Abstract
Background:
A 61-year-old man presented with upper abdominal pain and jaundice. Abdominal computed tomography imaging revealed stones in the gallbladder and the common bile duct, with a thickening of the gallbladder wall and an obvious increase in the volume of the gallbladder. Initial treatment using endoscopic retrograde cholangiopancreatography failed due to the presence of surgically altered gastrointestinal anatomy. Stones in the gallbladder and common bile duct were subsequently removed concurrently via percutaneous transhepatic papilla balloon dilatation combined with a percutaneous transcystic approach. Liver function recovered rapidly, with total bilirubin and direct bilirubin levels decreasing to normal, with a concomitant improvement in hemoglobin and thrombocyte levels and resolution of the upper abdominal pain and jaundice.
Conclusion:
Percutaneous transhepatic papilla balloon dilatation, combined with a percutaneous transcystic approach, provided an effective alternative treatment for removing concurrent stones in the common bile duct and gallbladder in a patient with a previous Billroth II gastrectomy and presenting with an acute cholecystitis.
Keywords: acute cholecystitis, common bile duct stone, gallbladder stone, percutaneous transcystic, percutaneous transhepatic papilla dilation
1. Introduction
Biliary lithiasis is a worldwide disease that affects 20% of the general population, with approximately 15% of patients presenting with concurrent gallbladder (GB) and common bile duct (CBD) stones.[1,2] Laparoscopic cholecystectomy (LC) is regarded as the standard treatment for GB stones, with endoscopic stone extraction combined with LC widely accepted as the treatment of choice for the treatment of concurrent GB and CBD stones.[3] However, transpapillary endoscopic approaches, such as endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (EST), are technically challenging to perform in patients with surgically altered gastrointestinal anatomy, and Roux-en-Y reconstruction in particular, due to difficulty in cannulating the bile duct.[4]
In the patient, we present in this case report, ERCP had previously been attempted but failed because of the presence of surgically altered gastrointestinal anatomy. Consequently, we performed percutaneous transhepatic papilla balloon dilatation (PTBD) combined with a percutaneous transcystic approach as a 1-step procedure for removal of concurrent GB and CBD stones. The consent for case publication was obtained from the patient.
2. Case report
A 61-year-old man presented to our hospital with upper abdominal pain and jaundice. Abdominal computed tomography imaging revealed a 5-mm stone in the inferior portion of the gallbladder (Fig. 1A) and an 8 mm CBD stone (Fig. 1B). A thickened gallbladder wall and an obvious increase in the volume of the gallbladder were also observed. The patient had previously undergone a Billroth II surgery for treatment of a gastric carcinoma, 12 years earlier. Surgical treatment had been followed by FOLFOX4 combination chemotherapy, consisting of oxaliplatin 85 mg/(m2•d), ivgtt, d1, leucovorin 200 mg/m2, ivgtt 2 hours followed by 5-fluorouracil 400 mg/m2, and 5-fluorouracil 600 mg/m2 (22 h-continuous infusion). The FOLFOX4 regimen was repeated at a 2-week interval, with 4 weeks to complete 1 cycle.
Figure 1.
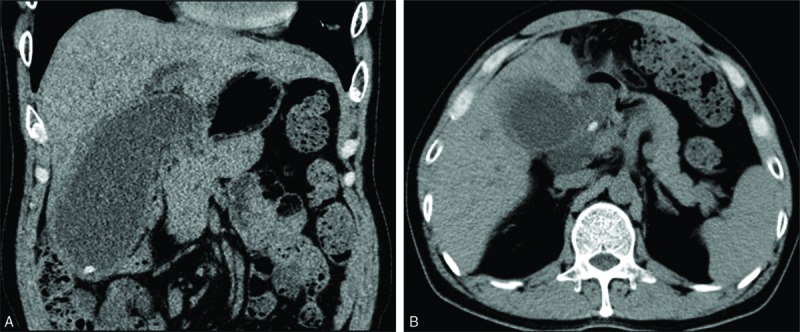
Computed tomography (CT) image showing (A) the gallbladder stone and (B) the combine bile duct stone. CT = computed tomography.
For the treatment of GB and CBD stones, the patient refused treatment using an open or laparoscopic approach because of the presence of abdominal lymph node metastases. As such, ERCP was selected as the first treatment approach. ERCP was performed by one of the specialists in our digestive system department at our hospital but failed because of the previous Billroth II procedure. Consequently, we proceeded with PTBD combined with a percutaneous transcystic approach for concurrent removal of the GS and CDB stones. Written informed consent was obtained from the patient, preoperatively.
Routine laboratory blood tests, electrocardiography, and evaluation of hepatic and renal function were completed, preoperatively. The patient completed a 4 hour fast prior to surgery. Following conscious sedation, surgery was performed under Doppler ultrasound guidance and fluoroscopic monitoring. A 21-gauge needle (Cook Medical, Bloomington) was first used to puncture the gallbladder and percutaneous cholangiography was performed through a 6-French introducer sheath (Terumo, Tokyo, Japan). Multiple positive and negative GB stones were identified. Next, a short guidewire (diameter, 0.035 inch [0.88 mm]); Terumo, Tokyo, Japan) was placed into the CBD via the cystic duct (Fig. 2A). The right hepatic duct was then punctured with a 21-gauge needle, and the biliary system was visualized by cholangiography. A short guidewire (diameter, 0.035 inch [0.88 mm]) was then inserted into the CBD through a 6-French introducer sheath through the transhepatic route. A second guidewire (length, 260 cm; diameter, 0.035 inch [0.88 mm]) was passed through the papilla and into the duodenum (Fig. 2B). A 40 × 10 mm balloon (Balt Extrusion, Montermorency, France) was advanced through the guidewire and into the duodenum. Under fluoroscopic guidance, the middle part of the balloon was placed at the sphincter (Fig. 2C), and the balloon was slowly inflated with a contrast agent to a maximum pressure of 6 to 8 atmospheres. The maximum inflation was retained for 10 to 20 s, until the waist of the balloon could no longer be seen. The balloon was partially deflated and pulled to the CBD stone and used to push the stone into the duodenum (Fig. 2D). A snare (Merit Medical, South Jordan) was then advanced through the transhepatic route to the CBD to catch and retrieve the guidewire delivered from the transcystic route, and a clear approach through the gallbladder, cystic duct, CBD, and intrahepatic bile duct was established (Fig. 2E). The cystic duct was dilated using a 40 × 18 mm balloon (Balt Extrusion, Montermorency, France) and a stone basket (Olympus, Tokyo, Japan) was advanced through the transhepatic route into the gallbladder to remove the GB stones into the CBD (Fig. 2F–H). The GB stones were pushed into the duodenum through the dilated sphincter of Oddi one by one, using the inflated balloon (Fig. 2I). Intraoperative cholangiography was performed to ensure the absence of any residual stones. Finally, two 8.5 French external drainage catheters (Cook Medical, Bloomington) were placed in the CBD and the gallbladder (Fig. 2J). On postoperative day 6, a repeat cholangiography was performed to confirm the absence of any residual stone and patency of the CBD, and the drainage catheter in the CBD was removed. The drainage catheter in the gallbladder was removed at 1-month postoperatively. A MRCP (magnetic resonance cholangiopancreatography) was performed to identify that there were no residual stones in GB and CBD (Fig. 2K). The liver function test and levels of hemoglobin and thrombocyte were monitored until the patient was fully recovered. Liver function recovered rapidly, with total bilirubin and direct bilirubin levels decreasing to normal. As well, hemoglobin and thrombocyte levels improved (Table 1), with resolution of the upper abdominal pain and jaundice.
Figure 2.
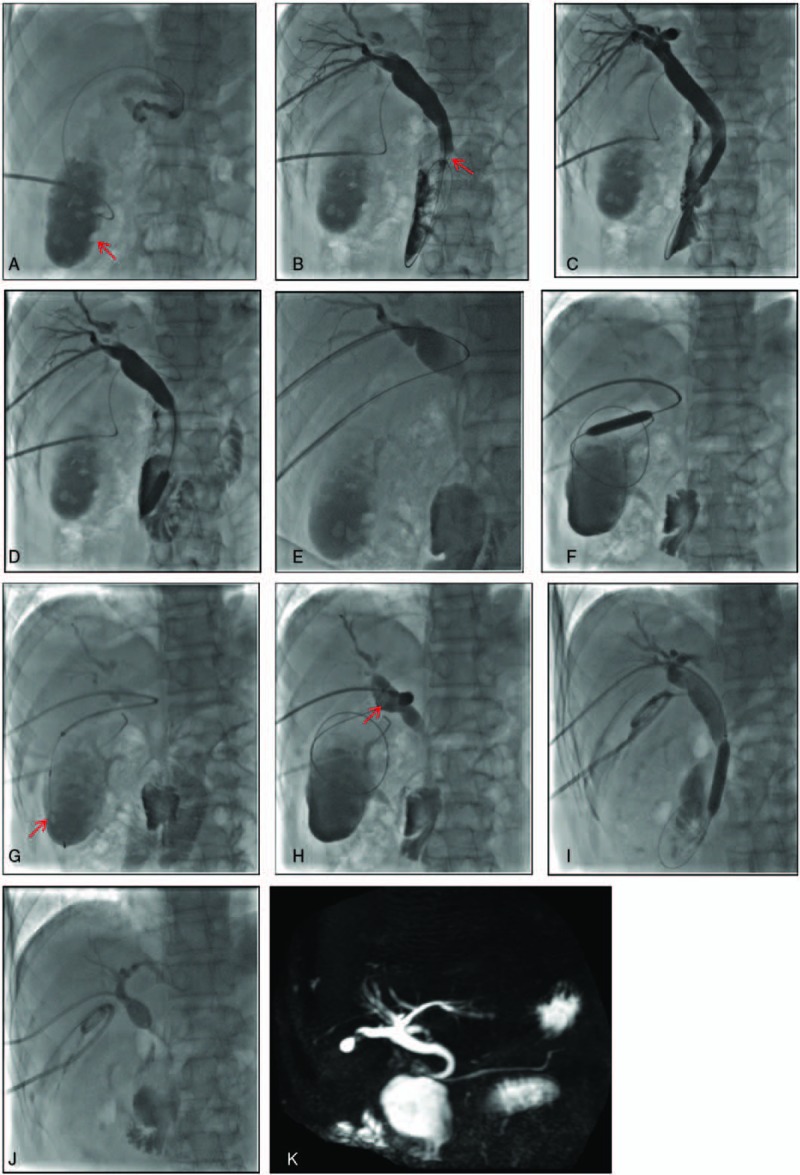
(A) Percutaneous transcystic cholangiography, showing the gallbladder stones and the guide wire, passed through the cystic duct and into the common bile duct. (B) Percutaneous transhepatic cholangiography, showing the common bile duct stone and guide wire, passed through the papilla and into the duodenum. (C) The papillary was dilated using a 40 × 10 mm balloon. (D) The common bile duct stone was pushed out into the duodenum by an inflated balloon. (E) A clear approach through the gallbladder, cystic duct, common bile duct, and intrahepatic bile duct was established. (F) The cystic duct was dilated using a 40 × 8 mm balloon. (G) A stone basket was place into the gallbladder. (H) The gallbladder stone was removed to the common bile duct and (I) pushed into the duodenum using the dilated balloon. (J) Two drainage catheters were placed in the common bile duct and the gallbladder. (K) A MRCP was performed to identify that there were no residual stones in GB and CBD.
Table 1.
Patient's laboratory findings before and after the procedure.

3. Discussion
Approximately 15% of patients with GB stones present with concurrent CBD stones.[2] Endoscopic stone removal is the preferred and most common approach for CBD stone removal in most countries.[5] Since 1974, EST has been considered as the main treatment for CBD stones in most countries.[4] For patients with concurrent GB stones, subsequent LC is considered as routine treatment.[6] In our case, the patient had a GB stone with acute cholecystitis, a CBD stone, and a history of failed endoscopic treatment caused by altered anatomy. This set of circumstances led us to develop a new innovative 1-step procedure for the concurrent removal of the GB and CBD stones.
EST has the disadvantage of requiring a sphincterotomy which leads to loss of normal papilla sphincter function, with the potential for chronic complications, such as duodeno-biliary reflux, inflammation of the biliary tree, and ampullary stenosis.[7] The use of EST is also limited in patients with a history of failed cannulation of the bile duct, a narrowed upper gastrointestinal tract, or surgically altered anatomy, as the increased length of the afferent and efferent limbs makes it difficult to reach the duodenal papilla.[4] A 19-year review of ERCP in patients with altered gastrointestinal anatomy from a single center reported a successful duodenal intubation rate of 51.9%, with failure resulting from the inability to cannulate (44%) or to identify the papilla (39.6%).[8] Percutaneous transhepatic papillary balloon dilatation is an alternative interventional radiological procedure for these cases. The technique was first reported by Staritz et al[9] in 1983. In our previous research on this procedure,[10] we reported that PTBT was associated with an overall low incidence of complications, which included: biliary tract infection (3/68 of cases), 4.4%; hemorrhage (2/68 of cases), 2.9%; and pancreatitis (1/68 of cases), 1.4% (1/68 of cases). Stones recurred in 10/68 of cases (14.7%), and reflux cholangitis occurred in 4/68 of cases (5.8%). No severe complications occurred, including gastrointestinal or biliary tract perforation or severe pancreatitis, and the technique preserved the function of the sphincter of Oddi.
Since its introduction by Dubois et al[11] in 1989, LC has become the first-choice treatment for cholecystolithiasis, replacing open surgery. Compared to open surgery, LC has the advantage of a shorter postoperative recovery and lower morbidity.[12] However, the use of LC for the treatment of acute cholecystitis is not considered routine, with debate regarding the ideal timing and its advantages over surgical management.[13] The conversion rate for delayed LC in the treatment of acute cholecystitis is higher at 51% than that for early LC at 19%.[14] Concurrent LC and laparoscopic removal is also effective and safe for the removal of CBD stones.[6] However, laparoscopic CBD exploration requires higher technical skill than transcystic stone removal.[15,16]
B-type ultrasound-guided percutaneous transcystic intervention was introduced in the early 1980s[17,18] and has since been widely accepted as an effective solution for stone removal in patients with acutely inflamed gallbladders,[19] allowing various interventional manipulations to be performed following successful negotiation of the cystic duct.[20] Gil and Eli have also reported on their successful experience of removing stones in the biliary tree through an existing gallbladder drain or T-tube, reporting a success rate of more than 90%.[21,22] The following key procedural points should be considered to ensure success. First, the patient should be placed in a supine position and the guide wire and catheter placed into the duodenum through the cystic duct, intrahepatic duct, or CBD. Second, to expand the sphincter of Oddi, the balloon should be positioned accurately and fully dilated. In principle, the diameter of the balloon should be equal to or slightly larger than the diameter of the stone. The sphincter should be dilated slowly as to prevent acute tearing of the muscle fibers. Third, in cases with multiple stones, stones should be removed one-by-one to avoid the possibility of pancreatitis caused by stone debris returning to the pancreatic duct. Fourth, a cystic drainage should be maintained in situ to reduce biliary pressure and bile leakage as a means of lowering the risk of the development of pancreatitis. Also, a gallbladder drain should be regularly retained, which also decreases biliary pressure, as well as reducing the incidence of bile leakage and pancreatitis. The main limitation of this combined approach is anatomical variations, including a very tortuous cystic duct, small-caliber cystic duct (<2 mm), the presence of Heister valves, and the lack of structural support from surrounding organs, which decrease the success rate of cannulation of the cystic duct.[23] Moreover, the size of the GB and CBD stones must be considered as an important limitation. Based on our experience and other published reports, the combined approach is recommended for GB stones with a diameter <14 mm and CBD stones <22 mm in diameter.[10,20–22]
Based on the limited evidence available, PTBD combined with a percutaneous transcystic approach may provide an alternative interventional procedure for concurrent GB and CBD stones, being of specific value for patients with previously altered gastrointestinal anatomy and acute cholecystitis.
Footnotes
Abbreviations: CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography, EST = endoscopic sphincterotomy, GB = gallbladder, LC = laparoscopic cholecystectomy, PTBD = papilla balloon dilatation.
Authorship: Surgical procedures were performed by YLL, WJW, YZW, and DL. The case and data were prepared by DL, BL, HYC, and ZL. The paper was written by DL and WW. All authors reviewed the final version.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Costi R, Gnocchi A, Di Mario F, et al. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol 2014;20:13382–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Sarli L, Lusco DR, Roncoroni L. Peroperative endoscopic sphincterotomy and laparoscopic chilecystectomy for the management of chilecystocholedocholithiasis: 10 year experience. World J Surg 2003;27:180–6. [DOI] [PubMed] [Google Scholar]
- [3].Bansal VK, Misra MC, Rajan K, et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc 2014;28:875–85. [DOI] [PubMed] [Google Scholar]
- [4].Li S, Li Y, Geng J, et al. Concurrent percutenous transhepatic papillary balloon dilatation combined with laparoscopic cholecystectomy for the treatment of gallstones with common bile duct stones. J Laparoendosc Adv Surg Tech A 2015;25:886–91. [DOI] [PubMed] [Google Scholar]
- [5].Han JY, Lee DH, Jeong S, et al. Clinical features and outcomes of endoscopic treatment for stones in stemware-shaped common bile ducts: a multicenter data analysis. Gut Liver 2015;9:800–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Boerma D, Schwartz MP. Management of common bile-duct stones and associated gallbladder stones: surgical aspects. Best Pract Res Clin Gastroenterol 2006;20:1103–16. [DOI] [PubMed] [Google Scholar]
- [7].Bergman JJ, Rauws EA, Fockens P, et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bile duct stones. Lancet 1997;349:1124–9. [DOI] [PubMed] [Google Scholar]
- [8].Ruiz CP, Hervás MA, Muñoz GB, et al. Endoscopic retrograde cholangiopancreatography in patients with anatomic abnormalities of the stomach due to surgery. Gastroenterol Hepatol 2013;36:609–15. [DOI] [PubMed] [Google Scholar]
- [9].Staritz M, Ewe K, zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment for common bile duct stones and papillary stenosis. Endoscopy 1983;15:197–8. [DOI] [PubMed] [Google Scholar]
- [10].Li YL, Geng JL, Jia YM, et al. Clinical study of percutaneous transhepatic balloon dilation: a novel procedure for common bile duct stone. Natl Med J 2013;93:3586–9. [PubMed] [Google Scholar]
- [11].Dubois F, Berthelot G, Lavard H. Cholecystectomy by coelioscopy. Presse Med 1989;18:980–2. [PubMed] [Google Scholar]
- [12].Shea JA, Healey MJ, Berlin JA, et al. Mortality and complications associated with laparoscopic cholecystectomy: a meta-analysis. Ann Surg 1996;224:609–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yuichi Y, Tadahiro T, Kawarada Y, et al. Surgical treatment of the patient with acute cholecystitis: Tokyo Guidelines. J Hepato-Biliary Pan 2007;14:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kullman E, Borch K, Svanvik J, et al. Differences in outcome of acute and elective laparoscopic cholecystectomy. Digestive Surg 1997;14:398–403. [Google Scholar]
- [15].Martin IJ, Baily IS, Rhodes M, et al. Toward T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg 1998;228:29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Thompson E, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg 2002;89:1608–12. [DOI] [PubMed] [Google Scholar]
- [17].Elyaderani M, Gabriele OF. Percutaneous cholecystostomy and cholangiography in patients with obstructive jaundice. Radiology 1979;130:601–2. [DOI] [PubMed] [Google Scholar]
- [18].Shaver RW, Hawkins IF, Soong J. Percutaneous cholecystostomy. AJR Am J Roentgenol 1982;138:1133–6. [DOI] [PubMed] [Google Scholar]
- [19].Hatzidakis AA, Prassopoulos P, Petinarakis I, et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol 2002;12:1778–84. [DOI] [PubMed] [Google Scholar]
- [20].Hatzidakis A, Venetucci P, Krokidis M, et al. Percutaneous biliary interventions through the gallbladder and the cystic duct: what radiologists need to know. Clin Radiol 2014;69:1304–11. [DOI] [PubMed] [Google Scholar]
- [21].Gil S, de la Iglesia P, Verdú JF. Effectiveness and safety of balloon dilation of the papilla and the useof an occlusion balloon for clearance of bile duct calculi. AJR 2000;174:1455–60. [DOI] [PubMed] [Google Scholar]
- [22].Eli A, Chaim N, Eduard R. Percutaneous trans-papillary elimination of common bile duct stones using an existing gallbladder drain for access. IMAJ 2012;14:354–8. [PubMed] [Google Scholar]
- [23].Yasumoto T, Yokoyama S, Nagaike K. Percutaneous transcholecystic metallic stent placement for malignant obstruction of the common bile duct: preliminary clinical evaluation. Vasc Interv Radiol 2010;21:252–8. [DOI] [PubMed] [Google Scholar]


