Abstract
The present study examined leisure activity and its association with caregiver involvement (i.e., residence and time spent with primary caregiver) in 62 middle-aged and older adults with Down syndrome (aged 30–53 years). Findings indicated that middle-aged and older adults with Down syndrome frequently participated in social and passive leisure activities, with low participation in physical and mentally stimulating leisure activities. Residence and time spent with primary caregiver were associated with participation in physical leisure activity. The findings suggest a need for support services aimed at increasing opportunities for participating in physical and mentally stimulating leisure activity by middle-aged and older adults with Down syndrome. These support services should partner with primary caregivers in order to best foster participation in physical leisure activity.
Keywords: leisure, Down syndrome, caregiving, aging
Down syndrome (DS) is estimated to occur in 1 in 733 live births (Zigman & Lott, 2007). Individuals with DS experience “accelerated aging” (e.g., Horvath et al., 2015; Moran, 2013; Patterson & Cabelof, 2012), and have a current life expectancy of about 60 years (Torr, Strydom, Patti, & Jokinen, 2010; Zigman & Lott, 2007). Little research has examined the daily lives of middle-aged and older adults with DS, and even less is known about their leisure activity, defined as pleasurable activities outside of the demands of work. Participation in leisure activity is a strong determinant of psychological well-being in middle-aged and older adults in the general population (e.g., Brajša-Žganec, Merkaš, & Šverko, 2011, Pressman et al., 2009), and in adolescents and young adults with intellectual and developmental disabilities (IDD; e.g., Badia, Orgaz, Verdugo, Ullán, & Martinez, 2011; García-Villamisar & Dattilo, 2010). Unfortunately, evidence suggests that middle-aged and older adults with DS may be at risk for low leisure activity participation. In part, the “accelerated aging” of adults with DS (i.e., early onset of neuropathological, medical, and functional features of aging) may limit leisure activity opportunities. Additionally, there are fewer formal disability support services for middle-aged and older adults with DS, as compared to services for individuals with DS at earlier life stages, and these services generally do not promote leisure activity (Browder & Cooper, 1994; Pruchno & McMullen, 2004). Given the lack of structured leisure activity support services, leisure activity participation may be reliant on the involvement of primary caregivers. The purpose of the present study was to evaluate the leisure activity of 62 middle-aged and older adults with DS (aged 30–53 years) and its association with caregiver involvement (i.e., residence and time spent with primary caregiver).
Leisure activities are not equally beneficial in terms of promoting psychological well-being. Research on the general population indicates that active leisure activity—physical (i.e., physical activities), social (i.e., activities involving interactions with others), and mentally stimulating (i.e., activities requiring cognitive engagement)—is positively related to psychological well-being. Indeed, in studies on the general population, participation in active leisure activity has been shown to lead to immediate and longer-term increases in positive affect, self-esteem, sense of belonging, and happiness (e.g., Menec, 2003; Mikkelsen et al., 2010; Reed & Ones, 2006). In contrast, a high level of passive leisure activity (i.e., activities requiring little cognitive engagement), such as watching television, is associated with poor psychological well-being (e.g., negative affect, fatigue, and low self-esteem; Kikuchi et al., 2014; Trainor, Delfabbro, Anderson, & Winefield, 2010).
To date, only a handful of studies have investigated the leisure activity of adults with DS and other types of IDD; most of these studies have focused on young adults in their 20s and assessed a limited number of leisure activities. Overall, these studies indicate a low level of physical leisure activity by young adults with DS; for example, in an early study, less than half of a sample of 71 adolescents and young adults with DS (aged 15–31 years) participated in sports on at least an occasional basis (Putnam, Pueschel, Gorder Holman, 1988). Leisure activity participation may be even lower for middle-aged and older adults with DS given their experience of “accelerated aging.” Adults with DS begin to evidence neuropathological (e.g., brain β-amyloid and tissue DNA methylation), medical (e.g., vision problems, thyroid conditions, sleep apnea, and dementia) and functional (e.g., slowing down) features of aging in their 30s, 40s, and 50s (Esbensen, 2010; Hartley et al., 2014; Hermans & Evenhuis, 2014; Horvath et al., 2015), and these features of aging may limit opportunities for physical leisure activity.
In contrast to their low levels of physical leisure activity, young adults with DS and other IDDs have been found to regularly participate in social leisure activity (Badia et al., 2011; Dusseljee, Rijken, Cardol, Curfs, & Groenewe-gen, 2011; Jobling & Cuskelly, 2002). For example, Jobling and Cuskelly (2002) reported that 83% of their sample of 110 young adults with DS (M = 27.7, SD = 7.1) reported having friends. However, there is evidence that social leisure activity declines in middle and older adulthood for individuals with DS. In one of the few studies to include a large sample of middle-aged and older adults with IDD (18–88 years [M = 42.9]), Dusseljee and colleagues (2011) found that only 35% of adults with DS in their sample had social contact with friends and/or family at least once a week. Similarly, in a longitudinal study of 38 adults with DS, Carr (2008) found that 47% of the adults with DS participated in clubs in the community at least once a week at age 30 years, but only 28% continued to participate at this level at age 40 years.
Few studies have examined mentally stimulating leisure activity in adults with DS or other types of IDD. There is evidence that a large portion of young adults with DS read and/or look through books at least once a week (79%; Carr, 2008), but little is known about other types of mentally stimulating activities (e.g., word games and crossword puzzles). Finally, previous studies indicate that young adults with DS and other types of IDD frequently participate in passive leisure activities (e.g., watching television; Buttimer & Tierney, 2005; Carr, 2008; Jobling & Cuskelly, 2002). Given evidence of reduced participation in active leisure activity during middle and older adulthood, level of participation in passive leisure activity may be particularly high during these later life stages.
Caregiver involvement may play a key role in facilitating the active leisure activity of middle-aged and older adults with DS. Many individuals with DS live with their parents or family members (e.g., siblings) into middle and older adulthood; others live in group homes or independent living situations with varying levels of support from caregivers (McGuire & Chicoine, 2006). Although a previous study found no difference in overall leisure activity for adults with IDD based on residence (Badia et al., 2011), there is also evidence that adults with DS living with family participate in more social leisure activities than adults with DS not living with family. In group homes and independent living situations, adults with DS often have limited transportation (Buttimer & Tierney, 2005), making it difficult to access leisure activities in the community. Indeed, Hall and Hewson (2006) found that 88% of adults with IDD living in group homes or independent living situations went into the community less than once a day. Moreover, in studies of adolescents and young adults with IDD, family members played a key role in organizing social leisure activities (more so than agency providers) for the individual with IDD, and were more likely to be social partners in these activities than agency providers (Buttimer & Tierney, 2005; Jobling & Cuskelly, 2002). The need for caregivers to facilitate active leisure activity may increase in middle and older adulthood, given reductions in formal support services in the later life stages (Browder & Cooper, 1994; Pruchno & McMullen, 2004), and age-related reductions in the physical and cognitive resources of the adult with DS. Thus, regardless of residence, time spent with primary caregivers (whether family, agency provider, or other) may be positively associated with the active leisure activity of middle-aged and older adults with DS.
The aims of the present study were to: 1) determine the extent to which middle-aged and older adults with DS participate in active (i.e., physical, social, and mentally stimulating) and passive leisure activity, and 2) evaluate the association between caregiver involvement (i.e., residence and time spent with primary caregiver) and the level of active and passive leisure activity of middle-aged and older adults with DS. Based on previous studies of young adults with DS and other types of IDD (e.g., Badia et al., 2011; Buttimer & Tierney, 2005), we predicted that middle-aged and older adults with DS would participate in a higher level of social and passive leisure activity than physical and mentally stimulating leisure activity. In addition, middle-aged and older adults with DS co-residing with family were hypothesized to participate in a higher level of active leisure activity than adults with DS residing in group homes or independent living situations. Time spent with a primary caregiver was hypothesized to be positively associated with active leisure activity participation in middle-aged and older adults with DS.
Method
Participants
Participants in the present study were drawn from a larger study conducted between 2010 and 2016 in two locations—University of Wisconsin-Madison and University of Pittsburgh Medical Center. The larger study included 83 middle-aged and older adults with DS and was focused on understanding functional and neurological changes associated with aging. An approximately equal number of participants participated at each site. Participants were recruited through fliers and postings on DS listservs and clinics. Eligibility criteria for the larger study included being over the age of 30 years, having DS confirmed by genetic testing, and having a mental age greater than 30 months. Additionally, participants were assessed for symptoms of dementia and needed to score in the asymptomatic range (<3 cognitive cutoff score) on the Dementia Scale for Down Syndrome (DSDS; Gedye, 1995).
The leisure activity questionnaire, which is the focus of the present study, was added to the study protocol in 2012. Thus, the present analyses are based on the subset of 62 participants (M = 37.82, SD = 7.46) who completed this measure (52 participants completed at first study visit, 10 participants completed at second study visit). The current study is cross-sectional and based on initial leisure activity ratings. Table 1 displays the sociodemographic information for the 62 participants and their caregivers. On average, participants had a mental age of 5.35 years, about half were male, and the majority lived with family. Caregivers of the participants, who completed measures, were primarily parents. All caregivers were a primary caregiver, defined as one of the main caregivers of the participant, and were knowledgeable about their daily activities.
Table 1.
Characteristics of Adults With Down Syndrome and Their Primary Caregivers
| Adult With DS | |
| Age in years (M [SD]) | 37.82 (7.46) |
| Range | 30.00–53.00 |
| Mental age in years (M [SD]) | 5.35 (1.36) |
| Range | 2–8 |
| Physical health (M [SD]) | 1.72 (1.11) |
| Range | 0–4 |
| Gender (n [%]) | |
| Female | 26 (41.9) |
| Male | 36 (58.1) |
| Ethnicity (n [%]) | |
| White, non-Hispanic | 62 (100.0) |
| Other | 0 (0.0) |
| Residence (n [%]) | |
| With Family | 42 (67.7) |
| Group Home | 7 (11.3) |
| Independent w/Support | 13 (21.0) |
| Primary Caregiver | |
| Age in years (M [SD]) | 62.98 (11.50) |
| Range | 22.00–85.00 |
| Ethnicity (n [%]) | |
| White, non-Hispanic | 61 (98.1) |
| Other | 1 (1.9) |
| Relationship (n [%]) | |
| Parent | 55 (88.7) |
| Sibling | 2 (3.2) |
| Other caregiver | 5 (8.1) |
| Time spent with adult with DS (n [%]) | |
| Once a month | 1 (1.6) |
| 2–3 times a month | 3 (4.8) |
| 4 times (weekly) | 2 (3.2) |
| 5–8 times (biweekly) | 11 (17.7) |
| Daily (or almost daily) | 43 (69.4) |
| Missing | 2 (3.2) |
Note. DS = Down syndrome. Physical health is the number of chronic physical health conditions (e.g., heart problems and diabetes) experienced by the middle-aged or older adult with DS.
Analyses were conducted to determine if the subset of 62 participants included in present analyses differed from the larger sample (n = 83). Independent samples t-tests indicated that the 62 participants included in the present analyses did not significantly differ from the larger sample on chronological or mental age. Chi-square tests of independence indicated that the 62 participants included in the present analyses did not significantly differ from the larger sample on residence (i.e., family vs. elsewhere) or type of caregiver (i.e., parent vs. other). The 62 participants included in the present analyses were more likely to be White, non-Hispanic (100% white, non-Hispanic) than those in the larger sample (χ2 [1, 87] = 4.88, p = .03); thus, findings from the present study can only generalize to White, non-Hispanic middle-aged and older adults with DS.
Procedure
The primary caregiver independently completed measures on sociodemographics, the leisure activities of the participant, and their level of caregiver involvement.
Measures
Sociodemographics
Sociodemographics were included in present analyses in order to examine and then control for their impact on leisure activity outcomes when addressing the second study aim. Caregivers reported the chronological age (coded in years) of the participant. The Stanford-Binet, Fifth Edition Abbreviated Battery (SB5; Roid, 2003) was used to obtain an estimate of mental age (in years) of the participant. The SB5 Abbreviated Battery has adequate validity in adults with DS (Couzens, Cuskelly, & Haynes, 2011). Caregivers also completed a checklist of 12 possible physical health problems experienced by the participants (e.g., heart problems, diabetes, and osteoporosis), rated as “present” vs. “absent.” The total number of physical problems rated as “present” was included in analyses. The Reiss Screen for Maladaptive Behavior (RSMB; Reiss, 1994) was completed by caregivers to assess the severity of the co-occurring emotional and behavior problems of the participant. The 26-item Reiss Total Score, which has been shown to have strong reliability and criterion and concurrent validity (Havercamp & Reiss, 1997), was used in analyses. The internal reliability of the 26-item Reiss Total Score in the present sample was adequate (Cronbach’s α =.84).
Caregiver involvement
Caregivers reported on the residence of the participant, which was effect coded as residing with family (1) versus residing elsewhere (−1). Positive coefficients in regression models thus indicate that higher levels of the dependent measure are associated with living with family, whereas negative coefficients indicate that higher levels of the dependent measure are associated with living elsewhere. Caregivers also reported on the amount of time they spent with the participant in the past month, coded as less than weekly (0), weekly (1), or daily (2).
Leisure activity
Caregivers completed the Victoria Longitudinal Study activity questionnaire (VLS; Jopp & Hertzog, 2007). For each item, caregivers rated the frequency (over a 1-year period) that the participant participated in the activity using a 9-point scale: never (0), less than once a year (1), about once a year (2), 2 or 3 times a year (3), about once a month (4), 2 or 3 times a month (5), about once a week (6), 2 or 3 times a week (7), and daily (8). The VLS consists of 10 subscales: physical activities, crafts, games, television watching, social activities, relational activities, travel, technology use, developmental activities, and experiential activities. As shown in Table 2, these subscales were placed in the following domains: physical (physical subscale), social (social-private, social-public, and religious subscales), mentally stimulating (game, experiential, and developmental subscales), and passive (television subscale). The items in each leisure activity domain are also presented in Table 2. Total domain scores (i.e., physical, social, mentally stimulating, and passive) were summed across the items (each rated on the 9-point scale) in the domains, and were used in analyses. In the general population, the VLS was found to have adequate internal consistency and test-retest reliability (Jopp & Hertzog, 2010). In the present sample, the internal consistencies of the domains were as follows: physical (α = .69), social (α = .73), mentally stimulating (α = .82), and passive (α = 64). Conceptually, the VLS is expected to have modest internal consistency, in that an individual who engages in one leisure activity (e.g., eat at a restaurant) may not necessarily engage in other activities in that domain (e.g., attend a church service).
Table 2.
Percentage of Middle-Aged and Older Adults With Down Syndrome Participating in Leisure Activities by Frequency
| Leisure Activity Items | Daily | 2–3 Times a Week | Once a Week | Monthly | Yearly | Never |
|---|---|---|---|---|---|---|
| Physical | ||||||
| Weight lift | 0.0 | 8.1 | 6.5 | 8.1 | 9.7 | 67.8 |
| Aerobics | 8.1 | 21.0 | 14.5 | 3.2 | 9.7 | 43.6 |
| Flexibility | 1.6 | 17.7 | 8.1 | 6.4 | 8.0 | 58.0 |
| Exercise | 8.1 | 16.1 | 21.0 | 24.2 | 16.2 | 14.5 |
| Recreational sports | 3.2 | 9.7 | 37.1 | 22.6 | 19.3 | 8.1 |
| At Least One Activity | 16.1 | 48.4 | 71.0 | 88.7 | 98.4 | 100.0 |
| Mentally Stimulating | ||||||
| Word games | 6.5 | 8.1 | 11.3 | 16.2 | 17.7 | 40.3 |
| Knowledge games | 17.7 | 4.8 | 8.1 | 19.4 | 16.1 | 33.9 |
| Jigsaw puzzles | 0.0 | 3.2 | 4.8 | 14.5 | 22.6 | 54.8 |
| Crossword puzzles | 1.6 | 3.2 | 4.8 | 3.2 | 6.4 | 80.6 |
| Play card game | 1.6 | 8.1 | 11.3 | 32.3 | 19.3 | 27.4 |
| Read books | 9.7 | 14.5 | 9.7 | 14.5 | 8.0 | 43.5 |
| Attend public lecture | 0.0 | 0.0 | 0.0 | 3.2 | 11.3 | 85.5 |
| Course at university | 0.0 | 1.6 | 0.0 | 0.0 | 0.0 | 98.4 |
| Creative writing | 4.8 | 1.6 | 6.5 | 6.4 | 0.0 | 80.6 |
| Go to library | 1.6 | 3.2 | 12.9 | 21.0 | 22.5 | 38.7 |
| Study foreign language | 0.0 | 1.6 | 0.0 | 1.6 | 0.0 | 96.8 |
| Attend movies | 0.0 | 1.6 | 3.2 | 51.6 | 35.5 | 8.1 |
| Collect something | 3.2 | 3.2 | 6.5 | 27.5 | 12.9 | 46.8 |
| Read for leisure | 27.4 | 9.7 | 11.3 | 9.7 | 1.6 | 40.3 |
| Read newspaper | 25.8 | 12.9 | 9.7 | 13.0 | 0.0 | 38.7 |
| Garden | 1.6 | 4.8 | 4.8 | 12.9 | 14.5 | 61.3 |
| Write Letters | 1.6 | 3.2 | 5.1 | 25.8 | 25.8 | 41.9 |
| Sewing, knitting | 0.0 | 3.2 | 0.0 | 0.0 | 4.8 | 91.9 |
| At Least One Activity | 53.2 | 72.6 | 80.6 | 96.8 | 98.4 | 100.0 |
| Social | ||||||
| Go out with friend | 1.6 | 17.7 | 24.2 | 37.1 | 14.5 | 4.8 |
| Visit with friends/relative | 1.6 | 19.4 | 30.6 | 38.7 | 8.0 | 1.6 |
| Attend parties | 0.0 | 1.6 | 4.8 | 48.4 | 37.1 | 8.1 |
| Talk to friend on phone | 19.4 | 14.5 | 9.7 | 30.6 | 14.6 | 11.3 |
| Eat out at restaurant | 0.0 | 27.4 | 30.6 | 37.1 | 4.8 | 0.0 |
| Engaged in political activity | 3.2 | 3.2 | 3.2 | 9.7 | 12.9 | 71.0 |
| Give public talk | 0.0 | 0.0 | 0.0 | 1.6 | 17.8 | 80.6 |
| Attend club meetings | 0.0 | 1.6 | 1.6 | 30.6 | 6.4 | 59.7 |
| Organized social events | 0.0 | 6.5 | 6.5 | 51.7 | 17.7 | 17.7 |
| Volunteer | 4.8 | 8.1 | 22.6 | 11.3 | 12.9 | 40.3 |
| Attend church service | 0.0 | 6.5 | 48.4 | 22.6 | 14.5 | 8.1 |
| Prayer/meditation | 37.1 | 19.4 | 11.3 | 8.1 | 6.5 | 17.7 |
| At Least One Activity | 50.0 | 83.9 | 91.9 | 100.0 | 100.00 | 100.0 |
| Passive | ||||||
| Watch TV comedy/adventure | 79.0 | 8.1 | 6.5 | 3.2 | 0.0 | 3.2 |
| Watch game show | 37.1 | 11.3 | 4.8 | 16.1 | 6.4 | 24.2 |
| Watch TV documentary | 9.7 | 3.2 | 8.1 | 17.8 | 25.8 | 35.5 |
| Watch news | 37.1 | 19.4 | 9.7 | 14.5 | 6.4 | 12.9 |
| At Least One Activity | 83.9 | 93.5 | 96.8 | 98.4 | 98.4 | 100.0 |
Data Analysis Plan
Analyses were first conducted to examine the normality of the data, including histograms of the residuals and quantile-comparison plots. Multi-collinearity among variables was also assessed. In the case of missing items on the leisure activity questionnaire, mean imputation was used to replace missing values if at least 80% of the values in that domain were completed. Across participants, only 1.2% of the items were mean-imputed.
To address the first study aim, descriptive statistics were used to examine the level of participation in active (i.e., physical, social, mentally stimulating) and passive leisure activities by participants. In order to provide a meaningful marker of a high level of leisure activity participation, we compared the percentage of participants who participated in at least one leisure activity within each domain, at least 2–3 times a week, using chi-square goodness-of-fit tests. To address the second study aim, simultaneous multiple linear regression models were conducted in which the leisure activity domain total scores (i.e., physical, social, mentally stimulating, and passive) were the dependent variables and caregiver involvement variables (i.e., residence and time spent with primary caregiver) were the independent variables. Sociodemographics were also included in models to allow us to estimate the association between caregiver involvement and leisure activity participation when holding sociodemographics constant. Independent variables were entered simultaneously given the lack of theoretical justification for an ordered entry of variables.
Results
Distributions of the variables and histograms of the residuals revealed that continuous variables had data with normal distribution and without skew, with the exception of severity of co-occurring emotional and behavior problems, which was positively skewed. This variable was log transformed prior to conducting analyses.
Leisure Activity
The frequency of participation in each specific leisure activity item, by domain, is displayed in Table 2. The most frequently endorsed leisure activity was a passive leisure activity—watching television (83.9% of participants watched television on a daily basis), with comedy or adventure programs being the most common. Of the physical leisure activities, aerobics, exercise, and recreational sports were the most frequent, albeit, less than one-third of participants engaged in any one of these activities at least 2–3 times a week. A marked percentage of participants had never participated in aerobics (43.6%) or exercise (14.5%) in the last year. Of the social leisure activities, seeing friends (i.e., going out with friend, visit friend), talking with friends on the phone, eating at restaurants, and religious activities (i.e., attending church and engaging in prayer) were the most frequent, with more than 83.9% of participants participating in at least one social leisure activity at least 2–3 times a week. Finally, of the mentally stimulating leisure activities, reading (i.e., reading for leisure, reading newspapers, and books), word games, knowledge games, and playing card games were the most frequent.
Figure 1 presents the percentage of participants who engaged in at least one activity in each leisure domain at least 2–3 times a week. A chi-square goodness-of-fit test indicated a significant difference across the four domains in the percentage of participants who engaged in at least one activity at least 2–3 times a week (χ2 [3] = 9.44, p = .02). Follow-up chi-square tests indicated that participants were more likely to participate in at least one passive leisure activity at least 2–3 times a week than at least one physical leisure activity (χ2 [1] = 8.91, p < .01). Participants were also more likely to participate in at least one social leisure activity at least 2–3 times a week than at least one physical leisure activity (χ2 [1] = 5.90, p = .02). There was not a significant difference in likelihood of participating in at least one social leisure activity at least 2–3 times a week versus at least one passive leisure activity (χ2 [1]= 0.33, p = .57). There was also not a significant difference in likelihood of participating in at least one social leisure activity at least 2–3 times a week versus at least one mentally stimulating leisure activity (χ2 [1] = 0.51, p = .48). There was a trend-level difference in likelihood of participating in at least one mentally stimulating leisure activity at least 2–3 times a week versus at least one physical leisure activity (χ2 [1] = 3.00, p = .08); specifically, more participants participated in at least one mentally stimulating leisure activity at least 2–3 times a week than at least one physical leisure activity.
Figure 1.
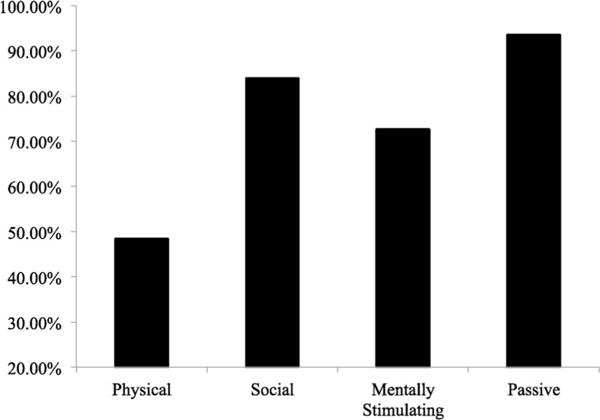
Percentage of middle-aged and older adults with Down syndrome participating in at least one activity at least 2–3 times a week in each leisure activity domain.
Caregiver Involvement and Leisure Activity
Table 3 presents the multiple linear regression models examining the association between caregiver involvement and each domain of leisure activity, while controlling for sociodemographics (i.e., chronological age, mental age, physical health, and co-occurring emotional and behavior problems). The regression model predicting physical leisure activity was significant (F [6,54] = 2.23, R2 = .11, p = .05), and explained 11.0% of the variance. In this model, time spent with primary caregiver (β = .49, p = .02) was significantly associated with physical leisure activity. In addition, participants who lived with family participated in significantly less physical leisure activity than those who lived elsewhere (β = −.47, p = .02). The regression model for social leisure activity was also significant (F [6,54] = 2.57, R2 = .14, p =.03), and explained 13.6% of the variance. In this model, mental age (β = .28, p = .04) was significantly associated with social leisure activity. The regression model for mentally stimulating leisure activity was significant (F [6,54] = 2.34, R2 = .12, p =.04) as well, and explained 11.8% of the variance. In this model, mental age was significantly positively associated with mentally stimulating leisure activity (β = .34, p = .02). Finally, the regression model for passive leisure activity was not significant (F [6,54] = 1.81 R2 = .08, p = .11); however, within the model, chronological age was significantly positively associated with passive leisure activity (β =.32, p = .02).
Table 3.
Multiple Linear Regression Models for Physical, Social, Mentally Stimulating, and Passive Leisure
| Physical
|
Social
|
Mentally Stimulating
|
Passive
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | p | B | SE B | β | p | B | SE B | β | p | B | SE B | β | p | |
| Constant | 12.59 | 10.90 | .25 | 22.29 | 14.86 | .14 | −4.38 | 25.93 | .87 | 1.79 | 9.14 | .85 | ||||
| Mental Age | 0.38 | 0.89 | 0.06 | .67 | 2.52 | 1.21 | 0.28 | .04* | 5.28 | 2.11 | 0.34 | .02* | 1.42 | 0.74 | 0.26 | .06 |
| Chronological Age | −0.14 | 0.16 | −0.12 | .38 | 0.01 | 0.22 | 0.01 | .97 | 0.05 | 0.38 | 0.02 | .90 | 0.31 | 0.13 | 0.32 | .02* |
| Physical Health | 0.55 | 1.05 | 0.07 | .61 | 2.18 | 1.43 | 0.19 | .13 | 4.29 | 2.50 | 0.22 | .09 | 0.19 | 0.88 | 0.03 | .83 |
| Co-EBP | −5.54 | 2.86 | −0.26 | .06 | −7.22 | 3.90 | −0.24 | .07 | −7.25 | 6.80 | −0.14 | .29 | −4.00 | 2.40 | −0.23 | .10 |
| Residence | −4.46 | 1.92 | −0.47 | .02* | −3.64 | 2.62 | −0.28 | .17 | −2.68 | 4.57 | −0.12 | .56 | −1.43 | 1.61 | −0.19 | .38 |
| Time with caregiver | 6.87 | 2.93 | 0.49 | .02* | 6.35 | 4.00 | 0.33 | .12 | 6.74 | 6.98 | 0.20 | .34 | 1.30 | 2.46 | 0.11 | .60 |
| R2 | .11 | .14 | .12 | .08 | ||||||||||||
| F (p-value) | 2.23 (0.05*) | 2.57 (0.03*) | 2.34 (0.04*) | 1.81 (.11) | ||||||||||||
Note. Physical health is the number of chronic physical health conditions (e.g., heart problems and diabetes) experienced by the middle-aged or older adult with DS. Co-EBP = co-occurring emotional and behavior problems. Time with caregiver = time spent with primary caregiver. In follow-up analyses, these models were re-run including middle-aged= and older adults with DS with family caregivers only (i.e., those with non-family caregivers were removed); the same pattern of significant associations was found.
p ≤.05.
Discussion
There is substantial evidence from research on both the general population (Brajša-Žganec et al., 2011, Pressman et al., 2009) and on adolescents and young adults with DS and other types of IDD that leisure activity promotes psychological well-being (e.g., Badia et al., 2011; García-Villamisar & Dattilo, 2010). Little is known about the leisure activity of middle-aged and older adults with DS. Yet, this information is critical for understanding if this population is at risk for low active leisure activity participation and, if so, which domains of leisure activity are underutilized.
We found that middle-aged and older adults with DS most frequently participate in passive, as opposed to active, leisure activity. Indeed, the large majority watched television daily, which was markedly higher than the daily level of participation in active leisure activities. In terms of the active leisure activity of middle and older adults with DS, social leisure activities were the most common, with interacting with friends, eating at restaurants, and religious activities being most frequent. Thus, as with younger adults with DS and other IDDs (e.g., Badia et al., 2011; Dusseljee, et al., 2011), social leisure activities are relatively common in middle-aged and older adults with DS. However, there are still a marked number of social leisure activities being underutilized by middle-aged and older adults with DS. For example, less than 14% of middle-aged and older adults with DS attended an organized social event, a party, or a club meeting in the past month.
Participation in physical and mentally stimulating leisure activity by middle-aged and older adults with DS was lower than participation in social leisure activity. In terms of physical leisure activity, less than half of the middle-aged and older adults with DS in our sample participated in at least one physical leisure activity at least 2–3 times per week, and a marked portion never participated in aerobics or flexibility exercises in the past year. In part, age-related medical conditions and declines in functioning that begin in middle adulthood in individuals with DS may make it difficult to engage in physical activities. However, number of physical health conditions and chronological age were not significantly associated with physical leisure activity participation in the present sample. Thus, mechanisms other than physical health appear to play a large role in the extent to which middle-aged and older adults with DS participate in physical leisure activity. In terms of mentally stimulating leisure activity, the majority of middle-aged and older adults with DS participated in at least one mentally stimulating activity at least 2–3 times per week; however, only half of the middle-aged and older adults with DS participated in at least one mentally stimulating leisure activity daily.
Overall, findings from the present study have several potential implications for supporting optimal psychological well-being in this population, which should be explored in future research. Although the high level of passive leisure (television watching) by middle-aged and older adults with DS may not greatly differ from the general population (Nielsen Report, 2016), when combined with low levels of active leisure activity, there could be negative consequences on psychological well-being. Indeed, high levels of passive leisure activity has been shown to negatively impact psychological well-being (e.g., negative affect, fatigue, and low self-esteem) in studies on the general population (e.g., Kikuchi et al., 2014; Trainor et al., 2010); thus, efforts to decrease passive leisure activity may result in more optimal psychological well-being in a DS population as well. Our findings also suggest a need for support services that promote physical leisure activity in middle-aged and older adults with DS, given that the majority of middle-aged and older adults with DS do not meet the World Health Organization recommended levels of aerobic (150 minutes spread across multiple days per week) and muscle-strengthening activities (2 days per week). Physical leisure activity has strong associations with healthy aging, specifically, by reducing or delaying the onset of medical problems and maintaining optimal physical functioning (Lee et al., 2012).
Mentally stimulating leisure appears to be relatively limited in middle-aged and older adults with DS; efforts to increase these activities may increase psychological well-being and could potentially help delay onset of dementia, as has been found in the general population (Wilson et al., 2002). There may be low-cost ways to foster regular participation in mentally stimulating activities appropriate for middle-aged and older adults with DS who have a wide range of cognitive ability levels. For example, designated times for games (e.g., crossword puzzles, mazes, and card games), reading, and writing (e.g., diaries and letters) may encourage participation in fun ways. Many mentally stimulating leisure activities require literacy skills; thus, postsecondary literacy programs, which have been shown to be efficacious in adults with DS (Moni, Jobling, Morgan & Lloyd, 2011), may also be important. Finally, many of the most commonly engaged in physical and mentally stimulating leisure activities were home-based, as opposed to community-based. Thus, support services should consider focusing on community-based leisure activities, given their added benefit of fostering social connections and feelings of community belonging.
In the present study, caregiver involvement had important associations with the physical leisure activity of middle-aged and older adults with DS. However, in contrast to our hypothesis, middle-aged and older adults with DS who co-resided with family participated in lower levels of physical leisure activity than those who lived in group homes or independent living situations. It may be that middle-aged and older adults with DS living with family are at risk for lower physical leisure activity participation because aging family members are less able to facilitate (e.g., organize and provide transportation) and/or be social partners in these activities than agency providers. Moreover, middle-aged and older adults with DS residing in group homes or independent living situations may have more physical leisure activities built into their programs and services (e.g., designated times for exercise and recreational sports) than middle-aged and older adults with DS co-residing with family. In support of our hypothesis, the time the middle-aged or older adult with DS spent with their primary caregiver was positively associated with physical leisure activity. Thus, a greater level of involvement by primary caregivers in the lives of middle-aged and older adults with DS is associated with greater participation in physical leisure activity. This finding is consistent with previous studies on adolescents and young adults with DS and other IDDs (Buttimer & Tierney, 2005; Jobling & Cuskelly, 2002), which have also highlighted the role of caregivers in facilitating and/or being social partners in leisure activities. Efforts to increase the physical leisure activity of middle-aged and older adults with DS may be most successful if they partner with primary caregivers, as these caregivers may have important insights into ways to overcome obstacles to participation.
Neither residence nor time spent with the primary caregiver was significantly related to participation in social or mentally stimulating leisure activity by the middle-aged and older adults with DS in our sample. Given the relatively high level of social leisure activity participation, it is possible that these activities are built into formal support services more so than physical leisure activities and, thus, they are not dependent upon involvement from primary caregivers. In contrast, the relatively low level of mentally stimulating leisure activity suggests that this domain of leisure activity is largely overlooked by both formal support services and the more informal support efforts of primary caregivers. In our sample, there were not sociodemographic differences between the middle-aged and older adults with DS who co-resided with family versus those who lived elsewhere, however, it is possible that other selection effects are contributing to these findings. In other words, middle-aged and older adults with DS who co-reside with family may be different from those who live in group homes or independent living situations in other unexamined ways.
Finally, sociodemographics of the middle-aged and older adults with DS were related to leisure activity in a number of ways. Mental age was positively associated with social and mentally stimulating leisure activity. Middle-aged and older adults with DS with higher cognitive functioning are likely to be able to engage in a greater range of social (e.g., attend club meetings and volunteer) and mentally stimulating (e.g., reading and writing) leisure activities than those with lower cognitive functioning. Thus, it may be important to educate caregivers and middle-aged and older adults with DS on social and mentally stimulating leisure activities that fit the ability of individuals with lower cognitive functioning, such that all individuals have access to social and mentally stimulating leisure activities, regardless of ability level. Finally, the chronological age of the adult with DS was positively associated with participation in passive leisure activity. Thus, efforts to reduce high frequency of passive leisure activity in older adults with DS may help increase the psychological well-being of this group.
The present study is one of the first to examine the leisure activity of middle-aged and older adults with DS across multiple domains and to examine associations with caregiver involvement. However, there are limitations to the present study. Our sample was restricted to middle-aged and older adults with DS with mental age greater than 30 months and with no clinical signs of dementia; thus, findings are only representative of this population. It is likely that the leisure activity of middle-aged and older adults with DS who have dementia symptoms differs from the patterns seen in the present sample. Moreover, the study largely involved family caregivers, specifically parents, as opposed to other types of caregivers (e.g., agency providers). In addition, future studies should assess caregiver characteristics, such as physical and psychological health, as these factors may influence the ability of caregivers to facilitate and engage in leisure activity with the middle-aged or older adult with DS.
The present study is cross-sectional, meaning that cause and effect interpretations about predictor variables and leisure activity cannot be made. However, as our ongoing longitudinal study unfolds, we will have the ability to examine within-person changes in leisure activity in relation to changes in caregiver involvement (e.g., changes in residence and time spent with primary caregivers). We created domains of leisure activity (i.e., physical, social, mentally stimulating, and passive) consistent with those identified in previous studies (Jobling & Cuskelly, 2002; Jopp & Hertzog, 2007); however, the psychometric properties of our leisure activity domains were not examined. Future studies should examine the properties of the VLS, as well as other leisure activity measures in middle-aged and older adult with DS. Finally, we recommend that multiple informants and self-report be incorporated into future studies of the leisure activity of middle-aged and older adults with DS, as any one caregiver may not be fully informed, particularly when caregivers do not co-reside with the middle-aged or older adult with DS. Diary studies documenting the leisure activities of middle-aged or older adults with DS over a short time frame (e.g., 1 week) and detailing each activity would further clarify the settings and social partners of leisure activities, as well as any barriers to increasing leisure activity.
Summary
In summary, our findings suggest that middle-aged and older adults with DS more frequently participate in passive and social leisure activities than in physical and mentally stimulating leisure activities. This information can be used to help direct support services in efforts to increase underutilized domains of active leisure activity. Middle-aged and older adults with DS who lived in group homes or independent living situations reported a higher level of physical leisure activity than those who lived with family, and greater time spent with the primary caregiver was positively associated physical leisure activity. Given the importance of caregiver involvement, programs and supports should partner with caregivers when developing ways to foster active leisure activity opportunities.
Acknowledgments
This study was funded by the National Institute of Aging (AG076640 to B. Handen and B. Christian) and the National Institute on Child Health and Human Development (P30 HD03352 to M. Mailick). We thank our team of collaborators and the families who generously participated in this study.
Contributor Information
Iulia Mihaila, University of Wisconsin – Madison.
Sigan L. Hartley, University of Wisconsin – Madison
Benjamin L. Handen, University of Pittsburgh
Peter D. Bulova, University of Pittsburgh
Rameshwari V. Tumuluru, University of Pittsburgh
Darlynne A. Devenny, New York State Institute for Basic Research in Developmental Disabilities
Sterling C. Johnson, University of Wisconsin – Madison
Patrick J. Lao, University of Wisconsin – Madison
Bradley T. Christian, University of Wisconsin – Madison
References
- Badia M, Orgaz BM, Verdugo MA, Ullán AM, Martínez MM. Personal factors and perceived barriers to participation in leisure activities for young and adults with developmental disabilities. Research in Developmental Disabilities. 2011;32(6):2055–2063. doi: 10.1016/j.ridd.2011.08.007. http://dx.doi.org/10.1016/j.ridd.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Brajša-Žganec A, Merkaš M, Šverko I. Quality of life and leisure activities: How do leisure activities contribute to subjective well-being? Social Indicators Research. 2011;102:81–91. http://dx.doi.org/10.1007/s11205-010-9724-2. [Google Scholar]
- Browder DM, Cooper KJ. Inclusion of older adults with mental retardation in leisure opportunities. Mental Retardation. 1994;32(2):91–99. [PubMed] [Google Scholar]
- Buttimer J, Tierney E. Patterns of leisure participation among adolescents with a mild intellectual disability. Journal of Intellectual Disabilities. 2005;9:25–42. doi: 10.1177/1744629505049728. http://dx.doi.org/10.1177/1744629505049728. [DOI] [PubMed] [Google Scholar]
- Carr J. The everyday life of adults withv Down syndrome. Journal of Applied Research in Intellectual Disabilities. 2008;21:389–397. http://dx.doi.org/10.1111/j.1468-3148.2007.00418.x. [Google Scholar]
- Couzens D, Cuskelly M, Haynes M. Cognitive development and Down syndrome: Age-related change on the Stanford-Binet Test (Fourth edition) American Journal on Intellectual and Developmental Disabilities. 2011;116:181–204. doi: 10.1352/1944-7558-116.3.181. http://dx.doi.org/10.1352/1944-7558-116.3.181. [DOI] [PubMed] [Google Scholar]
- Dusseljee JCE, Rijken PM, Cardol M, Curfs LMG, Groenewegen PP. Participation in daytime activities among people with mild or moderate intellectual disability. Journal of Intellectual Disability Research. 2011;55:4–18. doi: 10.1111/j.1365-2788.2010.01342.x. http://dx.doi.org/10.1111/j.1365-2788.2010.01342.x. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ. Health conditions associated with aging and end of life of adults with Down syndrome. International Review of Research in Mental Retardation. 2010;39(C):107–126. doi: 10.1016/S0074-7750(10)39004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Villamisar DA, Dattilo J. Effects of a leisure programme on quality of life and stress of individuals with ASD. Journal of Intellectual Disability Research. 2010;54:611–619. doi: 10.1111/j.1365-2788.2010.01289.x. http://dx.doi.org/10.1111/j.1365-2788.2010.01289.x. [DOI] [PubMed] [Google Scholar]
- Gedye A. Dementia Scale for Down’s Syndrome: Manual. Vancouver, BC: Gedye Research and Counseling; 1995. [Google Scholar]
- Hall L, Hewson S. The community links of a sample of people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2006;19(2):204–207. http://dx.doi.org/10.1111/j.1468-3148.2005.00249.x. [Google Scholar]
- Hartley SL, Handen BL, Devenny DA, Hardison R, Mihaila I, Price JC, Christian BT. Cognitive functioning in relation to brain amyloid-β in healthy adults with Down syndrome. Brain: A Journal of Neurology. 2014;137:2556–2563. doi: 10.1093/brain/awu173. http://dx.doi.org/10.1093/brain/awu173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havercamp SM, Reiss S. The Reiss Screen for Maladaptive Behavior: Confirmatory factor analysis. Behaviour Research and Therapy. 1997;35(10):967–971. doi: 10.1016/s0005-7967(97)00043-0. http://dx.doi.org/10.1016/S0005-7967(97)00043-0. [DOI] [PubMed] [Google Scholar]
- Hermans H, Evenhuis HM. Multimorbidity in older adults with intellectual disabilities. Research in Developmental Disabilities. 2014;35:776–783. doi: 10.1016/j.ridd.2014.01.022. http://dx.doi.org/10.1016/j.ridd.2014.01.022. [DOI] [PubMed] [Google Scholar]
- Horvath S, Garagnani P, Bacalini MG, Pirazzini C, Salvioli S, Gentilini D, Franceschi C. Accelerated epigenetic aging in Down syndrome. Aging Cell. 2015;14:491–495. doi: 10.1111/acel.12325. http://dx.doi.org/10.1111/acel.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobling A, Cuskelly M. Life styles of adults with Down syndrome living at home. In: Cuskelly M, Jobling A, Buckley S, editors. Down syndrome across the life span. Philadelphia, PA: Whurr Publishers; 2002. pp. 109–120. [Google Scholar]
- Jopp DS, Hertzog C. Activities, self-referent memory beliefs, and cognitive performance: Evidence for direct and mediated relations. Psychology and Aging. 2007;22(4):811–825. doi: 10.1037/0882-7974.22.4.811. http://dx.doi.org/10.1037/0882-7974.22.4.811. [DOI] [PubMed] [Google Scholar]
- Jopp DS, Hertzog C. Assessing adult leisure activities: An extension of a self-report activity questionnaire. Psychological Assessment. 2010;22(1):108–120. doi: 10.1037/a0017662. http://dx.doi.org/10.1037/a0017662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi H, Inoue S, Sugiyama T, Owen N, Oka K, Nakaya T, Shimomitsu T. Distinct associations of different sedentary behaviors with health-related attributes among older adults. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2014;67:335–339. doi: 10.1016/j.ypmed.2014.08.011. http://dx.doi.org/10.1016/j.ypmed.2014.08.011. [DOI] [PubMed] [Google Scholar]
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarkzyk PT. Effect of physical inactivity on major noncommunicable diseases worldwide: An analysis of burden of disease and life expectancy. The Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. http://dx.doi.org/10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire D, Chicoine B. Mental wellness in adults with Down syndrome: A guide to emotional and behavioral strengths and challenges. Bethesda, MD: Woodbine House; 2006. [Google Scholar]
- Menec VH. The relation between everyday activities and successful aging: A 6-year longitudinal study. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2003;58B(2):S74–S82. doi: 10.1093/geronb/58.2.s74. http://dx.doi.org/10.1093/geronb/58.2.S74. [DOI] [PubMed] [Google Scholar]
- Mikkelsen SS, Tolstrup JS, Flachs EM, Mortensen EL, Schnohr P, Flensborg-Madsen T. A cohort study of leisure time physical activity and depression. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2010;51(6):471–475. doi: 10.1016/j.ypmed.2010.09.008. http://dx.doi.org/10.1016/j.ypmed.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Moran J. Aging and Down Syndrome: A health & well-being guidebook. 2013 Retrieved from http://www.ndss.org/PageFiles/2594/Aging%20and%20Down%20Syndrome%20A%20Health%20and%20Well-Being%20Guidebook.pdf.
- Moni KB, Jobling A, Morgan M, Lloyd J. Promoting literacy for adults with intellectual disabilities in a community-based service organization. Australian Journal of Adult Learning. 2011;51:456–478. [Google Scholar]
- Nielson Report. The comparable metrics report: Q1 2016. 2016 Retrieved from: http://www.nielsen.com/us/en/insights/reports/2016/the-comparable-metrics-report-q1-2016.html.
- Patterson D, Cabelof DC. Down syndrome as a model of DNA polymerase beta haploinsufficiency and accelerated aging. Mechanisms of Ageing and Development. 2012;133(4):133–137. doi: 10.1016/j.mad.2011.10.001. http://dx.doi.org/10.1016/j.mad.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, Schulz R. Association of enjoyable leisure activities with psychological and physical well-being. Psychosomatic Medicine. 2009;71:725–732. doi: 10.1097/PSY.0b013e3181ad7978. http://dx.doi.org/10.1097/PSY.0b013e3181ad7978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruchno RA, McMullen WF. Patterns of service utilization by adults with a developmental disability: Type of service makes a difference. American Journal on Mental Retardation. 2004;109(5):362–378. doi: 10.1352/0895-8017(2004)109<362:POSUBA>2.0.CO;2. http://dx.doi.org/10.1352/0895-8017(2004)109<362:POSUBA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Putnam JW, Pueschel SM, Gorder Holman J. Community activities of youths and adults with Down syndrome. British Journal of Mental Subnormality. 1988;34(66):47–53. http://dx.doi.org/10.1179/bjms.1988.006. [Google Scholar]
- Reed J, Ones DS. The effect of acute aerobic exercise on positive activated affect: A meta-analysis. Psychology of Sport and Exercise. 2006;7:477–514. http://dx.doi.org/10.1016/j.psychsport.2005.11.003. [Google Scholar]
- Reiss S. Reiss Screen for Maladaptive Behavior. Worthington, OH: International Diagnostic Systems; 1994. [Google Scholar]
- Roid GH. Stanford-Binet Intelligence Scales. 5th. Itasca, IL: Riverside; 2003. [Google Scholar]
- Torr J, Strydom A, Patti P, Jokinen N. Aging in Down syndrome: Morbidity and mortality. Journal of Policy and Practice in Intellectual Disabilities. 2010;7:70–81. http://dx.doi.org/10.1111/j.1741-1130.2010.00249.x. [Google Scholar]
- Trainor S, Delfabbro P, Anderson S, Wine-field A. Leisure activities and adolescent psychological well-being. Journal of Adolescence. 2010;33:173–186. doi: 10.1016/j.adolescence.2009.03.013. http://dx.doi.org/10.1016/j.adolescence.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Barnes LLJA, Schneider Bienais JL, Evans DA, Bennett DA. Participation in cognitively stimulating activities and risk of incident Alzheimer disease. The Journal of the American Medical Association. 2002;287:742–748. doi: 10.1001/jama.287.6.742. http://dx.doi.org/10.1001/jama.287.6.74. [DOI] [PubMed] [Google Scholar]
- Zigman WB, Lott IT. Alzheimer’s disease in Down syndrome: Neurobiology and risk. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:237–246. doi: 10.1002/mrdd.20163. http://dx.doi.org/10.1002/mrdd.20163. [DOI] [PubMed] [Google Scholar]


