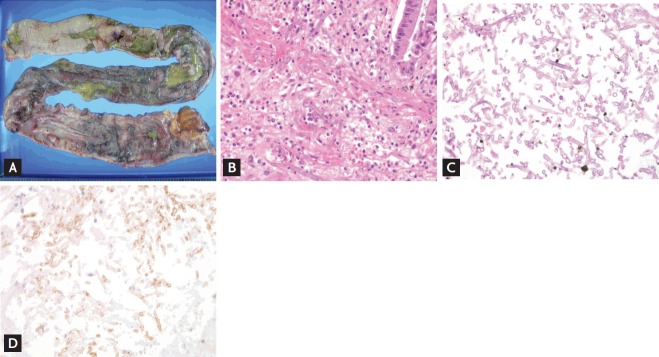
Figure 2.
A 62-year-old female underwent total colectomy because of sigmoid colon perforation and panperitonitis developing on day 10 after kidney transplantation. (A) The resected large intestine, a segment of the terminal ileum, the small intestine, and pericolic adipose tissue. Multiple ulcerative lesions (in a 6.2 × 5.4 × 0.2 cm region) are evident in the mucosal area. (B) The fungal morphology, as revealed by H&E (×400), was suggestive of mucormycosis. Mucormycetes invade tissues and cause vascular embolization. After surgery, despite the prescription of amphoterecin B, the infection was not controlled and a second-look operation involving total gastrectomy, splenectomy, graftectomy, and ileal repair was performed. Fungal balls were evident in the stomach and ileal walls. (C) Fungal hyphae associated with mycotic thromboemboli were evident in the stomach, liver, spleen, and peripancreatic tissue. The fungal hyphae were thin, evenly distributed, septated, and branched at an acute angle, suggestive of aspergillosis rather than mucormycosis (periodic acid-Schiff staining, ×400). (D) Mucormycosis immunohistochemistry (IHC) staining (×400) was positive and aspergillosis IHC was negative.