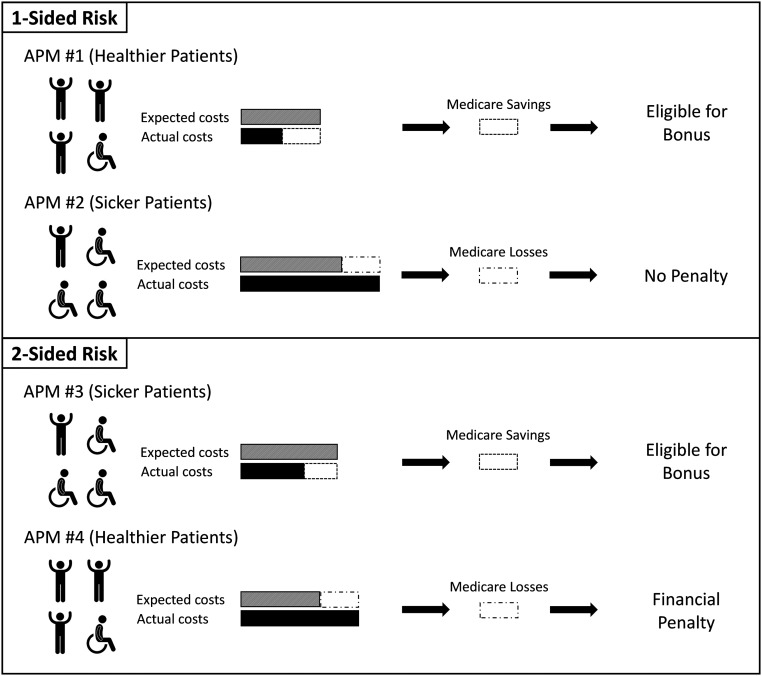
Figure 2.
Calculating shared savings and losses for the APMs. The CMS takes the population of patients within an APM and computes the risk-adjusted expected cost for the year. The APMs (2 and 3) that have sicker populations of patients will have higher expected costs. The APMs’ actual costs are then compared with expected costs. For providers taking on one-sided risk (1 and 2), if actual costs are less than expected costs, the APMs receive a portion of the shared savings as a bonus. However, if actual costs exceed expected costs, one-sided risk APMs are shielded from the loss and do not pay a penalty. In this case, APM 2 was more expensive than expected but does not owe the CMS any penalty. The APMs with two-sided risk (3 and 4) are susceptible to both shared savings and losses, which lead to bonuses or penalties, respectively. Bonuses and penalties are calculated as a portion of shared savings and losses and determined using factors that include type of APM, number of beneficiaries, and quality score.