) | |||
| Demographic risk factors | ||||
| Sex | ||||
| Male | 9.9 (7.3–13.3) | 2.0 (1.3–3.2) | 2.4 (1.4–3.9) | 1.8 (1.1–3.0) |
| Female | 5.1 (3.6–7.3) | 1.0 | 1.0 | 1.0 |
| Age, years | ||||
| 20–29 | 0.8 (0.3–2.3) | 1.0 | 1.0 | 1.0 |
| 30–39 | 0.9 (0.4–2.1) | 1.2 (0.3–4.6) | 1.2 (0.3–4.6) | 1.1 (0.3–4.4) |
| 40–49 | 3.4 (2.1–5.6) | 4.4 (1.3–15.4) | 4.4 (1.3–15.3) | 3.3 (0.8–13.3) |
| 50–59 | 11.2 (7.5–16.6) | 15.6 (4.2–58.2) | 16.2 (4.4–59.9) | 13.4 (2.8–63.5) |
| 60–69 | 24.7 (20.2–29.9) | 40.5 (13.4–122.3) | 43.3 (14.5–128.9) | 39.5 (10.5–149.4) |
| Race/ethnicity | ||||
| NHc White | 9.0 (7.1–11.5) | 2.3 (1.4–3.8) | 2.0 (1.2–3.1) | 2.3 (1.3–3.9) |
| NHc Black | 4.1 (2.7–−6.2) | 1.0 | 1.0 | 1.0 |
| Mexican-American | 4.3 (3.3–5.7) | 1.1 (0.7–1.8) | 1.7 (1.1–2.7) | 1.4 (0.8–2.3) |
| NHc Asian | 4.7 (2.8–7.8) | 1.2 (0.6–2.2) | 1.4 (0.8–2.6) | 2.1 (1.1–4.2) |
| Other Hispanic | 3.9 (1.9–7.7) | 1.0 (0.4–2.1) | 1.2 (0.6–2.2) | 1.2 (0.6–2.3) |
| Other race | 7.4 (2.3–21.2) | 1.9 (0.5–6.8) | 1.7 (0.7–4.2) | 1.4 (0.6–3.3) |
| Education | ||||
| < High school | 11.3 (8.5–14.8) | 3.1 (1.8–5.3) | 3.8 (2.2–6.7) | 4.2 (2.1–8.5) |
| High school diploma | 9.5 (6.5–13.5) | 2.5 (1.3–4.9) | 3.0 (1.5–5.8) | 2.8 (1.2–6.9) |
| Some college/AA degree | 8.3 (5.5–12.4) | 2.2 (1.2–4.2) | 2.8 (1.5–5.3) | 2.4 (1.2–4.9) |
| College graduate or above | 4.0 (2.6–6.0) | 1.0 | 1.0 | 1.0 |
| Cardiovascular Risk Factors | ||||
| Smoking (number of pack-years) | ||||
| Nonsmoker | 5.8 (4.2–7.9) | 1.0 | 1.0 | 1.0 |
| <20 | 2.7 (1.6–4.6) | 0.5 (0.2–0.9) | 0.5 (0.3–1.0) | 0.5 (0.2–1.0) |
| ≥20 | 14.6 (12.0–17.7) | 2.8 (2.1–3.7) | 1.5 (1.0–2.1) | 1.0 (0.7–1.5) |
| Unknown | 10.7 (4.2–24.9) | 2.0 (0.7–5.7) | 2.2 (0.7–7.0) | 2.0 (0.6–6.2) |
| History of hypertension | ||||
| No | 5.6 (4.1–7.6) | 1.0 | 1.0 | 1.0 |
| Yes | 11.6 (9.1–14.7) | 2.2 (1.6–3.0) | 1.0 (0.7–1.4) | 0.9 (0.6–1.3) |
| History of diabetes | ||||
| No | 6.8 (5.1–8.9) | 1.0 | 1.0 | 1.0 |
| Yes | 14.6 (12.0–17.6) | 2.4 (1.7–3.3) | 1.1 (0.8–1.6) | 1.1 (0.7–1.7) |
| Noise Exposures | ||||
| Occupational | ||||
| No | 5.5 (4.1–7.3) | 1.0 | 1.0 | 1.0 |
| Yes, “loud” only (<5 years) | 5.4 (3.0–9.6) | 1.0 (0.5–2.0) | 1.2 (0.6–2.5) | 1.0 (0.5–2.2) |
| Yes, “loud” only (≥5 years) | 10.0 (6.7–14.7) | 1.9 (1.1–3.4) | 1.5 (0.7–3.1) | 1.2 (0.5–2.6) |
| Yes, “very loud” (<5 years) | 8.9 (4.5–16.7) | 1.7 (0.8–3.4) | 2.0 (0.9–4.5) | 1.5 (0.7–3.3) |
| Yes, “very loud” (≥5 years) | 17.8 (11.9–25.7) | 3.7 (2.1–6.7) | 2.5 (1.4–4.5) | 1.5 (0.9–2.7) |
| Unknown | 2.3 (0.5–10.8) | 0.4 (0.1–2.2) | 0.4 (0.1–2.8) | 0.5 (0.1–3.1) |
| Outside of work: “very loud” noise | ||||
| No | 7.3 (5.8–9.3) | 1.0 | 1.0 | 1.0 |
| Yes | 8.6 (4.2–17.0) | 1.2 (0.6–2.5) | 1.4 (0.7–2.8) | 1.0 (0.6–1.7) |
| Firearms, includes use for recreation, job, or military | ||||
| No | 5.4 (4.3–6.8) | 1.0 | 1.0 | 1.0 |
| 1 to <1,000 rounds fired | 8.0 (5.8–10.9) | 1.5 (1.1–2.1) | 1.4 (0.9–2.1) | 1.4 (0.8–2.2) |
| 1,000 or more rounds fired | 15.2 (9.4–23.6) | 3.1 (1.7–5.7) | 2.4 (1.4–4.2) | 1.8 (1.1–3.0) |
| Noise exposure based on all noise exposures, except firearmsd | ||||
| No noise | 5.5 (4.1–7.3) | 1.0 | 1.0 | 1.0 |
| Loud job noise only | 7.7 (5.5–10.7) | 1.4 (0.9–2.4) | 1.4 (0.8–2.5) | 1.1 (0.6–2.0) |
| Loud and very loud job noise | 12.2 (7.9–18.5) | 2.4 (1.4–4.1) | 2.0 (1.1–3.6) | 1.4 (0.7–2.5) |
| Loud job noise, very loud job noise and loud noise outside of work | 15.6 (7.3–30.4) | 3.2 (1.3–8.2) | 3.2 (1.4–7.3) | 2.1 (1.0–4.4) |
Speech-frequency hearing impairment (HI) is defined by the PTA of thresholds across 0.5–1–2–4 kHz greater than 25 dB HL in the better ear
SUDAAN weighted percent
NH is an abbreviation for non-Hispanic
Included in a separate model in place of the three variables – loud job noise, very loud job noise and loud noise outside of work – shown above the solid line
The last column of Table 3 shows ORs fully adjusted for all risk factors. Age is again by far the best predictor of HI; the odds ratio for age 60–69, compared to the reference age 20–29 group, is 39.5. Aside from age, the risk factor most associated with risk of HI was “less than a high school education,” with an OR of 4.2 (95% CI: 2.1–8.5). Male sex, NH white race, and lower educational attainment remained significant predictors of HI, but no cardiovascular variables retained statistically significant ORs. Of the noise exposure variables, only heavy firearms use was significant, OR=1.8 (95%CI: 1.1–3.0).
Since hearing loss in the speech frequencies is not as sensitive to noise (and some other exposures) as the higher frequencies, we have also evaluated all demographic, noise exposure, and cardiovascular variables where the outcome or dependent variable is hearing loss as determined by the bilateral (better ear) high-frequency HI (Table 4). Several variables have stronger associations (compared to Table 3) in the multivariable model with high-frequency HI, including male sex, OR=3.8 (95% CI: 2.7–5.4), possibly diabetes, OR=1.5 (95% CI: 0.9–2.6; borderline p=0.08), and exposure to very loud (≥5 years) occupational noise, OR=1.5 (95% CI: 1.3–2.9).
TABLE 4.
Prevalence (%) and Odds Ratios (OR) and 95% Confidence Intervals (CI) of Bilateral (Better Ear) High-Frequency Hearing Impairment (HI) for U.S. Adults Aged 20–69 Years by Demographic Characteristics, Noise Exposures, and Cardiovascular Risk Factors, NHANES, 2011–2012
| Bilateral (Better Ear) High Frequency Hearing Impairment (HI)a | ||||
|---|---|---|---|---|
|
|
||||
| Prevalence %b (95% CI) |
OR (95% CI) Unadjusted |
OR (95% CI) Adjusted for age and sex |
OR (95% CI) Adjusted for all variables shown |
|
| Total | 19.1 (16.6–21.9) | |||
| Demographic risk factors | ||||
| Sex | ||||
| Male | 27.6 (23.0–32.8) | 3.2 (2.3–4.5) | 4.8 (3.3–6.9) | 3.8 (2.7–5.4) |
| Female | 10.6 (8.6–13.0) | 1.0 | 1.0 | 1.0 |
| Age, years | ||||
| 20–29 | 2.1 (1.0–4.2) | 1.0 | 1.0 | 1.0 |
| 30–39 | 3.0 (1.7–5.3) | 1.5 (0.6–3.8) | 1.5 (0.5–3.9) | 1.2 (0.5–3.4) |
| 40–49 | 14.7 (11.0–19.4) | 8.1 (3.8–17.3) | 8.7 (4.3–17.8) | 6.9 (3.3–14.2) |
| 50–59 | 30.8 (25.2–37.1) | 21.1 (8.8–50.4) | 25.3 (11.1–57.8) | 20.5 (8.7–48.6) |
| 60–69 | 50.1 (43.7–58.5) | 49.4 (20.4–119.7) | 68.3 (28.2–165.5) | 63.6 (24.8–163.4) |
| Race/ethnicity | ||||
| NHc White | 21.4 (18.7–24.5) | 2.1 (1.5–2.9) | 1.9 (1.3–2.6) | 2.2 (1.5–3.1) |
| NHc Black | 11.7 (9.3–14.6) | 1.0 | 1.0 | 1.0 |
| Mexican-American | 15.1 (12.5–18.0) | 1.3 (1.0–1.9) | 2.4 (1.7–3.5) | 2.0 (1.3–3.1) |
| NHc Asian | 13.9 (10.0–18.4) | 1.2 (0.8–1.9) | 1.5 (1.4–3.4) | 2.4 (1.6–3.6) |
| Other Hispanic | 16.8 (11.9–23.2) | 1.5 (0.9–2.5) | 2.2 (1.4–3.4) | 2.4 (1.4–4.0) |
| Other race | 21.6 (13.1–33.5) | 2.1 (1.1–3.8) | 2.2 (1.2–4.2) | 1.9 (1.0–3.5) |
| Education | ||||
| < High school | 28.2 (24.2–32.6) | 2.3 (1.6–3.3) | 3.2 (1.9–5.4) | 2.9 (1.7–4.9) |
| High school diploma | 25.1 (21.8–28.7) | 2.0 (1.3–2.9) | 2.4 (1.5–4.0) | 2.2 (1.3–3.6) |
| Some college/AA degree | 16.3 (12.1–21.6) | 1.1 (0.8–1.7) | 1.5 (0.9–2.3) | 1.2 (0.7–2.0) |
| College graduate or above | 14.6 (11.4–18.4) | 1.0 | 1.0 | 1.0 |
| Cardiovascular Risk Factors | ||||
| Smoking (number of pack-years) | ||||
| Nonsmoker | 14.8 (11.9–18.3) | 1.0 | 1.0 | 1.0 |
| <20 | 13.1 (8.7–19.1) | 0.9 (0.5–2.0) | 1.0 (0.5–2.0) | 0.9 (0.4–1.8) |
| ≥20 | 34.8 (31.2–38.5) | 3.1 (2.1–3.7) | 1.5 (1.0–2.1) | 1.1 (0.8–1.6) |
| Unknown | 12.6 (7.1–21.4) | 0.8 (0.4–1.7) | 0.7 (0.3–1.6) | 0.6 (0.3–1.2) |
| History of hypertension | ||||
| No | 14.2 (11.9–17.9) | 1.0 | 1.0 | 1.0 |
| Yes | 29.6 (26.2–33.3) | 2.5 (2.1–3.1) | 1.1 (0.9–1.4) | 1.0 (0.8–1.4) |
| History of diabetes | ||||
| No | 17.0 (15.0–19.2) | 1.0 | 1.0 | 1.0 |
| Yes | 39.5 (30.2–49.6) | 3.2 (2.2–4.7) | 1.6 (1.0–2.5) | 1.5 (0.9–2.6) |
| Noise Exposures | ||||
| Occupational | ||||
| No | 14.2 (12.8–15.7) | 1.0 | 1.0 | 1.0 |
| Yes, “loud” only (<5 years) | 16.3 (11.0–23.4) | 1.2 (0.7–1.9) | 1.2 (0.7–2.1) | 1.0 (0.6–1.9) |
| Yes, “loud” only (≥5 years) | 28.3 (20.8–37.3) | 2.4 (1.5–3.8) | 1.7 (0.9–3.3) | 1.3 (0.7–2.5) |
| Yes, “very loud” (<5 years) | 20.7 (14.8–28.2) | 1.6 (1.1–2.3) | 1.7 (1.0–2.8) | 1.3 (0.8–2.3) |
| Yes, “very loud” (≥5 years) | 42.8 (34.5–51.4) | 4.5 (3.2–6.3) | 2.8 (1.9–4.0) | 2.0 (1.3–2.9) |
| Unknown | 10.3 (4.6–21.4) | 0.7 (0.3–1.7) | 0.7 (0.2–3.3) | 0.8 (0.3–2.5) |
| Outside of work: “very loud” noise | ||||
| No | 18.3 (16.0–20.9) | 1.0 | 1.0 | 1.0 |
| Yes | 24.6 (18.1–32.5) | 1.5 (1.0–2.1) | 1.7 (1.1–2.7) | 1.4 (0.9–2.2) |
| Firearms, includes use for recreation, job, or military | ||||
| No | 14.4 (12.7–16.3) | 1.0 | 1.0 | 1.0 |
| 1 to <1,000 rounds fired | 22.1 (17.6–27.4) | 1.7 (1.3–2.2) | 1.4 (0.9–2.1) | 1.4 (0.9–2.3) |
| 1,000 or more rounds fired | 31.7 (22.5–42.6) | 2.8 (1.6–4.7) | 1.5 (1.0–2.5) | 1.3 (0.7–2.3) |
| Noise exposure based on all noise exposures, except firearmsd | ||||
| No noise | 14.2 (12.8–15.7) | 1.0 | 1.0 | 1.0 |
| Loud job noise only | 22.3 (17.3–28.3) | 1.7 (1.2–2.5) | 1.5 (0.9–2.5) | 1.2 (0.7–1.9) |
| Loud and very loud job noise | 30.1 (23.7–37.4) | 2.6 (2.0–3.5) | 2.0 (1.4–2.9) | 1.5 (1.0–2.3) |
| Loud job noise, very loud job noise and loud noise outside of work | 34.1 (24.3–45.5) | 3.1 (2.0–5.0) | 2.9 (1.6–5.0) | 2.4 (1.4–4.2) |
High-Frequency hearing impairment (HI) is defined by the PTA of thresholds across 3–4–6 kHz greater than 25 dB HL in the better ear
SUDAAN weighted percent
NH is an abbreviation for non-Hispanic
Included in a separate model in place of the three variables – loud job noise, very loud job noise and loud noise outside of work – shown above the solid line
Discussion
Age-adjusted prevalence of HI in adults (aged 20–69) declined from 1999–2004 to 2011–2012. However, the U.S. population grew during that decade and the age distribution also changed, with disproportionate growth (augmented by baby boomers) of older adults who are more likely to be hearing-impaired. Based on NHANES tabulation of Census Bureau estimates in 2011–2012, there were 196.6 million civilian, noninstitionalized U.S. adults, which is 20 million more than the average annual number of 176.2 million in 1999–2004. The relative shift in percentage of adults aged 60–69 was 34.8% (increasing from 11.5% to 15.5% among adults aged 20–69) and, similarly, the percentage of adults aged 50–59 grew18.9% (increasing from 18.1% to 21.5%). In spite of these unfavorable demographic shifts, the estimated number of adults aged 20–69 years with hearing loss actually declined absolutely from an estimate of 28.0 million in 1999–2004 to 27.7 million in 2011–2012. The reason is the decrease in overall prevalence from 16% to 14.1%. The percentage decrease of adults with hearing loss is small, <1%; however, one could have expected the opposite result based on the changing demographic figures. Hence, the decrease in overall prevalence of hearing loss between the two time periods was sufficient to reduce (slightly) the number of adults aged 20–69 with hearing loss. The continuing decline in HI prevalence for adults 20–69 years may represent delay of the onset of age-related hearing loss. Audiometric testing of adults aged 70 and above was not conducted during the 1999–2004 or 2011–2012 survey cycles, but this group has a much higher HI prevalence than any of the age groups shown in Table 1,15,16 and their relative numbers are expected to continue growing rapidly.17
This finding of declining age-adjusted HI prevalence, combined with both our earlier reports showing improvement of hearing between 1959–1962 and 1999–2004,1,16 and similar findings by others, for example, the Beaver Dam, WI hearing loss studies,18 suggests a beneficial trend that spans at least half a century. Explanations for this trend are unavoidably speculative, but could include reduction in occupational noise exposure (fewer manufacturing jobs, more use of hearing protection devices), less smoking, and better management of other cardiovascular risk factors such as hypertension and diabetes. Less plausible explanations, especially for beneficial changes in the most recent decade, might include fewer and better-managed ear infections and better diet.
Male sex and NH white race continue to be significant risk factors for HI, even after accounting for risk factors that might be more prevalent in NH white men, such as noise exposure. The typical noise exposures of men and women are different, especially at high exposure levels.19 Although we controlled for noise exposure and sex in the multivariable analyses, it remains possible the noise exposure questions asked were inadequate to represent lifetime noise exposure, in which case there may have been residual confounding.20,21 In spite of this concern, we suspect there are major contributions that are genetic and probably not amenable to clinical intervention.22–24 On the other hand, lower educational attainment is a risk factor for many adverse health outcomes and could be linked to less access to medical care in childhood, poorer diet, and other concomitants of lower socioeconomic status including increased noise exposure.
Our finding of non-significance for cardiovascular risk factors and occupational noise in the fully adjusted model contrasts with the report of Agrawal et al.25 This cannot be attributed to sample size (3,831 for this study versus 3,527 for their analysis), but could be related to better medical management of these risk factors in recent years, as well as more consistent use of hearing protection in industry.26–29 Recreational shooting, which often occurs without hearing protection remains a significant risk factor for hearing impairment, for both speech frequencies and high frequencies, and for both better and worse ears. In this study, we analyzed lower (less than 1000 lifetime shots) and higher (1000 or more) gunfire exposure separately and found that only the higher exposure predicted hearing impairment in the unadjusted and adjusted analyses (Table 3). Recall bias must be considered in all of these analyses: for example, people who know they are hearing-impaired could be more likely to remember and report high levels of recreational shooting or other use of firearms.
One limitation of our study is the necessarily abbreviated NHANES questionnaires used for occupational and recreational noise exposure and other risk factors. One can question their adequacy for capturing noise exposure information across the adult lifespan. We doubt this problem is sufficient to invalidate the findings when comparing results from NHANES 2011–2012 with 1999–2004,14 since the questions about noise exposure and other risk factors were similar. An innovation in the 2011–2012 questionnaire was the distinction between loud (“need to speak in a raised voice to be heard/understood”) versus very loud (“need to shout to be heard/understood”) noise exposure. Associations by degree and extent of noise exposure are evident, illustrating face validity between self-reported exposure and expected increases in prevalence and risk estimates.
Age, even after adjustment for other risk factors thought to be important, remains by far the strongest predictor of HI, although the Figure suggests a different pattern of age-related hearing loss for men and women, with earlier age of onset and more pronounced HI for men. These differences may have a genetic basis; alternatively, they could be in part attributable, despite our adjustment for self-reported noise exposure, to more sustained, higher-intensity noise exposures in men.
Another question regarding higher HI prevalence in men versus women is whether there have been relative changes during this time period – is the gap widening or closing? The overall speech-frequency HI prevalence for men was 21.0% in 1999–2004,14 and in 2011–2012, it was 18.6% (Table 1), an 11.4% decline. Changes for women were similar: speech-frequency HI was 11.0% in 1999–2004,14 and in 2011–2012, it was 9.6%, a 12.7% decline. Hence, there was no difference in relative decline of HI prevalence between men and women.
No intervention has yet been shown to prevent the progression of age-related hearing loss. Hearing aids can improve speech communication, but they are not used by most people with hearing loss.30,31 Several studies, including in countries that subsidize hearing aid cost, have demonstrated many barriers other than cost: self-perceived disability, self-perceived likelihood of benefit/lack of benefit, and hearing aid comfort and appearance.32,33 Reducing obstacles to hearing aid use through educating patients about the importance of amplification, training health professionals to understand and overcome barriers, improving quality and affordability of devices, and increasing access to hearing health services34–37 are important public health objectives in view of the high prevalence of hearing loss in the U.S. adult population.
Acknowledgments
Dr. Dobie is a member of the faculties of The University of Texas Health Science Center at San Antonio and the University of California at Davis, and also has a private consulting practice in otology; Dr. Flamme is a member of the faculty of Western Michigan University, Kalamazoo, MI, and also has a private consulting practice in audiology.
Funding/Support: Ms. Themann was supported in part by an Interagency Agreement between the National Institute on Deafness and Other Communication Disorders (NIDCD), NIH with the National Institute for Occupational Safety and Health (NIOSH), CDC.
Role of the Funder/Sponsor: The National Health and Nutrition Examination Survey (NHANES) is conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention. The NIDCD helped fund the hearing component of the NHANES and had input into the design and conduct of the study, and the collection and management of the data with regard to the hearing-related data. Other than the authors, the NIDCD and NIOSH had no role in the design, analysis, and interpretation of the secondary analysis of data; preparation, review, and approval of the manuscript; and the decision to submit the manuscript for publication.
Footnotes
Author Contributions: Mr. Hoffman and Ms. Losonczy had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Hoffman, Dobie
Acquisition of data: Hoffman, Themann
Analysis and interpretation of data: Hoffman, Dobie, Losonczy, Themann, Flamme (the order of the authors is intended to reflect the contribution each made to the paper)
Drafting of the manuscript: Dobie, Hoffman
Critical revision of the manuscript for important intellectual content: Hoffman, Dobie, Themann, Flamme
Statistical analysis: Losonczy, Hoffman, Flamme
Obtained funding: Hoffman, Themann
Administrative, technical, and material support: Hoffman, Themann
Study supervision: Hoffman, Dobie, Themann
Conflict of Interest Disclosures: Three authors, Hoffman, Losonczy, and Themann, are U.S. Federal employees; they have no conflicts of interest to declare. Dr. Dobie and Dr. Flamme have no other financial or potential conflicts of interest to declare.
Disclaimer: Any analyses, interpretations, or conclusions reached are those of the authors; they do not necessarily represent the official positions of the U.S. governmental agencies, NIDCD and NIOSH, or academic institutions for which the authors work.
Additional Contributions: We are grateful to the adult subjects who participated in these NHANES audiometric surveys and we also appreciate the efforts of the NCHS staff who worked with Westat, Inc. to implement, coordinate, and conduct the NHANES Audiometry Examination Protocols and Questionnaires. NIDCD co-funded the NHANES Audiometry Component via Interagency Agreements with NCHS and NIOSH. May Chiu, Epidemiology and Statistics Program, NIDCD, assisted with preparation of the Tables and Figure.
References
- 1.Hoffman HJ, Dobie RA, Ko C-W, Themann CL, Murphy WJ. Americans hear as well or better today compared with 40 years ago: Hearing threshold levels in the unscreened adult population of the United States, 1959–1962 and 1999–2004. Ear Hear. 2010;31:725–734. doi: 10.1097/AUD.0b013e3181e9770e. [DOI] [PubMed] [Google Scholar]
- 2.Curtin LR, Mohadjer LK, Dohrmann SM, et al. The National Health and Nutrition Examination Survey: Sample Design, 1999–2006. Vol. 155. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; May, 2012. pp. 1–39. DHHS Publication No. (PHS) 2012–1355, Series 2. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey: NHANES 2011–2012 Overview. [Accessed May 23, 2016]; http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/overview_g.htm.
- 4.American National Standards Institute (ANSI) ANSI S3.1–1991. New York, NY: ANSI; 1991. Maximum permissible ambient noise levels for audiometric test rooms. [Google Scholar]
- 5.American National Standards Institute (ANSI) ANSI S3.1–1999. New York, NY: ANSI; 1999. Maximum permissible ambient noise levels for audiometric test rooms. [Google Scholar]
- 6.American National Standards Institute. ANSI S3.6–1996. New York, NY: ANSI; 1996. Specifications for audiometers. [Google Scholar]
- 7.National Health and Nutrition Examination Survey Audiometry Procedures Manual. Hyattsville, MD: Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS); Jan, 2003. [Accessed May 23, 2016]. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/AU.pdf. [Google Scholar]
- 8.Hyattsville, MD: Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS); Jan, 2011. [Accessed May 23, 2016]. National Health and Nutrition Examination Survey (NHANES) Audiometry Procedures Manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Audiometry_Procedures_Manual.pdf. [Google Scholar]
- 9.Carhart R, Jerger JF. Preferred method for clinical determination of pure-tone thresholds. J Speech Hear Disord. 1959;24(4):330–345. [Google Scholar]
- 10.Lutman ME, Qasem HYN. A source of notches at 6 kHz. In: Prasher D, Luxon L, editors. Advances on Noise Research, Volume 1: Biological Effects of Noise. London: Whurr; 1998. pp. 170–176. [Google Scholar]
- 11.Flamme GA, Stephenson MR, Deiters KK, et al. Short-term variability of pure-tone thresholds obtained with TDH-39P earphones. Int J Audiol. 2014;53:S5–S15. doi: 10.3109/14992027.2013.857435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis AC. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int J Epidemiol. 1989;18(4):911–917. doi: 10.1093/ije/18.4.911. [DOI] [PubMed] [Google Scholar]
- 13.Dobie RA. The AMA method of estimation of hearing disability: a validation study. Ear Hear. 2011;32:732–740. doi: 10.1097/AUD.0b013e31822228be. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999–2004. Arch Intern Med. 2008;168(14):1522–1530. doi: 10.1001/archinte.168.14.1522. [DOI] [PubMed] [Google Scholar]
- 15.Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. [Letter to the Editor] Arch Intern Med. 2011;171(20):1851–1852. doi: 10.1001/archinternmed.2011.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoffman HJ, Dobie RA, Ko CW, Themann CL, Murphy WJ. Hearing threshold levels at age 70 years (65–74 years) in the unscreened older adult population of the United States, 1959–1962 and 1999–2004. Ear Hear. 2012;33(3):437–440. doi: 10.1097/AUD.0b013e3182362790. [DOI] [PubMed] [Google Scholar]
- 17.Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. Washington, DC: U.S. Census Bureau, Current Population Reports; 2014. P25-1140. [Google Scholar]
- 18.Zhan W, Cruickshanks KJ, Klein BE, et al. Generational differences in the prevalence of hearing impairment in older adults. Am J Epidemiol. 2010;171(2):260–266. doi: 10.1093/aje/kwp370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flamme GA, Stephenson MR, Deiters K, et al. Typical noise exposure in daily life. Int J Audiol. 2012;51(Suppl 1):S3–S11. doi: 10.3109/14992027.2011.635316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson DI, Nelson RY, Concha-Barrientos MC, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48(6):446–458. doi: 10.1002/ajim.20223. [DOI] [PubMed] [Google Scholar]
- 21.El Dib RP, Silva EM, Morais JF, Trevisani VF. Prevalence of high frequency hearing loss consistent with noise exposure among people working with sound systems and general population of Brazil: a cross-sectional study. BMC Public Health. 2008;8:151–159. doi: 10.1186/1471-2458-8-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gates GA, Couropmitree NN, Myers RH. Genetic associations in age-related hearing thresholds. Arch Otolaryngol Head Neck Surg. 1999;125:654–659. doi: 10.1001/archotol.125.6.654. [DOI] [PubMed] [Google Scholar]
- 23.Christensen K, Frederiksen H, Hoffman HJ. Genetic and environmental influences on self-reported reduced hearing in the old and oldest old. J Am Geriatr Soc. 2001;49:1512–1517. doi: 10.1046/j.1532-5415.2001.4911245.x. [DOI] [PubMed] [Google Scholar]
- 24.Kvestad E, Czajkowski N, Krog NH, Engdahl B, Tambs K. Heritability of hearing loss. Epidemiology. 2012;23(2):328–331. doi: 10.1097/EDE.0b013e318245996e. [DOI] [PubMed] [Google Scholar]
- 25.Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009;30(2):139–145. doi: 10.1097/MAO.0b013e318192483c. [DOI] [PubMed] [Google Scholar]
- 26.Davis RR, Sieber WK. Trends in hearing protector usage in American manufacturing from 1972 to 1989. Am Ind Hyg Assoc J. 1998;59(10):715–722. doi: 10.1080/15428119891010893. [DOI] [PubMed] [Google Scholar]
- 27.Tak S, Davis RR, Calvert GM. Exposure to hazardous workplace noise and use of hearing protection devices among US workers–NHANES, 1999–2004. Am J Ind Med. 2009;52(5):358–371. doi: 10.1002/ajim.20690. [DOI] [PubMed] [Google Scholar]
- 28.Joy GJ, Middendorf PJ. Noise exposure and hearing conservation in U.S. coal mines—A surveillance report. J Occup Environ Hyg. 2007;4(1):26–35. doi: 10.1080/15459620601067209. [DOI] [PubMed] [Google Scholar]
- 29.Masterson EA, Deddens JA, Themann CL, Bertke S, Calvert GM. Trends in worker hearing loss by industry sector, 1981–2010. Am J Ind Med. 2015;58:392–401. doi: 10.1002/ajim.22429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. [Letter to the Editor] Arch Intern Med. 2012;172(3):292–293. doi: 10.1001/archinternmed.2011.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bainbridge KE, Ramachandran V. Hearing aid use among older U.S. adults: The National Health and Nutrition Examination Survey, 2005–2006 and 2009–2010. Ear Hear. 2014;35(3):289–294. doi: 10.1097/01.aud.0000441036.40169.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fisher DE, Li CM, Hoffman HJ, et al. Sex-specific predictors of hearing-aid use in older persons: The Age, Gene/Environment Susceptibility–Reykjavik Study. Int J Audiol. 2015;54(9):634–641. doi: 10.3109/14992027.2015.1024889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gopinath B, Schneider J, Hartley D, et al. Incidence and predictors of hearing-aid use and ownership among older adults with hearing loss. Ann Epidemiol. 2011;21:497–506. doi: 10.1016/j.annepidem.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Laplante-Lévesque A, Hickson L, Worrall L. What makes adults with hearing impairment take up hearing AIDS or communication programs and achieve successful outcomes? Ear Hear. 2012;33(1):79–93. doi: 10.1097/AUD.0b013e31822c26dc. [DOI] [PubMed] [Google Scholar]
- 35.Nash SD, Cruickshanks KJ, Huang GH, et al. Unmet hearing health needs: The Beaver Dam Offspring Study. Am J Public Health. 2013;103:1134–1139. doi: 10.2105/AJPH.2012.301031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meyer C, Hickson L, Fletcher A. Identifying the barriers and facilitators to optimal hearing aid self-efficacy. Int J Audiol. 2014;53:S28–S37. doi: 10.3109/14992027.2013.832420. [DOI] [PubMed] [Google Scholar]
- 37.Blustein J, Weinstein BE. Opening the market for lower cost hearing aids: regulatory change can improve the health of older Americans. Am J Public Health. 2016;106(6):1032–1035. doi: 10.2105/AJPH.2016.303176. [DOI] [PMC free article] [PubMed] [Google Scholar]