Abstract
Aim:
The aim of the study was to measure patient’s satisfaction level and acceptance of conscious sedation as a method of pain relief following transvaginal oocyte retrieval (TVOR) during assisted reproduction technology treatment. We also evaluated the factors that may influence the efficacy of conscious sedation method.
Setting and Design:
A prospective cross-sectional study.
Materials and Methods:
Prospective study was conducted from October 2015 to January 2016 at a university-level hospital and 100 women were recruited. Variables for analysis included woman age, duration of procedure, number of oocytes retrieved, and transmyometrial passage of the needle. Pain assessment was done by visual analog scale (VAS). Medical complications, and patient satisfaction score [Likert’s score and client satisfaction questionnaire (CSQ)] were recorded.
Results:
There was a moderate positive correlation between age and pain score on day 1 post-procedure. When the duration of procedure was >12 min, immediate post-procedure pain score was significantly higher compared to those whose procedure where duration was <12 min. There was no correlation between pain score and the number of oocytes retrieved (≤5, 6–15, and ≥16) and transmyometrial passage of needle. The VAS 10-point score immediately post-procedure, after 6 and 24 h post-procedure, and on day of embryo transfer was 2.83 (±1.67), 0.78 (±1.04), 0.39 (±1.09), and 0.14 (±0.58), respectively. The Likert’s score was 3.65 (±0.82) and mean CSQ was 27.04 (±3.01). Majority of the women (86%) preferred the same pain relief method for future analgesia. There were no major complications.
Conclusion:
Conscious sedation was associated with high satisfaction level and acceptance rate among patients undergoing TVOR.
KEYWORDS: Conscious sedation, pain relief, transvaginal oocyte retrieval
INTRODUCTION
Surgical retrieval of oocytes from the ovary is an important step in an in vitro fertilization (IVF) treatment. Initially, oocyte retrieval was done laparoscopically and involved general anesthesia.[1] However, with the introduction of transvaginal ultrasound guided oocyte retrieval, the procedure became less invasive, shorter in duration, and technically less challenging compared to the earlier laparoscopic approach.[2,3,4] Ultrasound guided aspiration also meant alternative methods of pain relief could be employed instead of general anesthesia.
Transvaginal oocyte retrieval (TVOR) is relatively painful and usually performed as a day care procedure. Pain during the oocyte retrieval is mainly caused by puncture of vaginal skin, ovarian capsule, and manipulation of the ovaries during the procedure.[5] Various options are available for pain relief during TVOR and they include general anesthesia,[6] regional anesthesia,[7,8,9] and conscious sedation.[10] Conscious sedation is administered alone or in combination with paracervical block or acupuncture.[5]
Conscious sedation involves depressing level of consciousness minimally, whereas the patient is able to maintain airway patency independently and respond to physical stimulation or verbal commands.[11] It does not require highly specialized equipment and can be administered by trained personal under physician’s supervision.[10] Commonly opioids and benzodiazepines are used for their analgesic and sedative properties, respectively. Benzodiazepines also have amnestic effects.
Women have different coping strategies for pain and perception of pain depends on sociocultural factors of the individual. An earlier study evaluated experiences of women undergoing TVOR under conscious sedation and found high satisfaction levels and acceptance among the included women.[12]
We decided to measure patient satisfaction and acceptance level of conscious sedation method for pain relief and also determine the factors which may influence its efficacy.
MATERIALS AND METHODS
Infertile women undergoing assisted reproduction technology treatment for any etiology at our unit were invited to participate in our study. Those who were willing were recruited in the study after getting a written informed consent. The study was cross-sectional in design and conducted between October 2015 and January 2016. Ethics approval was taken from the institutional review board.
We included the following:
Women undergoing conventional IVF and willing to participate in the study.
We excluded the following:
Women who were not willing to participate or who were to receive general anesthesia.
Women whose body mass index was more than 35 kg/m2.
Women who were allergic to Pethidine, Benzodiazepines, or Fentanyl.
Primary outcome of the trial was pain relief as measured by visual analog scale (VAS), immediate post-procedure, 6 and 24 h post-procedure (next day after procedure), and on the day of embryo transfer. The secondary outcomes included the following: incidence of perioperative complications, such as hypotension (blood pressure <90/60 mmHg), bradycardia (pulse rate <60/min), and respiratory depression (respiratory rate <12/min; Oxygen saturation <90%), side effects of analgesia, patient satisfaction score [Likert’s score and client satisfaction questionnaire (CSQ)], and clinical pregnancy rate per embryo transfer.
Protocol
For women who were planned for TVOR, a basic health assessment was done which included medical history and physical examination (including reference to allergies), current medication use, and screening for medical comorbidities. Blood count, sugars, thyroid hormone, and viral screening status were noted. Instructions about diet and overnight fasting were given before procedure. Written informed consent was taken from couple before the procedure.
Sample protocol used for conscious sedation in patients undergoing transvaginal follicle aspiration was as follows:
Intravenous (IV) access was secured.
In the procedure room, a blood pressure and pulse oximeter monitoring was started just prior to sedation.
Oxygen inhalation was given at 3 l/min with face mask.
Inj. Pethidine (Pethidine Hcl; Haffkine Bio Pharmaceuticals Corporation Ltd, Mumbai, Maharashtra, India) 0.5 to 1 mg/kg was given slow IV. Initial loading dose of 20 to 40 mgs IV was given depending upon patient weight, anticipated duration of procedure, and presence of pelvic adhesions.
Inj. Midazolam (Midosed; Sun Pharmaceuticals, Mumbai, Maharashtra, India) 0.01 to 0.03 mg/kg slow IV was given.
Inj. Fentanyl (Fendrop, Sun Pharmaceuticals) 1 to 2 μg/kg slow IV was given only if required.
Local preovarian block was given with Inj. Lignocaine (Xylocaine; Astra Zeneca Pharma India Limited, Bangalore, India) 10 ml of 1%. Approximately 5 ml of Inj Lignocaine was injected on both sides using a 16-G sterile IVF ovum pick up needle (Cook Australia, Queensland, Australia) between vaginal wall and peritoneal surface close to the ovary where the follicle aspiration needle was to be inserted.[13]
Diclofenac (Jonac; German Remedies Private Limited, Mumbai, Maharashtra, India) suppository 50 mg was inserted per rectal post-procedure.
Continuous monitoring of oxygen saturation and vitals was done during procedure and post-procedure period in the recovery room for 30 min and subsequently, at 1 and 6 h. Once the patient was ambulatory with stable vital parameters and was able to tolerate soft diet, she was discharged.
Patients were interviewed before discharge. The pain score was assessed by VAS during immediate postoperative period, 6 and 24 h, and then on the day of embryo transfer and overall satisfaction score based on Likert’s scale was also completed. A CSQ was also filled on the day of TVOR.
VAS is a measurement instrument that is used to measure the amount of pain that a patient feels ranging across a continuum from none to an extreme amount of pain.[14] The patient marks on the line the point that they feel represents their perception of their current state. In a 10-point VAS scoring: 0 indicates no pain, 1 to 3 indicates mild pain, 4 to 6 indicates moderate pain, and 7 to 10 indicates severe pain.
A Likert’s scale is a psychometric scale commonly used in research and employs questionnaire. It combines the responses from the series of questions to create an attitudinal measurement scale. In a commonly used 5-point Likert’s satisfaction scale format: 1-poor, 2-fair, 3-satisfactory, 4-very good, and 5-excellent.
Satisfaction is an important indicator of the quality of care. The CSQ-8 has eight question-items (quality of service, kind of service, met needs, recommend to a friend, amount of help, deal with problems, overall satisfaction, and return back). Their responses are scored from 1 to 4, and thus the possible total scores range from 8 to 32. Higher scores indicate greater satisfaction. Reliability testing and validation testing of the CSQ-8 have been done in clinical scenario dealing with mental health.[15] We have incorporated this additional method to measure the satisfaction with overall care involved during TVOR which is closely linked to pain relief and subsequent inpatient care.
Sample size calculation
An earlier study in which VAS 100-point scoring system was used to assess pain, the mean pain score reported was 38.38 (±19.97).[12] Assuming a mean pain score of 38, a standard deviation of 20, a total of 64 women were required to obtain a 95% confidence interval with a precision 5 around an average pain estimate. We decided to recruit total of 100 women for our study.
All study variables were described using summary statistics. Continuous variables were summarized with means and standard deviations, if normally distributed. For variables with skewed distributions, median with interquartile ranges were calculated. Frequencies with percentages were used to describe the categorical variables. Relationship between continuous variables and pain scores were assessed using spearman’s correlation coefficient. Pain levels were associated with other categorical factors across time points using Wilcoxan rank sum tests. All analysis was performed using STATA 13.0 (StataCorp, College Station, Texas, USA).
RESULTS
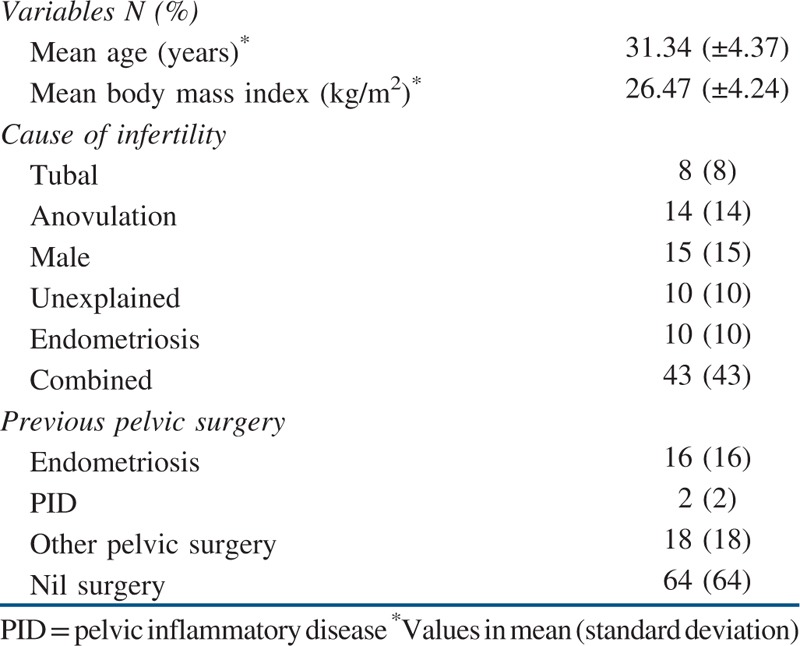
A total of 100 women were recruited in our study and were available for final analysis. The patient’s clinical characteristics are shown in [Table 1].
Table 1.
Clinical characteristics
The median number of oocytes retrieved were 7.5 (interquartile range: 4–11) and the mean duration of the TVOR was 11.86 (±3.36) min as shown in Table 2. Mean dose of Pethidine used was 22.1 mg (±4.78) and all the patients received starting dose of 0.5 mg of Midazolam uniformly. None of the patients received Fentanyl. During TVOR, the needle traversed the uterus in 12 (12%) women.
Table 2.
Procedure related variables
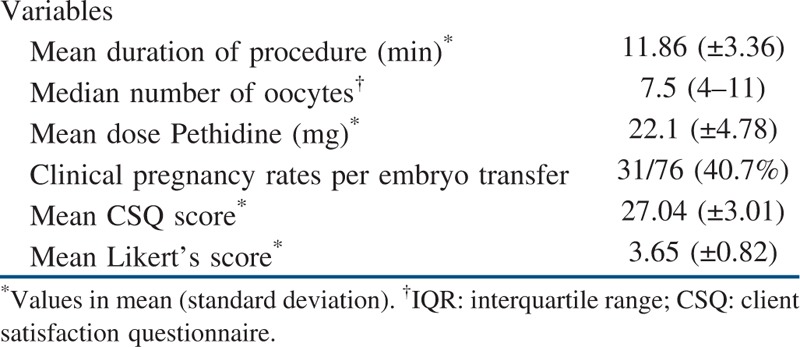
None of the women had hypotension, respiratory depression, or vomiting; though six (6%) of them had transient bradycardia which recovered after atropine administration. Two women had anterograde amnesia (2%). The clinical pregnancy rate per embryo transfer was 40.7% (31/76). Remaining 24 women did not undergo fresh transfer.
The VAS 10-point score immediately post-procedure, after 6 and 24 h post-procedure, and on day of embryo transfer was 2.83 (±1.67), 0.78 (±1.04), 0.39 (±1.09), and 0.14 (±0.58), respectively. The Likert’s score was 3.65 (±0.82) and mean CSQ was 27.04 (±3.01).
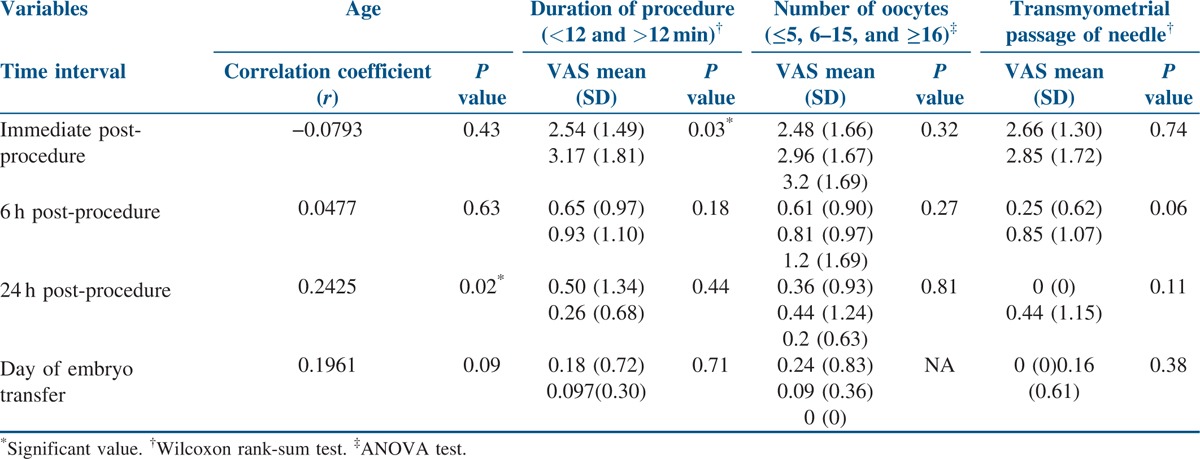
There was a moderate positive correlation between age and pain score on day 1 post-procedure. When the duration of procedure was more than 12 min, immediate post-procedure pain score was significantly higher compared to those whose procedure duration was less than 12 min. However, there was no correlation of duration of procedure with pain score after 6 and 24 h post-procedure and on the day of embryo transfer. There was no correlation between pain score and the number of oocytes retrieved (≤5, 6–15, and ≥16) across all the four-time intervals when the pain score was measured. Similarly, transmyometrial passage of TVOR needle also did not correlate with pain score across all the time intervals [Table 3].
Table 3.
Variables and its association with pain score
Preference for future analgesia was recorded at immediate post-procedure and on the day of embryo transfer. Majority of the women (86%) preferred the same method for future analgesia. There was a significant correlation in patient’s acceptance of future analgesia and pain score in immediate post-procedure period. Those with higher pain score desired for better method of analgesia in future. However, this correlation was no longer significant when the question was asked again on day of embryo transfer.
DISCUSSION
We found high patient satisfaction level with mean Likert’s score ranging between satisfactory to very good. Acceptance rate for the method was also high with majority of the patients (86%) preferring the same method of pain relief for future as well. No major complications were recorded during the study. The pain score were significantly higher immediately post-procedure for those women whose duration of TVOR exceeded 12 min, whereas it did not have any significant correlation with number of oocytes retrieved or transmyometrial passage of needle. There was a significant correlation in patient’s acceptance of future analgesia and pain score in immediate post-procedure period though it was no longer significant on the embryo transfer.
Among the strength of our study was its prospective design and adequate sample size. Apart from objective assessment of pain, we also measured patient satisfaction level which is an important patient centric outcome. One of the limitations of the study was lack of control arm. The subjective nature of pain and satisfaction limit our ability to get a truly objective assessment of the pain relief method.
We found significant association of pain score with duration of procedure in the immediately post-procedure though it was no longer significant across the remaining time period. Our finding is contrary to earlier study which did not find any association with duration, age, educational level, number of follicles retrieved, or transmyometrial retrieval.[12] The reason for the contrary finding could be due to multiple intervals the pain score was measured in our study compared to earlier study which included measurement only once. Similarly, those who preferred another method of analgesia in future had significantly higher pain score and understandably wished to change the current method. This finding was in agreement with finding of an earlier study which found significant correlation between patient’s pain experience and future preference for pain relief method.[12] Although we found significantly higher pain score on day 1 post-procedure with regards to age, the correlation was only moderate and hence may not be clinically significant observation.
One of the earlier randomized trials, comparing conscious sedation using Midazolam and Ketamine with general anesthesia using Propofol, found similar patient satisfaction and clinical pregnancy rates in both the groups.[16] A Cochrane review which included 21 trials comparing different methods of pain relief during TVOR, such as general anesthesia, regional anesthesia, conscious sedation alone or in combination with paracervical block, and patient versus physician, controlled analgesia. The review did not find one particular modality of pain relief better than other and overall satisfaction level was high among women irrespective of the pain relief method used during TVOR. The optimal method could be decided depending upon the women and clinicians preferences with resource availability being another important factor.[5]
Among the conscious sedation methods, there is paucity of trials comparing various combinations of drugs used. In a recent Cochrane review, only four studies were identified that compared the different drug regimens for conscious sedation. There was no evidence of difference in pain relief between Midazolam combined with Fentanyl compared to Propofol with Fentanyl, but the former was associated with less nausea and vomiting.[5]
Survey in United Kingdom and other countries have shown differential levels of acceptance for conscious sedation for TVOR varying between 48 and 95%.[6,11,17] As an anesthetist or specialized equipments are not routinely required while using this protocol, it is useful method in a low resource setting.[10] However, the equipments for intubation should be kept in the theater and anesthetist or person trained in performing intubation should be available on a short notice. Majority of the women in our study were satisfied with the pain relief method as suggested by high Likert’s and CSQ score. Out of 100 women, 86 preferred the current method of conscious sedation as an option for future analgesia which is comparable to finding of earlier study where 94% women felt the same.[12]
We found the conscious sedation using Midazolam and Pethidine along with preovarian block acceptable and safe method of pain relief. The patient’s experiences from our study can be used to for counseling purposes prior to TVOR. There is a need for conducting well powered trial comparing various methods of conscious sedation to determine the most cost-effective combination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tanbo T, Henriksen T, Magnus O, Abyholm T. Oocyte retrieval in an IVF program. A comparison of laparoscopic and vaginal ultrasound-guided follicular puncture. Acta Obstet Gynecol Scand. 1988;67:243–6. doi: 10.3109/00016348809004213. [DOI] [PubMed] [Google Scholar]
- 2.Gleicher N, Friberg J, Fullan N, Giglia RV, Mayden K, Kesky T, et al. Egg retrieval for in vitro fertilisation by sonographically controlled vaginal culdocentesis. Lancet. 1983;2:508–9. doi: 10.1016/s0140-6736(83)90530-5. [DOI] [PubMed] [Google Scholar]
- 3.Wikland M, Enk L, Hamberger L. Transvesical and transvaginal approaches for the aspiration of follicles by use of ultrasound. Ann N Y Acad Sci. 1985;442:182–94. doi: 10.1111/j.1749-6632.1985.tb37519.x. [DOI] [PubMed] [Google Scholar]
- 4.el Hussein E, Balen AH, Tan SL. A prospective study comparing the outcome of oocytes retrieved in the aspirate with those retrieved in the flush during transvaginal ultrasound directed oocyte recovery for in-vitro fertilization. Br J Obstet Gynaecol. 1992;99:841–4. doi: 10.1111/j.1471-0528.1992.tb14417.x. [DOI] [PubMed] [Google Scholar]
- 5.Kwan I, Bhattacharya S, Knox F, McNeil A. Pain relief for women undergoing oocyte retrieval for assisted reproduction. Cochrane Database Syst Rev. 2013:CD004829. doi: 10.1002/14651858.CD004829.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Elkington NM, Kehoe J, Acharya U. Intravenous sedation in assisted conception units: a UK survey. Hum Fertil (Camb) 2003;6:74–6. doi: 10.1080/1464770312331369083. [DOI] [PubMed] [Google Scholar]
- 7.Lefebvre G, Vauthier D, Seebacher J, Henry M, Thormann F, Darbois Y. In vitro fertilization: a comparative study of cleavage rates under epidural and general anesthesia—interest for gamete intrafallopian transfer. J In Vitro Fert Embryo Transf. 1988;5:305–6. doi: 10.1007/BF01132185. [DOI] [PubMed] [Google Scholar]
- 8.Hayes MF, Sacco AG, Savoy-Moore RT, Magyar DM, Endler GC, Moghissi KS. Effect of general anesthesia on fertilization and cleavage of human oocytes in vitro. Fertil Steril. 1987;48:975–81. doi: 10.1016/s0015-0282(16)59594-6. [DOI] [PubMed] [Google Scholar]
- 9.Gonen O, Shulman A, Ghetler Y, Shapiro A, Judeiken R, Beyth Y, et al. The impact of different types of anesthesia on in vitro fertilization embryo transfer treatment outcome. J Assist Reprod Genet. 1995;12:678–82. doi: 10.1007/BF02212892. [DOI] [PubMed] [Google Scholar]
- 10.Trout SW, Vallerand AH, Kemmann E. Conscious sedation for in vitro fertilization. Fertil Steril. 1998;69:799–808. doi: 10.1016/s0015-0282(98)00031-4. [DOI] [PubMed] [Google Scholar]
- 11.Ditkoff EC, Plumb J, Selick A, Sauer MV. Anesthesia practices in the United States common to in vitro fertilization (IVF) centers. J Assist Reprod Genet. 1997;14:145–7. doi: 10.1007/BF02766130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiebai PO, Ogunmokun AA, Ajayi RA. Experience with conscious sedation for oocyte retrieval in Nigeria. Afr J Reprod Health. 2008;12:30–4. [PubMed] [Google Scholar]
- 13.Cerne A, Bergh C, Borg K, Ek I, Gejervall AL, Hillensjö T, et al. Pre-ovarian block versus paracervical block for oocyte retrieval. Hum Reprod. 2006;219110:2916–21. doi: 10.1093/humrep/del271. [DOI] [PubMed] [Google Scholar]
- 14.Kuhlmann T, Dantlgraber M, Reips UD. Investigating measurement equivalence of visual analogue scales and Likert-type scales in Internet-based personality questionnaires. Behav Res Methods 2017. doi: 10.3758/s13428-016-0850-x. Article in press. [DOI] [PubMed] [Google Scholar]
- 15.Matsubara C, Green J, Astorga LT, Daya EL, Jervoso HC, Gonzaga EM, et al. Reliability tests and validation tests of the client satisfaction questionnaire (CSQ-8) as an index of satisfaction with childbirth-related care among Filipino women. BMC Pregnancy Childbirth. 2013;13:235. doi: 10.1186/1471-2393-13-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ben-Shlomo I, Moskovich R, Katz Y, Shalev E. Midazolam/Ketamine sedative combination compared with fentanyl/propofol/isoflurane anaesthesia for oocyte retrieval. Hum Reprod. 1999;14:1757–9. doi: 10.1093/humrep/14.7.1757. [DOI] [PubMed] [Google Scholar]
- 17.Bokhari A, Pollard BJ. Anaesthesia for assisted conception: a survey of UK practice. Eur J Anaesthesiol. 1999;16:225–30. doi: 10.1046/j.1365-2346.1999.00461.x. [DOI] [PubMed] [Google Scholar]


