Figure 1.
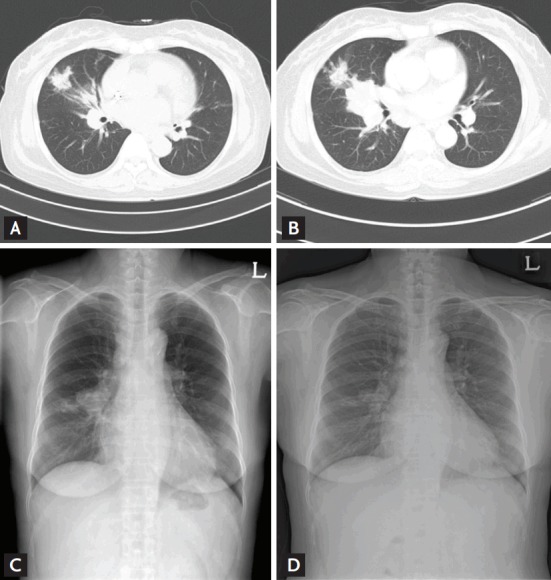
Images obtained from a 60-year-old female with tuberculosis mimicking invasive aspergillosis. She had received a kidney transplant 4 months prior. (A, B) conventional computed tomography (CT) lung images (5-mm-thick) obtained at the level of the right middle lobe (RML). (A) Image reveals macronodular consolidation along the bronchovascular bundle of the RML, and bronchial wall thickening. The bronchoalveolar lavage fluid was strongly positive for galactomannan and the initial diagnosis was of probable invasive pulmonary aspergillosis. (B) After 4 months of voriconazole treatment, follow-up chest CT showed that the irregularly shaped mass had increased in size and exhibited a tree-inbud appearance. Percutaneous core lung and supraclavicular lymph node biopsies revealed chronic granulomatous inf lammation with caseous necrosis. A member of the Mycobacterium tuberculosis complex was cultured from sputum and aspirated lung tissue. The patient received empirical anti-tuberculous therapy. Follow-up chest radiographs showed that the RML lung nodules had decreased in size (C: before anti-tuberculous therapy; D: after 8 weeks of anti-tuberculous therapy).
