Abstract
Background
Many physicians believe that advanced practice clinicians (APCs [nurse practitioners and physician assistants]) provide care of relatively lower value.
Objective
To compare use of low-value services among U.S. APCs and physicians.
Design
Service use after primary care visits was evaluated for 3 conditions after adjustment for patient and provider characteristics and year. Patients with guideline-based red flags were excluded and analyses stratified by office-versus hospital-based visits, acute versus nonacute presentations, and whether clinicians self-identified as the patient’s primary care provider (PCP).
Setting
National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS), 1997 to 2011.
Patients
Patients presenting with upper respiratory infections (URIs), back pain, or headache.
Measurements
Use of guideline-discordant antibiotics (for URIs), radiography (for URIs and back pain), computed tomography (CT) or magnetic resonance imaging (MRI) (for headache and back pain), and referrals to other physicians (for all 3 conditions).
Results
12 170 physician and 473 APC office-based visits and 13 359 physician and 2947 APC hospital-based visits were identified. Although office-based clinicians saw similar patients, hospital-based APCs saw younger patients (mean age, 42.6 vs. 45.0 years; P < 0.001), and practiced in urban settings less frequently (49.7% vs. 81.7% of visits; P < 0.001) than hospital-based physicians. Unadjusted and adjusted results revealed that APCs ordered antibiotics, CT or MRI, radiography, and referrals as often as physicians in both settings. Stratification suggested that self-identified PCP APCs ordered more services than PCP physicians in the hospital-based setting.
Limitation
NHAMCS reflects hospital-based APC care; NAMCS samples physician practices and likely underrepresents office-based APCs.
Conclusion
APCs and physicians provided an equivalent amount of low-value health services, dispelling physicians’ perceptions that APCs provide lower-value care than physicians for these common conditions.
Primary Funding Source
U.S. Health Services and Research Administration, Ryoichi Sasakawa Fellowship Fund, and National Institutes of Health.
The U.S. health care system faces a looming shortage of primary care providers (PCPs) (1, 2), and estimates suggest that it might reach up to 20 000 physicians by 2020 (3). The causes of the projected shortage include both demand- and supply-related factors, such as an increased demand for primary care services from the millions of newly insured patients after passage of the Patient Protection and Affordable Care Act, as well as fewer trainees electing to enter primary care (2, 4–7).
In response to these trends, many have advocated for expanding the role of advanced practice clinicians (APCs [nurse practitioners and physician assistants]) in primary care as a potential policy solution to mitigate the workforce shortage (1, 8–10). These practitioners represent the fastest-growing segment of the primary care workforce, and they are more likely to serve minority and underserved patients (1). Studies suggest that APCs may be a cost-saving alternative to physicians in primary care, even after adjustment for case complexity and productivity, mainly because of their lower salaries (10–13). Although previous research and systematic reviews suggest that APCs provide care of the same quality as that of physicians (14–17), little is known about their effect on providing wasteful or low-value health services. According to a recent national survey, most physicians believe that APCs provide lower-quality care than they do, and nearly one quarter think that expanding nurse practitioners’ roles in U.S. practice would decrease the efficiency and value of health care (18).
Despite these perceptions, no previous research compared APCs and physicians directly with regard to ordering potentially guideline-discordant and low-value health services, which has important implications for the quality and efficiency of care delivery in the U.S. health care system. For example, an estimated 30% of U.S. health care spending is wasteful (19), and much of this waste is driven by use of low-value health services, which is defined as patient care that typically portends a greater probability of harm than benefit (20–22). In this context, we used national data on ambulatory visits to providers to compare the use of potentially low-value health services between APCs and physicians in the management of common conditions in the primary care setting.
Methods
Data Sources
We used data from the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) on ambulatory visits to clinicians from 1 January 1997 through 31 December 2011. The NAMCS comprises probability samples of outpatient visits to nonfederal, office-based physician practices, whereas the NHAMCS contains data on visits to nonfederal, hospital-based outpatient departments, including outpatient clinics and emergency departments. Developed in parallel, the NAMCS and NHAMCS have common designs, variables, and visit weights. They both are structured to represent ambulatory visits to physicians across the United States, but they also contain data on visits to APCs (23, 24). Importantly, the NAMCS samples physician practices, some of which include APCs, but does not include independently practicing APCs. The NHAMCS samples hospital-based outpatient departments, which more commonly include APCs, including those who practice independently. Thus, APCs in our sample are represented predominantly by the NHAMCS data. Further details on the NAMCS and NHAMCS are available in the Methods section in the Appendix (including Appendix Figures 1 and 2, available at www.annals.org) and from the National Center for Health Statistics (23).
Data Collection Procedures
The data are collected by a standardized survey form, which the provider or other staff completes soon after each ambulatory visit. The NAMCS and NHAMCS both collect information on the patient’s primary reason for the visit (for example, the chief symptom); 2 other nonprimary reasons for the visit; up to 3 diagnoses, derived from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM); the payer for the visit (for example, commercial or Medicare insurance); whether the provider self-identified as the patient’s PCP; patient and provider demographic information; tests and treatments ordered; and medications listed during the visit.
Study Sample
We selected outpatient visits (excluding those to the emergency department) for 3 common conditions seen in the primary care setting (for example, general medicine, family medicine, or internal medicine physician offices or outpatient hospital departments; see the Methods section in the Appendix for more details) that frequently are associated with use of low-value services, namely upper respiratory infections (URIs [such as acute bronchitis and pharyngitis]), back pain, and headache.
For all chief symptoms, the NAMCS and NHAMCS provide information on the reasons for patient visits, divided into 5 categories: new-onset symptoms (<3 months duration), acute-on-chronic flare-up, chronic routine visit, routine or preventive care, and pre- or postoperative visit. We defined acute visits by combining the categories new-onset symptoms and acute-on-chronic flare-up.
APCs
Both the NAMCS and NHAMCS identify the clinician who provided care during the visit as a physician, a nurse practitioner, a physician assistant, a nurse midwife, a registered or licensed practical nurse, or another provider. For this study, we excluded registered and licensed practical nurses, other providers, and midwives (see the Appendix for details on excluding midwives), because they typically do not have the authority to order such services as antibiotic treatment, imaging, and referrals. For our primary analysis, we classified nurse practitioners and physician assistants as APCs. As a secondary analysis, we also evaluated results by APC visit subtype (for example, APCs seeing the patient alone vs. alongside the physician) and profession subtype (for example, nurse practitioner vs. physician assistant) and compared them with results from physicians seeing patients without an APC, who made up the reference group (Appendix). Although training of nurse practitioners and physician assistants, as well as the regulatory environment in which they practice, differs between these groups and among the states in which they practice, we chose a combined APC variable, because both types of clinicians often play similar roles in the primary care setting (25) and because it made interpretation easier. In addition, the findings of the subgroup categories described earlier largely were consistent with our overall results.
Outcome Measures
We studied 3 types of outcomes widely considered to be low-value services in most cases, as identified in previous studies or guidelines—use of antibiotics (for URIs); plain radiography (for URIs and back pain); and advanced imaging, including both magnetic resonance imaging (MRI) and computed tomography (CT) (for back pain and headache)—as well as 1 overall outcome that applied to all 3 conditions. Our cohort excluded visits from patients with red flags (for example, symptoms or diagnoses of neurologic deficit in those with back pain or headache, concomitant chronic obstructive pulmonary disease, or HIV in those with acute bronchitis) and was derived from previous research by our group and others using NAMCS and NHAMCS data (20, 21, 26, 27), which were based on relevant clinical and regulatory agency guidelines during the study period (28–32). In addition, we evaluated referrals to other physicians (for all 3 conditions), which generally are not required for these illnesses and might indicate more unnecessary downstream utilization.
Potential Confounders
From the data recorded for each visit, we assessed for patient age (measured as a continuous variable), sex, race or ethnicity, modified Charlson comorbidity count (33), symptom acuity, insurance status, urban location, geographic region, and year. The clinicians who completed the survey defined race and ethnicity as 2 separate variables; we reclassified patients to a single 4-level race or ethnicity variable (white, black, Hispanic, and other).
We also considered whether the clinician self-identified as the patient’s PCP, which we determined as follows: From 1997 through 2004, the NAMCS and NHAMCS asked, “Are you the patient’s primary care physician?” From 2005 through 2011, the NAMCS changed the question to “Are you the patient’s primary care physician/provider?” During 2005 and 2006, the NHAMCS asked, “Are you the patient’s primary care physician/provider?” Finally, in 2007 to 2011, the NHAMCS changed the question to “Is this clinic the patient’s primary care provider?”
For the NAMCS analyses, we also identified practice setting types, which we combined into 3 main categories: private solo or group continuity practices; noncontinuity, freestanding clinics or urgent care centers; and other continuity-type clinics (such as federally qualified health centers, community health centers, and nonfederal government clinics).
Statistical Analysis
We pooled all years and conducted separate analyses for our NAMCS and NHAMCS samples because they each use distinct sampling approaches with regard to APC practice, as explained earlier. All analyses were weighted and accounted for the complex sampling. We used chi-square tests and unadjusted linear regression to compare visit characteristics among APCs and physicians, respectively. For our unadjusted analysis, we pooled all years within each outcome category and used unadjusted logistic regression models for each outcome, focusing on APC provider as the exposure of interest. For adjusted analyses, we estimated similar models but included the aforementioned demographic, clinical, and provider variables to control for potential confounders. We also controlled for year.
To evaluate important potential effect modification based on symptom acuity and whether the clinician self-identified as the PCP, we also stratified our results by symptom acuity and PCP status. Because of the wording change associated with the PCP variable, as noted earlier, we conducted sensitivity analyses to ensure that stratified results were similar when we compared data after 2005 with our main findings (see the Appendix for details). Finally, we also evaluated practice settings in which APCs predominantly practiced independently versus those in which physicians practiced alone (Appendix).
We performed all our analyses with SAS-Callable SUDAAN, version 11.0 (RTI International), using SUDAAN subpopulation procedures. These functions use information from the entire NAMCS and NHAMCS sample to account for the complex study design and sampling weights to produce national estimates (24).
The Harvard Medical School Committee on Human Studies determined that this study was exempt from review.
Role of the Funding Source
The funders had no role or influence in the design and conduct of the study; collection, management, analysis, and interpretation of the data; decision to publish; or preparation, review, or approval of the manuscript.
Results
We identified 28 949 U.S. primary care visits for the 3 conditions, including 25 529 physician and 3420 APC visits, representing an estimated 681 million total visits from 1997 to 2011. Of these, 89.9% reflected visits to clinicians in office-based physician practices (data from the NAMCS) and 10.1% to those practicing in hospital-based outpatient clinics (data from the NHAMCS). Table 1 presents relevant patient and visit characteristics by clinician subtype, and Appendix Tables 1 and 2 (available at www.annals.org) present these characteristics by additional APC subgroupings. Although office-based APCs and physicians saw largely similar patients, hospital-based APCs treated younger patients (mean age, 42.6 vs. 45.0 years; P < 0.001) and delivered care in an urban setting less frequently (49.7% vs. 81.7% of visits; P < 0.001) than hospital-based physicians.
Table 1.
Patient Demographic Characteristics, by Clinician Type*
| Characteristic | Office-Based | Hospital-Based | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Physicians | APCs | P Value | Physicians | APCs | P Value | |
| Sample/weighted population, n/N | 12 170/586 million | 473/25.8 million | 13 359/54.2 million | 2947/14.6 million | ||
|
| ||||||
| Mean age, y | 48.9 | 47.9 | 0.34 | 45.0 | 42.6 | <0.001 |
|
| ||||||
| Female | 62.7 | 63.6 | 0.78 | 64.6 | 66.3 | 0.27 |
|
| ||||||
| Race/ethnicity | 0.067 | <0.001 | ||||
| White | 76.9 | 77.2 | 70.6 | 79.6 | ||
|
| ||||||
| Black | 10.3 | 10.8 | 16.7 | 9.2 | ||
|
| ||||||
| Hispanic | 8.3 | 10.0 | 9.7 | 7.5 | ||
|
| ||||||
| Other | 4.6 | 1.9 | 3.0 | 3.6 | ||
|
| ||||||
| Mean Charlson comorbidity count | 0.047 | 0.044 | 0.77 | 0.049 | 0.022 | <0.001 |
|
| ||||||
| Acute symptoms | 72.7 | 77.5 | 0.096 | 75.0 | 88.0 | <0.001 |
|
| ||||||
| Insurance | 0.077 | 0.050 | ||||
| Private | 57.6 | 65.1 | 46.0 | 42.0 | ||
|
| ||||||
| Medicare/Medicaid | 26.7 | 21.0 | 33.4 | 32.7 | ||
|
| ||||||
| Other | 15.8 | 13.9 | 20.6 | 25.3 | ||
|
| ||||||
| Provider identifies as PCP | 79.9 | 71.0 | 0.21 | 52.8 | 52.5 | 0.96 |
|
| ||||||
| Urban location | 82.1 | 78.9 | 0.46 | 81.7 | 49.7 | <0.001 |
| Region | 0.040 | 0.31 | ||||
|
| ||||||
| Northeast | 19.1 | 17.1 | 17.6 | 17.5 | ||
|
| ||||||
| Midwest | 24.2 | 23.6 | 37.2 | 25.5 | ||
|
| ||||||
| South | 35.5 | 47.6 | 30.8 | 40.2 | ||
|
| ||||||
| West | 21.2 | 11.7 | 14.4 | 16.8 | ||
| Symptom group | ||||||
|
| ||||||
| URIs | 35.6 | 44.1 | 0.015 | 37.1 | 42.0 | 0.016 |
|
| ||||||
| Back pain | 47.4 | 39.9 | 0.011 | 46.0 | 41.5 | 0.029 |
|
| ||||||
| Headache | 18.2 | 17.8 | 0.85 | 18.1 | 18.1 | 0.99 |
APC = advanced practice clinician; PCP = primary care provider; URI = upper respiratory infection.
Values are percentages unless otherwise indicated and may not sum to 100 due to rounding. Boldface values indicate comparisons with P < 0.05.
Unadjusted Frequencies of Use
In the unadjusted analyses (Table 2), APCs were not significantly more likely to order antibiotics, CT or MRI, or radiography, or to refer patients to other physicians, than physicians in office- or hospital-based settings, although the rates of these outcomes differed across these settings. We also examined visits among the APC subgroups (Appendix Tables 3 and 4, available at www.annals.org), which revealed few differences.
Table 2.
Unadjusted Frequencies of Utilization, by APC Versus Physician Status and Office-Versus Hospital-Based Clinics*
| Variable | Physicians | APCs | P Value |
|---|---|---|---|
| Weighted population, n | |||
|
| |||
| Office-based | 586 million | 25.8 million | |
|
| |||
| Hospital-based | 54.2 million | 14.6 million | |
| Antibiotics | |||
|
| |||
| Office-based | 1988/4074(49.1) | 98/191 (51.3) | 0.71 |
|
| |||
| Hospital-based | 2233/4742 (51.6) | 665/1281 (53.9) | 0.46 |
| CT/MRI | |||
|
| |||
| Office-based | 511/8156(6.3) | 12/283(3.3) | 0.111 |
|
| |||
| Hospital-based | 87/1680 (7.5) | 639/8666 (8.5) | 0.52 |
| Radiography | |||
|
| |||
| Office-based | 45/399 (9.4) | 987/10 093(10.1) | 0.74 |
|
| |||
| Hospital-based | 1390/11 015 (13.2) | 299/2436(11.6) | 0.24 |
| Referral to other physician | |||
|
| |||
| Office-based | 1066/12 170 (8.1) | 44/473 (9.2) | 0.54 |
|
| |||
| Hospital-based | 2546/13 359 (18.4) | 582/2947 (21.5) | 0.35 |
APC = advanced practice clinician; CT = computed tomography; MRI = magnetic resonance imaging.
Values are sample numerator/sample denominator (percentages) unless otherwise indicated. Proportions do not match percentages because the percentages represent national estimates based on population weighting.
Multivariable-Adjusted and Stratified Results
After multivariable adjustment, practice patterns among APCs and physicians remained consistent with the unadjusted findings in both office- and hospital-based settings (Table 3). Appendix Tables 5 and 6 (available at www.annals.org) present multivariable-adjusted results by visit and profession category.
Table 3.
Multivariable-Adjusted Frequencies of Utilization, by APC Versus Physician Status and Office-Versus Hospital-Based Clinics*
| Variable | Physicians | APCs | P Value |
|---|---|---|---|
| Sample/weighted population, n/N | |||
|
| |||
| Office-based | 12 170/586 million | 473/25.8 million | |
|
| |||
| Hospital-based | 13 359/54.2 million | 2947/14.6 million | |
| Antibiotics | |||
|
| |||
| Office-based | 49.2 | 49.4 | 0.96 |
|
| |||
| Hospital-based | 52.0 | 52.3 | 0.92 |
| CT/MRI | |||
|
| |||
| Office-based | 5.7 | 2.8 | 0.086 |
|
| |||
| Hospital-based | 7.3 | 6.4 | 0.48 |
| Radiography | |||
|
| |||
| Office-based | 9.8 | 8.7 | 0.65 |
|
| |||
| Hospital-based | 12.2 | 11.8 | 0.73 |
| Referral to other physician | |||
|
| |||
| Office-based | 7.4 | 8.1 | 0.64 |
|
| |||
| Hospital-based | 14.7 | 18.6 | 0.091 |
APC = advanced practice clinician; CT = computed tomography; MRI = magnetic resonance imaging; NAMCS = National Ambulatory Medical Care Survey.
Values are percentages unless otherwise indicated. Models are adjusted for age, sex, race/ethnicity, insurance status, modified Charlson comorbidity count, symptom acuity, and whether the provider self-identified as the patient’s primary care provider. Office-based (NAMCS) models also adjusted for practice setting.
Table 4 presents results stratified by PCP versus non-PCP visits. Hospital-based PCP APCs ordered more antibiotics (52.8% vs. 46.0%; P = 0.043) and made more referrals (11.8% vs. 8.3%; P = 0.018) than hospital-based PCP physicians. However, only referral differences remained significant in a sensitivity analysis of data recorded in the surveys from 2005 to 2011, after the wording change in the question regarding clinicians self-identifying as PCPs (see the Appendix for details). Test results for interaction were positive only for antibiotic use (P = 0.019 for interaction), suggesting that differences in antibiotic use between PCP APCs and PCP physicians were greater than those between non-PCP APCs and non-PCP physicians in the hospital setting. Table 5 presents results stratified by acute versus nonacute visits. Symptom-acuity stratification demonstrated that hospital-based APCs referred patients to other physicians for nonacute care more often than hospital-based physicians (20.3% vs. 11.4%; P = 0.022). Tests for interaction between acuity and APCs were nonsignificant for all outcomes. Practice settings with more independent APCs had results that were not substantively different from our main findings. Detailed results are presented in Appendix Table 7 (available at www.annals.org).
Table 4.
Multivariable-Adjusted Frequencies of Utilization, by APC Versus Physician Status, Office-Versus Hospital-Based Clinics, and PCP Versus Non-PCP Status*
| Variable | PCP | Non-PCP | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Physicians | APCs | P Value | Physicians | APCs | P Value | |
| Sample/weighted population, n/N | ||||||
|
| ||||||
| Office-based | 9592/468 million | 366/18.3 million | 2578/118 million | 107/7.5 million | ||
|
| ||||||
| Hospital-based | 6547/28.6 million | 1410/7.6 million | 6812/25.6 million | 1537/6.9 million | ||
| Antibiotics | ||||||
|
| ||||||
| Office-based | 48.7 | 51.9 | 0.52 | 50.9 | 45.2 | 0.61 |
|
| ||||||
| Hospital-based | 46.0 | 52.8 | 0.043 | 56.9 | 51.1 | 0.23 |
| CT/MRI | ||||||
|
| ||||||
| Office-based | 5.7 | 3.0 | 0.24 | 3.0 | 4.2 | 0.67 |
|
| ||||||
| Hospital-based | 7.1 | 6.4 | 0.70 | 4.4 | 5.8 | 0.34 |
| Radiography | ||||||
|
| ||||||
| Office-based | 10.0 | 10.9 | 0.71 | 8.5 | 3.3 | 0.097 |
|
| ||||||
| Hospital-based | 10.5 | 11.1 | 0.66 | 13.9 | 12.5 | 0.49 |
| Referral to other physician | ||||||
|
| ||||||
| Office-based | 7.6 | 7.8 | 0.88 | 6.6 | 8.6 | 0.57 |
|
| ||||||
| Hospital-based | 8.3 | 11.8 | 0.018 | 25.1 | 29.6 | 0.35 |
APC = advanced practice clinician; CT = computed tomography; MRI = magnetic resonance imaging; NAMCS = National Ambulatory Medical Care Survey; PCP = primary care provider.
Values are percentages unless otherwise indicated. Boldface values indicate comparisons with P < 0.05. Models are adjusted for age, sex, race/ethnicity, insurance status, modified Charlson comorbidity count, and symptom acuity. Office-based (NAMCS) models also adjusted for practice setting.
Table 5.
Multivariable-Adjusted Frequencies of Utilization, by APC Versus Physician Status, Office-Versus Hospital-Based Clinics, and Acute Versus Nonacute Visits*
| Variable | Acute | Nonacute | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Physicians | APCs | P Value | Physicians | APCs | P Value | |
| Sample/weighted population, n/N | ||||||
|
| ||||||
| Office-based | 8804/427 million | 360/20 million | 3366/160 million | 113/5.8 million | ||
|
| ||||||
| Hospital-based | 9847/40.7 million | 2581/12.8 million | 3512/13.6 million | 366/1.7 million | ||
| Antibiotics† | ||||||
|
| ||||||
| Office-based | 51.1 | 52.1 | 0.87 | 34.6 | 26.7 | 0.60 |
|
| ||||||
| Hospital-based | 54.1 | 53.8 | 0.93 | 22.9 | 29.9 | 0.40 |
| CT/MRI | ||||||
|
| ||||||
| Office-based | 6.8 | 2.7 | 0.061 | 3.7 | 3.4 | 0.91 |
|
| ||||||
| Hospital-based | 7.9 | 6.4 | 0.30 | 5.2 | 6.4 | 0.52 |
| Radiography | ||||||
|
| ||||||
| Office-based | 10.7 | 9.0 | 0.49 | 7.0 | 8.3 | 0.76 |
|
| ||||||
| Hospital-based | 12.0 | 11.6 | 0.75 | 11.7 | 12.1 | 0.86 |
| Referral to other physician | ||||||
|
| ||||||
| Office-based | 7.4 | 8.1 | 0.65 | 7.3 | 8.2 | 0.80 |
|
| ||||||
| Hospital-based | 15.5 | 18.5 | 0.27 | 11.4 | 20.3 | 0.022 |
APC = advanced practice clinician; CT = computed tomography; MRI = magnetic resonance imaging; NAMCS = National Ambulatory Medical Care Survey; PCP = primary care provider.
Values are percentages unless otherwise indicated. Boldface values indicate comparisons with P < 0.05. Models are adjusted for age, sex, race/ethnicity, insurance status, modified Charlson comorbidity count, and whether the provider self-identified as the patient’s PCP. Office-based (NAMCS) models also adjusted for practice setting.
Positive for interaction (P = 0.019), suggesting that differences in antibiotic use between PCP APCs and PCP physicians were greater than those between non-PCP APCs and non-PCP physicians in the hospital setting.
Discussion
This large national comparison between APCs and physicians on the use of potentially low-value health services revealed that APCs and physicians in both office- and hospital-based primary care settings provided equivalent amounts of guideline-discordant low-value care, including antibiotics, CT or MRI, plain radiography, and referrals to other physicians. Moreover, our results remained largely consistent when stratified by important potential effect modifiers, such as symptom acuity and whether the clinician self-identified as the PCP, although results did suggest that self-identified PCP APCs used more services than PCP physicians in the hospital-based setting. These findings have important implications for ongoing efforts to improve the quality and value of health care delivered in the United States as well as for the expanding role of APCs in primary care delivery.
Previous studies and meta-analyses showed that APC-provided care is similar in quality to that of physician-provided care, with equal or better outcomes (15). Despite this evidence, a recent national survey revealed that most physicians believe APCs provide lower-quality care than physicians, and nearly one quarter of those surveyed think expanding nurse practitioners’ role in U.S. practice would decrease the efficiency and value of care (18). Few studies, however, have compared APCs and physicians specifically in providing inefficient or low-value care. The existing literature is limited and shows mixed results, with some studies showing increased value and others showing no net change or lower value associated with APCs (15, 34, 35). Moreover, these studies focused mainly on health care costs, and few investigated the use of guideline-discordant and low-value health services as we did in our study. As debate continues over whether APCs’ scope of practice should expand (36), our analysis adds important data to the literature, suggesting that U.S. APCs seem to provide care equal to that of physicians in value and efficiency of delivery.
Our finding that APCs order antibiotics, CT or MRI, radiography, and referrals as frequently as physicians is reassuring given recent efforts to expand the number of APCs, as well as their role, to meet the increasing demand for primary care while the primary care physician workforce continues to shrink. Our results on antibiotic use among APCs and physicians are consistent with those of studies from a decade ago (37, 38). Our study builds on previous work by also demonstrating the similarities between APCs and physicians regarding potentially low-value referrals they make for conditions commonly encountered in primary care. The NAMCS and NHAMCS data we used also provide better clinical granularity and validity than earlier claims-based research, which frequently underrepresented APCs, who often bill under a physician’s name (39). The lack of differences in imaging use between APCs and physicians contrasts with recent research using Medicare claims data that showed greater imaging use among APCs than physicians (40). That study, however, included patients with multiple different presenting complaints of varying complexity. Consistent with our study, the authors found little to no difference among patients presenting with back pain or URI, which are relatively straightforward conditions with clearly defined guidelines. These findings are consistent with the hypothesis that APCs order imaging more frequently for patients whose conditions might be more complex than those we studied or for which guidelines are lacking.
Our analysis is subject to several limitations. First, because the NAMCS samples ambulatory visits to physician practices, it may exclude visits to more independent APCs or to APC-led practices, clearly underrepresenting APC care. However, we note that by law, physician assistants cannot practice without physician supervision, and previous research suggests that few nurse practitioners lead their own practices nationally (39). In addition, because the NHAMCS samples visits to outpatient departments rather than to physicians, it is considered more nationally representative of APCs in those settings and should be generalizable to APCs who practice at nonfederal outpatient hospital clinics (41). Moreover, although the NHAMCS represents a smaller proportion of care than office-based visits, our finding that NAMCS results were consistent with our NHAMCS results is reassuring.
Second, we could not identify low-value care precisely because we lacked granular clinical data. Thus, in some instances, such care might be justified. However, prominent clinical guidelines, specialty societies, and regulatory bodies previously identified these measures as being low-value in most circumstances. Moreover, our analyses excluded clinical red flags and controlled for age, symptom acuity, and comorbid conditions; thus, it is unlikely that variations in case complexity are confounding our results.
Third, we lacked longitudinal data at the patient level, as the NAMCS and NHAMCS are cross-sectional, visit-based surveys; thus, we could not assess whether various tests or referrals ordered were completed. However, we have no reason to suspect that completion rates would differ between APCs and physicians.
Fourth, we also could not account for variations in state-level scope-of-practice laws across the United States, which may limit an APC’s ability to order diagnostic tests (40, 42, 43). However, controlling for larger geographic regions did not affect our findings, and importantly, a recent rigorous analysis of the effect of state scope-of-practice laws on APC utilization revealed only a modest association at best (44).
We found that APCs and physicians ordered potentially guideline-discordant and low-value health services with similar frequency, dispelling physicians’ perceptions that APCs provide lower-value care than they do. We also acknowledge, however, that attributes of specific clinicians or practice settings might lead to practice patterns that differ from those we observed overall. As APCs rapidly expand their role in primary care, these findings have important implications for clinicians, practice leaders, and policymakers who have a stake in improving access to primary care services and ensuring the delivery of high-value care.
Acknowledgments
The authors acknowledge David Wilson, PhD, a senior research staff consultant with RTI International, SUDAAN Software Division.
Financial Support: Dr. Mafi was supported by National Research Service Award training grant T32HP12706 from the U.S. Health Services and Research Administration and by the Ryoichi Sasakawa Fellowship Fund. Dr. Wee was supported by National Institutes of Health Midcareer Mentorship Award K24DK087932. Dr. Davis was supported by Harvard Catalyst National Institutes of Health Award UL1 TR001102.
Appendix: Further Details and Subanalyses
Methods
Complex Design of the NAMCS and NHAMCS
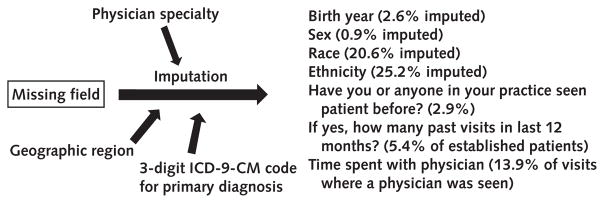
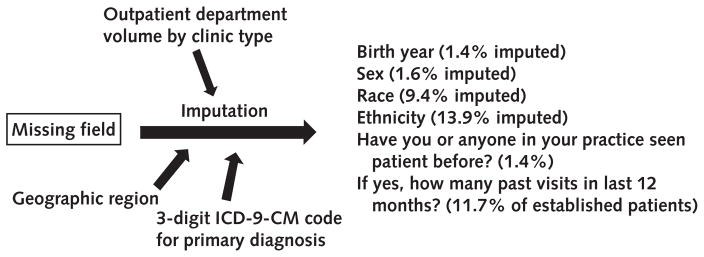
The NAMCS and NHAMCS both use a multistage probability sample design to acquire nationally representative samples of U.S. ambulatory visits to physicians (45). During the first stage, 112 geographic primary sampling units were selected from among those originally used in the National Health Interview Survey. For the second stage, physician office practices (NAMCS) or hospitals (NHAMCS) were chosen within these primary sampling units. In the last stage, a subset of visits to these office practices or outpatient departments was sampled during a prespecified period. This complex design allowed calculation of national-level estimates for physician visits and associated SEs by using the survey weights provided by the National Center for Health Statistics. See Appendix Figures 1 and 2 for details on imputation methods to handle missing values.
Excluding Midwives
From 1997 through 2000, the NAMCS and NHAMCS included midwives and nurse practitioners as separate variables; from 2001 through 2011, they were combined into a single element. We examined visits to midwives and nurse practitioners for the selected conditions from 1997 to 2000 in our cohort and identified 14 midwife and 709 nurse practitioner visits, suggesting that the combined variable from 2001 to 2011 captures predominantly nurse practitioner visits in our primary care–focused cohort.
NAMCS and NHAMCS Wording Change on Whether Clinician Self-Identified as the PCP
From 1997 through 2004, the NAMCS and NHAMCS asked, “Are you the patient’s primary care physician?” Therefore, some APCs may have answered “no” because they were not physicians. From 2005 through 2011, the NAMCS question was changed to “Are you the patient’s primary care physician/provider?” In addition, from 2005 through 2006, the NHAMCS question became “Are you the patient’s primary care physician/provider?” Finally, from 2007 through 2011, the NHAMCS asked, “Is this clinic the patient’s primary care provider?” We therefore compared the frequency of APCs self-identifying as the PCP from 1997 to 2004 versus 2005 to 2011. We found that the frequency increased on both the NAMCS (59.5% from 1997 to 2004, to 78.3% from 2005 to 2011; P = 0.21) and NHAMCS (42.4% from 1997 to 2004, to 59.6% from 2005 to 2011; P = 0.030). Therefore, we evaluated whether our findings that PCP APCs ordered more antibiotics and referrals than PCP physicians in the hospital setting remained true after the surveys’ wording change starting in 2005. We found that although differences in referral patterns remained significant (18.2% among PCP APCs vs. 10.5% among PCP physicians; P < 0.001), differences in antibiotic use no longer were significant (47.8% among PCP APCs vs. 50.9% among PCP physicians; P = 0.60) in the hospital setting from 2005 to 2011.
Selecting Generalists in the Primary Care Setting by Using NAMCS and NHAMCS Data
The NAMCS provides detailed specialty data, allowing us to restrict our analysis to general, family, and internal medicine physicians and APCs. Although the NHAMCS does not provide detailed specialty information on the physician or APC, it does allow restriction of the analysis to “general medical clinics” as opposed to surgical or other specialty clinics. General medical clinics exclude most specialists who treat URIs (such as otolaryngologists), back pain (such as orthopedic surgeons, neurosurgeons, anesthesiologists, and pain specialists), and headache (such as neurologists and pain specialists).
To confirm that general medicine clinics excluded relevant specialists (general medical clinics include some other medical subspecialists), we used the NAMCS to examine all visits for the identified symptoms to determine the extent to which these symptoms were seen by specialists. Most patients presenting with back pain, headache, and URIs were treated by generalists, internists, and family physicians, with the rest being seen predominantly by orthopedic/neurosurgeons; neurologists; and ear, nose, and throat physicians, respectively, none of whom are part of the NHAMCS general medical clinics (rather, they are part of “surgical” and “other” clinics).
Results
Subcategory Analysis
Findings in the subcategory analysis were not substantively different from our main results, with few exceptions (see Appendix Tables 3 to 6 for details). For example, nurse practitioners seeing patients alongside physicians were less likely to order antibiotics (with multivariable-adjusted rates of 27.3% vs. 49.2%; P = 0.034) than physicians alone in the office-based setting (Appendix Table 5). However, nurse practitioners seeing patients alongside physicians were more likely to refer patients to other physicians (multivariable-adjusted rates of 23.5% vs. 14.8%; P = 0.044) than physicians in the hospital-based setting (Appendix Table 6).
Practice Setting Sensitivity Analyses
Adding the practice setting variable to our NAMCS multivariable models did not change our results, and interacting practice setting with APC provider in our NAMCS subset revealed no significant findings, suggesting that practice setting in the NAMCS was not associated with differences in provider behavior. In addition, when we evaluated physician practices or hospitals in which nurse practitioners and physician assistants predominantly practiced independently (Appendix Table 7; see columns for “Nurse Practitioners: Always Alone” and “Physician Assistants: Always Alone”), our findings were consistent with our overall results, with few exceptions. For example, physician assistants who predominantly see patients alone ordered antibiotics more frequently than physicians practicing alone (71.6% vs. 49.1%; P = 0.020).
We note, however, that these subanalyses are imperfect because of small sample sizes, and we remain concerned about multiple testing and potential bias in creating these categories. Hence, we limit these results to the Appendix.
Appendix Figure 1.
NAMCS missing data procedures.
Some missing data were imputed by randomly assigning a value from a patient record survey form with similar characteristics. Imputations were based on physician specialty, geographic region, and 3-digit ICD-9-CM codes for primary diagnosis. ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; NAMCS = National Ambulatory Medical Care Survey.
Appendix Figure 2.
NHAMCS outpatient department missing data procedures.
Some missing data were imputed by randomly assigning a value from a patient record survey form with similar characteristics. Imputations were based on outpatient department volume by clinic type, geographic region, and 3-digit ICD-9-CM codes for primary diagnosis. ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; NHAMCS = National Hospital Ambulatory Medical Care Survey.
Appendix Table 1.
Demographic Characteristics, by Clinician Type, in Physician Offices (NAMCS)*
| Characteristic | Physician (Reference) (n = 12 170) | Nurse Practitioner Only (n = 70) | P Value | Nurse Practitioner and Physician (n = 103) | P Value | Physician Assistant Only (n = 82) | P Value | Physician Assistant and Physician (n = 218) | P Value |
|---|---|---|---|---|---|---|---|---|---|
| Mean age, y | 48.9 | 47.0 | 0.36 | 46.8 | 0.37 | 47.1 | 0.29 | 49.1 | 0.91 |
|
| |||||||||
| Female | 62.7 | 83.9 | 61.7 | 63.8 | 56.7 | 0.068† | |||
| Race/ethnicity | 0.029† | ||||||||
|
| |||||||||
| White | 76.9 | 85.5 | 71.9 | 70.4 | 79.3 | ||||
|
| |||||||||
| Black | 10.3 | 9.1 | 9.8 | 13.0 | 10.9 | ||||
|
| |||||||||
| Hispanic | 8.3 | 5.3 | 16.4 | 14.7 | 7.0 | ||||
|
| |||||||||
| Other | 4.6 | 0.01 | 1.9 | 1.9 | 2.8 | ||||
|
| |||||||||
| Mean Charlson comorbidity count | 0.047 | 0.049 | 0.95 | 0.032 | 0.41 | 0.047 | NA | 0.046 | 0.93 |
|
| |||||||||
| Acute symptoms | 72.7 | 84.3 | 71.7 | 77.7 | 77.4 | 0.37† | |||
| Insurance | 0.21† | ||||||||
|
| |||||||||
| Private | 57.6 | 61.0 | 56.4 | 72.9 | 66.7 | ||||
|
| |||||||||
| Medicare/Medicaid | 26.7 | 21.4 | 21.6 | 15.3 | 23.2 | ||||
|
| |||||||||
| Other | 15.8 | 17.6 | 22.0 | 11.9 | 10.0 | ||||
|
| |||||||||
| Provider identifies as PCP | 79.9 | 88.5 | 70.9 | 68.9 | 65.5 | 0.193† | |||
|
| |||||||||
| Urban location | 82.1 | 54.1 | 61.3 | 79.2 | 95.4 | 0.011† | |||
|
| |||||||||
| Region | 0.062† | ||||||||
| Northeast | 19.1 | 13.9 | 12.8 | 19.5 | 19.0 | ||||
|
| |||||||||
| Midwest | 24.2 | 28.7 | 36.8 | 8.6 | 23.0 | ||||
|
| |||||||||
| South | 35.5 | 49.3 | 45.0 | 60.3 | 42.3 | ||||
|
| |||||||||
| West | 21.2 | 8.1 | 5.4 | 11.6 | 15.7 | ||||
|
| |||||||||
| Symptom group | |||||||||
| URIs | 35.7 | 54.0 | 48.9 | 41.1 | 39.9 | 0.054† | |||
|
| |||||||||
| Back pain | 47.4 | 32.8 | 33.2 | 32.3 | 48.7 | 0.003† | |||
|
| |||||||||
| Headache | 18.2 | 15.9 | 22.2 | 26.7 | 12.5 | 0.108† | |||
NA = not available; NAMCS = National Ambulatory Medical Care Survey; PCP = primary care provider; URI = upper respiratory infection.
Values are percentages unless otherwise indicated and may not sum to 100 due to rounding. Boldface values indicate comparisons with P < 0.05.
Represents global chi-square tests among all clinician subtypes.
Appendix Table 2.
Demographic Characteristics, by Clinician Type, in Hospital Clinics (NHAMCS)*
| Characteristic | Physician (Reference) (n = 13 359) |
Nurse Practitioner Only (n = 1400) |
P Value | Nurse Practitioner and Physician (n = 191) |
P Value | Physician Assistant Only (n = 1152) |
P Value | Physician Assistant and Physician (n = 204) |
P Value |
|---|---|---|---|---|---|---|---|---|---|
| Mean age, y | 45.0 | 42.2 | 0.003 | 46.3 | 0.58 | 42.1 | 0.006 | 44.2 | 0.63 |
|
| |||||||||
| Female | 64.4 | 67.1 | 58.3 | 66.7 | 63.7 | 0.51† | |||
| Race/ethnicity | 0.002† | ||||||||
|
| |||||||||
| White | 70.6 | 81.4 | 59.2 | 82.0 | 67.2 | ||||
|
| |||||||||
| Black | 16.7 | 8.3 | 17.7 | 9.3 | 8.1 | ||||
|
| |||||||||
| Hispanic | 9.7 | 6.3 | 20.0 | 6.3 | 14.7 | ||||
|
| |||||||||
| Other | 3.0 | 4.0 | 3.1 | 2.5 | 10.0 | ||||
|
| |||||||||
| Mean Charlson comorbidity count | 0.049 | 0.021 | <0.001 | 0.059 | 0.68 | 0.015 | <0.001 | 0.039 | 0.70 |
|
| |||||||||
| Acute symptoms | 75.0 | 89.6 | 75.4 | 88.7 | 81.2 | <0.001† | |||
| Insurance | 0.007† | ||||||||
|
| |||||||||
| Private | 46.0 | 41.8 | 45.8 | 43.4 | 28.3 | ||||
|
| |||||||||
| Medicare/Medicaid | 33.4 | 34.5 | 37.4 | 28.7 | 41.2 | ||||
|
| |||||||||
| Other | 20.6 | 23.7 | 16.8 | 27.9 | 30.5 | ||||
|
| |||||||||
| Provider identifies as PCP | 52.8 | 59.3 | 28.0 | 49.6 | 38.0 | 0.027† | |||
|
| |||||||||
| Urban location | 81.7 | 51.2 | 83.9 | 39.5 | 74.3 | <0.001† | |||
|
| |||||||||
| Region | 0.126 | ||||||||
| Northeast | 17.6 | 19.4 | 12.9 | 14.4 | 28.1 | ||||
|
| |||||||||
| Midwest | 37.2 | 26.0 | 33.1 | 25.1 | 16.6 | ||||
|
| |||||||||
| South | 30.8 | 45.4 | 37.6 | 35.8 | 26.6 | ||||
|
| |||||||||
| West | 14.4 | 9.3 | 16.5 | 24.7 | 28.6 | ||||
|
| |||||||||
| Symptom group | |||||||||
| URIs | 37.1 | 43.8 | 35.7 | 42.0 | 31.8 | 0.046† | |||
|
| |||||||||
| Back pain | 46.0 | 38.0 | 53.1 | 43.3 | 47.6 | 0.060† | |||
|
| |||||||||
| Headache | 18.1 | 20.0 | 12.9 | 16.2 | 20.6 | 0.178† | |||
NHAMCS = National Hospital Ambulatory Medical Care Survey; PCP = primary care provider; URI = upper respiratory infection.
Values are percentages unless otherwise indicated and may not sum to 100 due to rounding. Boldface values indicate comparisons with P < 0.05.
Represents global chi-square tests among all clinician subtypes.
Appendix Table 3.
Unadjusted Proportions of Utilization, by Clinician Type, in the NAMCS Only*
| Variable | Physician (Reference) (n = 12 170) | Nurse Practitioner Only (n = 70) | P Value | Nurse Practitioner and Physician (n = 103) | P Value | Physician Assistant Only (n = 82) | P Value | Physician Assistant and Physician (n = 218) | P Value |
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics | 1988/4074(49.1) | 15/32 (48.7) | 0.96 | 18/47 (29.0) | 0.057 | 23/34(61.0) | 0.29 | 42/78 (59.4) | 0.083 |
| CT/MRI | 511/8156(6.3) | 0/39 (0) | NA | 4/56 (8.8) | 0.60 | 2/48 (2.2) | 0.123 | 6/140 (2.9) | 0.22 |
| Radiography | 987/10 093 (10.1) | 8/61 (10.7) | 0.92 | 10/88 (6.4) | 0.28 | 8/62 (13.8) | 0.45 | 19/188 (8.4) | 0.62 |
| Referral to other physician | 1066/12 170 (8.1) | 4/70 (8.8) | 0.85 | 11/103(9.3) | 0.75 | 7/82 (7.2) | 0.82 | 22/218 (10.2) | 0.46 |
CT = computed tomography; MRI = magnetic resonance imaging; NA = not available; NAMCS = National Ambulatory Medical Care Survey.
Values are sample numerator/sample denominator (percentages). Proportions may not match percentages because the percentages represent national estimates based on population weighting.
Appendix Table 4.
Unadjusted Proportions of Utilization, by Clinician Type, in the NHAMCS Only*
| Variable | Physician (Reference) (n = 13 359) |
Nurse Practitioner Only (n = 1400) |
P Value | Nurse Practitioner and Physician (n = 191) |
P Value | Physician Assistant Only (n = 1130) |
P Value | Physician Assistant and Physician (n = 204) |
P Value |
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics | 2233/4742 (51.6) | 335/637 (55.5) | 0.35 | 28/64(48.4) | 0.66 | 271/516(53.0) | 0.73 | 31/64 (47.4) | 0.66 |
| CT/MRI | 639/8666 (8.5) | 41/771 (6.7) | 0.38 | 12/128(18.3) | 0.057 | 27/641 (7.0) | 0.51 | 7/140(4.9) | 0.20 |
| Radiography | 1390/11 015 (13.2) | 140/1153 (11.9) | 0.52 | 27/159(17.7) | 0.30 | 102/964(9.8) | 0.040 | 30/160(15.9) | 0.46 |
| Referral to other physician | 2546/13 359 (18.4) | 267/1400 (22.6) | 0.46 | 53/191 (33.6) | 0.017 | 207/1152 (17.7) | 0.81 | 55/204 (25.9) | 0.146 |
CT = computed tomography; MRI = magnetic resonance imaging; NHAMCS = National Hospital Ambulatory Medical Care Survey.
Values are sample numerator/sample denominator (percentages). Proportions may not match percentages because the percentages represent national estimates based on population weighting. Boldface values indicate comparisons with P < 0.05.
Appendix Table 5.
Multivariable-Adjusted Proportions of Utilization, by Clinician Type, in Physician Offices (NAMCS)*
| Variable | Physician (Reference) (n = 12 170) | Nurse Practitioner Only (n = 70) | P Value | Nurse Practitioner and Physician (n = 103) | P Value | Physician Assistant Only (n = 82) | P Value | Physician Assistant and Physician (n = 218) | P Value |
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics | 49.2 | 46.8 | 0.78 | 27.3 | 0.034 | 56.5 | 0.51 | 59.1 | 0.101 |
| CT/MRI | 5.7 | 0 | NA | 7.7 | 0.66 | 2.2 | 0.140 | 2.2 | 0.163 |
| Radiography | 9.8 | 10.1 | 0.95 | 6.5 | 0.34 | 12.6 | 0.56 | 7.6 | 0.52 |
| Referral to other physician | 7.4 | 8.2 | 0.83 | 8.5 | 0.74 | 6.8 | 0.88 | 0 | 0.62 |
CT = computed tomography; MRI = magnetic resonance imaging; NA = not available; NAMCS = National Ambulatory Medical Care Survey.
Values are percentages. Proportions may not match percentages because the percentages represent national estimates based on population weighting. Boldface values indicate comparisons with P < 0.05.
Appendix Table 6.
Multivariable-Adjusted Proportions of Utilization, by Clinician Type, in Hospital Clinics (NHAMCS)*
| Variable | Physician (Reference) (n = 13 359) | Nurse Practitioner Only (n = 1400) | P Value | Nurse Practitioner and Physician (n = 191) | P Value | Physician Assistant Only (n = 1152) | P Value | Physician Assistant and Physician (n = 204) | P Value |
|---|---|---|---|---|---|---|---|---|---|
| Antibiotics | 51.9 | 52.7 | 0.88 | 48.1 | 0.56 | 52.8 | 0.83 | 47.7 | 0.70 |
| CT/MRI | 7.3 | 5.4 | 0.25 | 13.7 | 0.056 | 6.6 | 0.68 | 3.9 | 0.182 |
| Radiography | 12.2 | 12.0 | 0.91 | 13.5 | 0.68 | 10.6 | 0.31 | 15.0 | 0.45 |
| Referral to other physician | 14.8 | 19.4 | 0.22 | 23.5 | 0.044 | 16.6 | 0.38 | 19.5 | 0.25 |
CT = computed tomography; MRI = magnetic resonance imaging; NHAMCS = National Hospital Ambulatory Medical Care Survey.
Values are percentages. Proportions may not match percentages because the percentages represent national estimates based on population weighting. Boldface values indicate comparisons with P < 0.05.
Appendix Table 7.
Unadjusted Sensitivity Analysis of Proportions of Service Use Among Various Collaborative Practice Arrangements*
| Variable | Physicians Always Alone (Reference) | Nurse Practitioners | Physician Assistants | Nurse Practitioner Visits Alone or Shared | P Value | Physician Assistant Visits Alone or Shared | P Value | Practices With Too Few Visits to Be Categorized | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||
| Always Alone | P Value | Always Shared | P Value | Always Alone | P Value | Always Shared | P Value | |||||||
| Antibiotics | ||||||||||||||
|
| ||||||||||||||
| Physician offices | 1489/3019(49.1) | 5/13(40.6) | 0.50 | 18/53 (30.1) | 0.093 | 22/34 (71.6) | 0.020 | 63/130 (47.4) | 0.78 | 0(0) | NA | 0(0) | NA | 489/1016(50.4) |
|
| ||||||||||||||
| Hospital clinics | 203/454 (54.0) | 590/1191 (54.4) | 0.93 | 27/64 (43.8) | 0.37 | 685/1367(52.7) | 0.74 | 81/178 (46.7) | 0.29 | 130/257 (54.6) | 0.93 | 51/113(42.5) | 0.182 | 1131/2399 (51.2) |
| CT/MRI | ||||||||||||||
|
| ||||||||||||||
| Physician offices | 373/6078 (6.0) | 0/25 (0) | NA | 3/76 (3.2) | 0.28 | 4/38 (9.9) | 0.30 | 12/184 (6.8) | 0.69 | 0(0) | NA | 0(0) | NA | 131/2038 (6.7) |
|
| ||||||||||||||
| Hospital clinics | 43/789 (11.9) | 140/2203 (7.1) | 0.20 | 11/247 (2.8) | 0.015 | 167/2161 (7.9) | 0.27 | 20/255 (8.3) | 0.46 | 33/332 (12.9) | 0.85 | 14/203 (8.1) | 0.54 | 298/4156 (8.4) |
| Radiography | ||||||||||||||
|
| ||||||||||||||
| Physician offices | 723/7518(10.2) | 2/28 (5.0) | 0.34 | 9/92 (7.5) | 0.41 | 6/60 (11.4) | 0.71 | 28/267 (9.5) | 0.75 | 0(0) | NA | 0(0) | NA | 264/2527 (10.2) |
|
| ||||||||||||||
| Hospital clinics | 125/1029 (14.4) | 343/2809 (13.2) | 0.70 | 21/252 (9.4) | 0.188 | 346/2909(11.8) | 0.28 | 52/367(12.1) | 0.57 | 96/493 (17.0) | 0.62 | 34/236(15.3) | 0.83 | 672/5356(12.6) |
| Referral to other physician | ||||||||||||||
|
| ||||||||||||||
| Physician offices | 789/9052 (8.2) | 1/37 (1.7) | 0.104 | 7/128 (3.8) | 0.113 | 6/72 (5.9) | 0.52 | 30/314(8.6) | 0.86 | 0(0) | NA | 0(0) | NA | 277/3040 (8.3) |
|
| ||||||||||||||
| Hospital clinics | 206/1241 (16.2) | 625/3385 (16.3) | 0.98 | 50/311 (10.0) | 0.28 | 625/3514(18.9) | 0.56 | 86/433(13.3) | 0.60 | 119/584 (27.5) | 0.25 | 107/313(24.4) | 0.34 | 1310/6525(20.5) |
CT = computed tomography; MRI = magnetic resonance imaging; NA = not available; NAMCS = National Ambulatory Medical Care Survey; NHAMCS = National Hospital Ambulatory Medical Care Survey.
Values are sample numerator/sample denominator (percentages). Boldface values indicate comparisons with P < 0.05. Of note, categories are created on the basis of whether there are at least 4 observations occurring with each physician (NAMCS) or hospital (NHAMCS) clinic. The cutoff of 4 was chosen because it represents the median number of advanced practice clinician providers in each provider setting. For example, if a physician or hospital has >4 visits with nurse practitioners seeing patients alone (and 0 patients in shared visits), then this practice and its visits would fall under the first column (Nurse Practitioners Always Alone). Or if a practice has >4 nurse practitioner alone visits and >4 nurse practitioner shared visits, then we conclude that this practice allows for discretionary sharing. Also, percentages may differ from numerator/denominator proportion because of sample weighting. Finally, mixed-practice settings in this table occur only in the hospital clinic setting (NHAMCS data).
Footnotes
Author Contributions: Conception and design: J.N. Mafi, C.C. Wee, B.E. Landon.
Analysis and interpretation of the data: J.N. Mafi, R.B. Davis, B.E. Landon.
Drafting of the article: J.N. Mafi.
Critical revision for important intellectual content: J.N. Mafi, C.C. Wee, R.B. Davis, B.E. Landon.
Final approval of the article: J.N. Mafi, C.C. Wee, R.B. Davis, B.E. Landon.
Statistical expertise: R.B. Davis.
Obtaining of funding: C.C. Wee.
Administrative, technical, or logistic support: J.N. Mafi, B.E. Landon.
Collection and assembly of data: J.N. Mafi.
Presented in oral abstract form at the New England Regional Meeting of the Society of General Internal Medicine (SGIM) in Boston, Massachusetts, March 2015, and at the SGIM 38th Annual Meeting, in Toronto, Ontario, Canada, April 2015, and in abstract form at the Annual Research Meeting of Academy-Health, in Minneapolis, Minnesota, June 2015.
Disclosures: Dr. Davis reports grants from the National Institutes of Health during the conduct of the study and personal fees from the American Heart Association outside the submitted work. Dr. Landon reports personal fees from United Biosource and Research Triangle Institute outside the submitted work. Authors not named here have disclosed no conflicts of interest. Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M15-2152.
Reproducible Research Statement: Study protocol: Available from Dr. Mafi (jmafi@mednet.ucla.edu). Statistical code: Interested readers may contact Dr. Mafi for discussion. Data set: Available from Centers for Disease Control and Prevention, National Center for Health Statistics (www.cdc.gov/nchs/ahcd/).
Current author addresses and author contributions are available at www.annals.org.
References
- 1.Schwartz MD. Health care reform and the primary care workforce bottleneck. J Gen Intern Med. 2012;27:469–72. doi: 10.1007/s11606-011-1921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Health Aff (Millwood) 2008;27:w232–41. doi: 10.1377/hlthaff.27.3.w232. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. Projecting the Supply and Demand for Primary Care Practitioners Through 2020. Rockville, MD: U.S. Department of Health and Human Services; 2013. [on 20 January 2016]. Accessed at http://bhpr.hrsa.gov/healthworkforce/supplydemand/usworkforce/primarycare/projectingprimarycare.pdf? [Google Scholar]
- 4.Petterson SM, Liaw WR, Phillips RL, Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10:503–9. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipner RS, Bylsma WH, Arnold GK, Fortna GS, Tooker J, Cassel CK. Who is maintaining certification in internal medicine—and why? A national survey 10 years after initial certification. Ann Intern Med. 2006;144:29–36. doi: 10.7326/0003-4819-144-1-200601030-00007. [DOI] [PubMed] [Google Scholar]
- 6.Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44:234–42. doi: 10.1097/01.mlr.0000199848.17133.9b. [DOI] [PubMed] [Google Scholar]
- 7.Edwards ST, Mafi JN, Landon BE. Trends and quality of care in outpatient visits to generalist and specialist physicians delivering primary care in the United States, 1997–2010. J Gen Intern Med. 2014;29:947–55. doi: 10.1007/s11606-014-2808-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health Aff (Millwood) 2009;28:64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff (Millwood) 2013;32:1881–6. doi: 10.1377/hlthaff.2013.0234. [DOI] [PubMed] [Google Scholar]
- 10.Mehrotra A, Liu H, Adams JL, Wang MC, Lave JR, Thygeson NM, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151:321–8. doi: 10.7326/0003-4819-151-5-200909010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roblin DW, Howard DH, Becker ER, Kathleen Adams E, Roberts MH. Use of midlevel practitioners to achieve labor cost savings in the primary care practice of an MCO. Health Serv Res. 2004;39:607–26. doi: 10.1111/j.1475-6773.2004.00247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Aff (Millwood) 2010;29:893–9. doi: 10.1377/hlthaff.2010.0440. [DOI] [PubMed] [Google Scholar]
- 13.Chenoweth D, Martin N, Pankowski J, Raymond LW. Nurse practitioner services: three-year impact on health care costs. J Occup Environ Med. 2008;50:1293–8. doi: 10.1097/JOM.0b013e318184563a. [DOI] [PubMed] [Google Scholar]
- 14.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martínez-González NA, Djalali S, Tandjung R, Huber-Geismann F, Markun S, Wensing M, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14:214. doi: 10.1186/1472-6963-14-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson IB, Landon BE, Hirschhorn LR, McInnes K, Ding L, Marsden PV, et al. Quality of HIV care provided by nurse practitioners, physician assistants, and physicians. Ann Intern Med. 2005;143:729–36. doi: 10.7326/0003-4819-143-10-200511150-00010. [DOI] [PubMed] [Google Scholar]
- 17.Mundinger MO, Kane RL, Lenz ER, Totten AM, Tsai WY, Cleary PD, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA. 2000;283:59–68. doi: 10.1001/jama.283.1.59. [DOI] [PubMed] [Google Scholar]
- 18.Donelan K, DesRoches CM, Dittus RS, Buerhaus P. Perspectives of physicians and nurse practitioners on primary care practice. N Engl J Med. 2013;368:1898–906. doi: 10.1056/NEJMsa1212938. [DOI] [PubMed] [Google Scholar]
- 19.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 20.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173:1573–81. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mafi JN, Edwards ST, Pedersen NP, Davis RB, McCarthy EP, Landon BE. Trends in the ambulatory management of headache: analysis of NAMCS and NHAMCS data 1999–2010. J Gen Intern Med. 2015;30:548–55. doi: 10.1007/s11606-014-3107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174:1067–76. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsiao C. [on 20 January 2016];Understanding and using NAMCS and NHAMCS data: data tools and basic programming techniques. 2010 Accessed at www.cdc.gov/nchs/ppt/nchs2010/03_Hsiao.pdf.
- 24.Centers for Disease Control and Prevention. [on 20 January 2016];Using ultimate cluster models with NAMCS and NHAMCS public use files. 2004 Accessed at www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf.
- 25.Atwater A, Bednar S, Hassman D, Khouri J. Nurse practitioners and physician assistants in primary care. Dis Mon. 2008;54:728–44. doi: 10.1016/j.disamonth.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996–2010. JAMA. 2014;311:2020–2. doi: 10.1001/jama.2013.286141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997–2010. JAMA Intern Med. 2014;174:138–40. doi: 10.1001/jamainternmed.2013.11673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gonzales R, Bartlett JG, Besser RE, Cooper RJ, Hickner JM, Hoffman JR, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med. 2001;134:479–86. doi: 10.7326/0003-4819-134-6-200103200-00013. [DOI] [PubMed] [Google Scholar]
- 29.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Clinical Efficacy Assessment Subcommittee of the American College of Physicians. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 30.National Committee for Quality Assurance. [on 20 January 2016];Summary table of measure changes. 2015 Accessed at www.ncqa.org/Portals/0/HEDISQM/Hedis2015/HEDIS%202015%20Physician%20Measures%20List.pdf.
- 31.Goertz M, Thorson D, Bonsell J, Bonte B, Campbell R, Haake B, et al. Institute for Clinical Systems Improvement. Adult Acute and Subacute Low Back Pain. Bloomington, MN: Institute for Clinical Systems Improvement; 2012. [Google Scholar]
- 32.Hainer BL, Matheson EM. Approach to acute headache in adults. Am Fam Physician. 2013;87:682–7. [PubMed] [Google Scholar]
- 33.Peek ME, Tang H, Alexander GC, Chin MH. National prevalence of lifestyle counseling or referral among African-Americans and whites with diabetes. J Gen Intern Med. 2008;23:1858–64. doi: 10.1007/s11606-008-0737-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hemani A, Rastegar DA, Hill C, al-Ibrahim MS. A comparison of resource utilization in nurse practitioners and physicians. Eff Clin Pract. 1999;2:258–65. [PubMed] [Google Scholar]
- 35.Martin-Misener R, Harbman P, Donald F, Reid K, Kilpatrick K, Carter N, et al. Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: systematic review. BMJ Open. 2015;5:e007167. doi: 10.1136/bmjopen-2014-007167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iglehart JK. Expanding the role of advanced nurse practitioners—risks and rewards. N Engl J Med. 2013;368:1935–41. doi: 10.1056/NEJMhpr1301084. [DOI] [PubMed] [Google Scholar]
- 37.Linder JA, Singer DE, Stafford RS. Association between antibiotic prescribing and visit duration in adults with upper respiratory tract infections. Clin Ther. 2003;25:2419–30. doi: 10.1016/s0149-2918(03)80284-9. [DOI] [PubMed] [Google Scholar]
- 38.Gonzales R, Barrett PH, Jr, Crane LA, Steiner JF. Factors associated with antibiotic use for acute bronchitis. J Gen Intern Med. 1998;13:541–8. doi: 10.1046/j.1525-1497.1998.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuo YF, Loresto FL, Jr, Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Aff (Millwood) 2013;32:1236–43. doi: 10.1377/hlthaff.2013.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hughes DR, Jiang M, Duszak R., Jr A comparison of diagnostic imaging ordering patterns between advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Intern Med. 2015;175:101–7. doi: 10.1001/jamainternmed.2014.6349. [DOI] [PubMed] [Google Scholar]
- 41.Morgan PA, Strand J, Ostbye T, Albanese MA. Missing in action: care by physician assistants and nurse practitioners in national health surveys. Health Serv Res. 2007;42:2022–37. doi: 10.1111/j.1475-6773.2007.00700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gadbois EA, Miller EA, Tyler D, Intrator O. Trends in state regulation of nurse practitioners and physician assistants, 2001 to 2010. Med Care Res Rev. 2015;72:200–19. doi: 10.1177/1077558714563763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Christian S, Dower C, O’Neil E. Overview of Nurse Practitioner Scopes of Practice in the United States—Discussion. San Francisco, CA: UCSF Center for the Health Professions; 2007. [on 6 June 2016]. Accessed at http://enp-network.s3.amazonaws.com/NP_Alliance/PDF/NPScopes.pdf. [Google Scholar]
- 44.Stange K. How does provider supply and regulation influence health care markets? Evidence from nurse practitioners and physician assistants. J Health Econ. 2014;33:1–27. doi: 10.1016/j.jhealeco.2013.10.009. [DOI] [PubMed] [Google Scholar]
Web-Only Reference
- 45.McCaig LF, McLemore T. Plan and operation of the National Hospital Ambulatory Medical Survey. Series 1: programs and collection procedures. Vital Health Stat. 1994;1:1–78. [PubMed] [Google Scholar]