Abstract
Background
The syphilis diagnostic algorithms applied in different countries vary significantly depending on the local syphilis epidemiology and other considerations, including the expected workload, the need for automation in the laboratory and budget factors. This study was performed to investigate the efficacy of traditional and reverse syphilis diagnostic algorithms during general health checkups.
Methods
In total, 1,000 blood specimens were obtained from 908 men and 92 women during their regular health checkups. Traditional screening and reverse screening were applied to the same specimens using automatic rapid plasma regain (RPR) and Treponema pallidum latex agglutination (TPLA) tests, respectively. Specimens that were reverse algorithm (TPLA) reactive, were subjected to a second treponemal test performed by using the chemiluminescent microparticle immunoassay (CMIA).
Results
Of the 1,000 specimens tested, 68 (6.8%) were reactive by reverse screening (TPLA) compared with 11 (1.1%) by traditional screening (RPR). The traditional algorithm failed to detect 48 specimens [TPLA(+)/RPR(−)/CMIA(+)]. The median TPLA cutoff index (COI) was higher in CMIA-reactive cases than in CMIA-nonreactive cases (90.5 vs 12.5 U).
Conclusions
The reverse screening algorithm could detect the subjects with possible latent syphilis who were not detected by the traditional algorithm. Those individuals could be provided with opportunities for evaluating syphilis during their health checkups. The COI values of the initial TPLA test may be helpful in excluding false-positive TPLA test results in the reverse algorithm.
Keywords: Syphilis, Treponema pallidum, Rapid plasma regain (RPR), Treponema pallidum latex agglutination, Chemiluminescent microparticle immunoassay, Algorithm
INTRODUCTION
Syphilis is a sexually transmitted infection caused by Treponema pallidum that can be transmitted from an infected mother to her fetus or through a blood transfusion. The identification and control of this venereal disease using screening tests have become a public health priority aimed at preventing pregnancy loss and congenital malformations and reducing the increased risk of HIV infection [1,2].
Because T. pallidum cannot be detected by conventional laboratory stains and requires in vivo culturing, serologic tests are critically important for detecting the bacteria. Two algorithms (traditional and reverse) are currently used as the principal diagnostic methods [3,4]. Traditionally, syphilis screening is first performed with a non-treponemal test, such as the rapid plasma regain (RPR) or venereal disease research laboratory (VDRL) test, and the result is then confirmed using a treponemal test [5]. This sequence of tests is sometimes reversed, whereby screening commences with a treponemal assay, followed by a non-treponemal assay. In cases with positive treponemal test results and negative non-treponemal test results, a second and different treponemal assay needs to be performed to resolve the discordant results [6].
The diagnostic algorithms for syphilis vary significantly depending not only on the local epidemiology of syphilis, but also on other considerations, such as the workload, the need for automation in the laboratory, and budget factors. Several studies have been reported regarding the comparison of these diagnostic algorithms for syphilis [6,7,8,9]. Most of them recruited subjects from university hospitals, which might include more patients than the number of patients among subjects taking general health checkup. Furthermore, qualitative immunoassays were used as primary treponemal screening tests for reverse algorithm in their studies. In recent years, automated quantitative turbidimetric assays have been used to detect non-specific and specific antibodies for T. pallidum in laboratories.
Therefore, this study was performed to investigate the efficacy of the traditional and reverse syphilis diagnostic algorithms for the subjects taking health checkups, by using automatic RPR test and Treponema pallidum latex agglutination (TPLA) test, respectively.
METHODS
1. Study subjects and T. pallidum screening
The RPR test was performed as a screening test for syphilis at Health Promotion Center of Korea Association of Health Promotion, Seoul, Korea. One thousand blood specimens were obtained from 908 men and 92 women (range of age: 21–84 yr) who underwent syphilis testing during their regular health checkups from June 2016 to August 2016. Traditional screening and reverse screening were applied to the same specimens using the HiSense Auto RPR LTIA kit (HBi Co, Anyang, Korea) and the AutoLab TPLA kit (IVD-TPLA, IVDLab Co, Anyang, Korea), respectively, on a Hitachi 7600 system (Roche, New York, NY, USA). The RPR and TPLA cutoff indexes (COI) were 1.0 and 10 U, respectively; specimens with COI values of <1.0 and <10 U, respectively, were considered nonreactive.
Specimens that were TPLA screening reactive were tested by using the Architect syphilis treponemal assay (Abbott Diagnostics, Tokyo, Japan), which is a chemiluminescent microparticle immunoassay (CMIA) for the qualitative detection of T. pallidum antibodies in the ARCHITECT i System. Specimens with signal-to-cutoff (S/CO) values of <1.0 are considered nonreactive according to the Architect syphilis treponemal assay. The fluorescent treponemal antibody absorption (FTA-ABS) test (Zeus Scientific, Branchburg, NJ, USA) was applied to specimens with discordant treponemal test results and those with discordant traditional and reverse screening results. All testing was performed according to the manufacturers' recommendations.
2. The optimal COI for syphilis screening by TPLA in reverse algorithm
ROC curve was analyzed to identify the optimal COI for TPLA and calculate the area under the ROC curve (AUROC).
3. Data analysis
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). The percentage of agreement and the kappa (κ) coefficient were calculated to determine the agreement between the traditional algorithm and the reverse algorithm. The χ2 test was used to compare proportions. Student's test was used to compare mean values, and the Wilcoxon test was used to compare continuous variables that did not conform to a normal distribution. ROC curve was analyzed to identify the optimal COI of TPLA for syphilis screening. Sensitivity, specificity, and positive and negative predictive values (PPV, NPV) were calculated with 95% confidence intervals (CI). A P value of <0.05 was considered statistically significant.
This study was approved by the institutional review board of the Korea Association of Health Promotion (130750-2016011-HR-025).
RESULTS
1. Comparison of the traditional and reverse algorithms
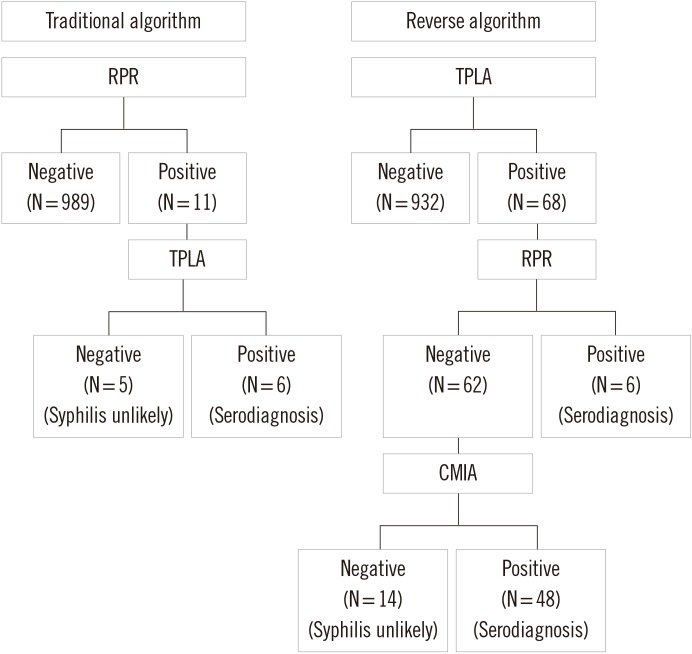
Of the 1,000 specimens tested, 68 (6.8%) and 11 (1.1%) were reactive using reverse screening (TPLA) and traditional screening (RPR), respectively. Six of the 11 RPR-reactive specimens were confirmed as positive by TPLA. The five nonreactive specimens (0.5%) were interpreted as biological false reactive. In addition to the six traditional algorithm-reactive specimens, another 62 specimens not detected by the traditional algorithm were reactive on the basis of reverse sequence screening. Forty-eight of these 62 specimens were serologically confirmed as syphilis by using a second treponemal test (CMIA). The corresponding κ value of the traditional algorithm vs the reverse algorithm was 0.191 (95% CI=0.060–0.322), which indicates a slight agreement between the traditional and reverse algorithms (Table 1, Fig. 1).
Table 1. Comparison of the traditional and reverse algorithms.
| Reverse algorithms | Traditional algorithms | Total | Agreement (%) | Kappa value (95% CI) | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Positive | 6 | 48 | 54 | 11.1 (6/54) | 0.191 (0.060–0.322) |
| Negative | - | 946 | 946 | 100 (946/946) | |
| Total | 6 | 994 | 1,000 | 95.2 (952/1,000) | |
Abbreviation: CI, confidence interval.
Fig. 1. Traditional and Reverse algorithms for syphilis diagnosis.
Abbreviations: TPLA, Treponema pallidum latex agglutination; RPR, rapid plasma regain; CMIA, chemiluminescent microparticle immunoassay.
2. Analysis of results not identified by using the traditional (RPR) screening method [TPLA(+)/RPR(-)]
Forty-eight of the 62 TPLA reactive and RPR-nonreactive specimens were reactive by CMIA, while the remaining 14 specimens (1.4%) were not reactive by CMIA; these were interpreted as false reactive in the TPLA test. Of these 48 specimens, 44 were reactive by using FTA-ABS IgG. The CMIA S/CO values of the four remaining non-reactive specimens ranged from 1.16 to 4.16. A manual RPR test was performed on 17 specimens selected randomly from the 48 specimens [TPLA(+)/RPR(-)/CMIA(+)]. The test results for these specimens were all nonreactive (data not shown).
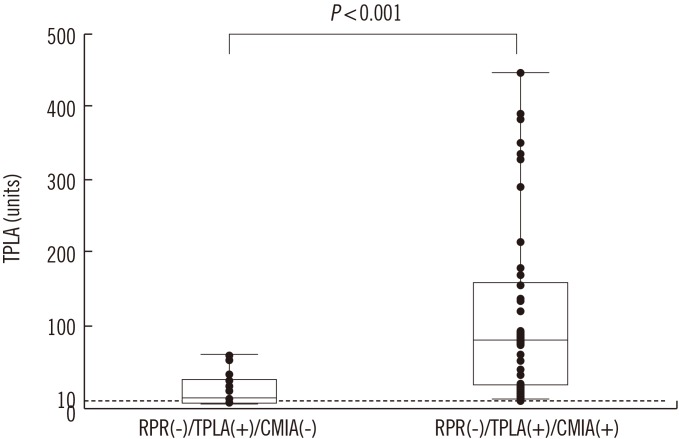
3. Comparison of true-reactive TPLA results [TPLA(+)/RPR(-)/CMIA(+)] and false-reactive TPLA results [TPLA(+)/RPR(-)/CMIA(-)]
The TPLA values differed between CMIA-reactive and CMIA-nonreactive specimens (Table 2, Fig. 2). The median TPLA COI for CMIA-reactive specimens was higher than that for CMIA-nonreactive ones (90.5 vs 12.5 U). Eight (57.2%) of the 14 CMIA-nonreactive specimens had TPLA values below 20 U, with a range of 10–45 U. In contrast, three (6.3%) of the 48 CMIA-reactive specimens had TPLA values below 20 U, with a range of 12–449 U. Twelve of the 14 false-reactive TPLA results [TPLA(+)/RPR(-)/CMIA(-)] were confirmed as nonreactive by using FTA-ABS. The remaining two specimens were weakly reactive with the FTA-ABS test, which could be interpreted as false non-reactives in the CMIA test.
Table 2. Characteristics of subjects with discordant syphilis serology [TPLA(+)/RPR(-)] according to CMIA status in the reverse syphilis screening algorithm.
| Variables | TPLA(+)/RPR(−)/CMIA(+) (N = 48) | TPLA(+)/RPR(−)/CMIA(−) (N = 14) | P values |
|---|---|---|---|
| Age (yr) | 0.023 | ||
| Median | 58 | 44.0 | |
| Range | (23-84) | (21-77) | |
| Sex | 0.389 | ||
| Male, N (%) | 44 (91.7) | 10 (83.3) | |
| Female, N (%) | 4 (8.3) | 2 (16.7) | |
| TPLA (U) | 0.000 | ||
| Median | 90.5 | 12.5 | |
| Range | (12.0-449.0) | (10.0-45.0) | |
| CMIA (S/CO) | 0.000 | ||
| Median | 8.635 | 0.135 | |
| Range | (1.12-30.88) | (0.04-0.69) | |
| FTA-ABS IgG | 0.000 | ||
| Negative, N (%) | 4 (8.3) | 12 (85.7) | |
| Positive, N (%) | 44 (91.7) | 2 (14.3)* |
*weakly reactive to FTA-ABS.
Abbreviations: TPLA, Treponema pallidum latex agglutination; RPR, rapid plasma regain; CMIA, chemiluminescent microparticle immunoassay; S/CO, signal-to-cutoff ratio; FTA-ABS, fluorescent treponemal antibody absorption.
Fig. 2. Comparison of the quantitative results of TPLA between true reactive TPLA [TPLA(+)/RPR(-)/CMIA(+)] and false reactive TPLA [TPLA(+)/RPR(-)/CMIA(-)] cases in the reverse algorithm. Dotted line represents the cutoff index of TPLA test.
Abbreviations: TPLA, Treponema pallidum latex agglutination; RPR, rapid plasma regain; CMIA, chemiluminescent microparticle immunoassay.
4. The optimal cutoff index (COI) for syphilis screening by TPLA
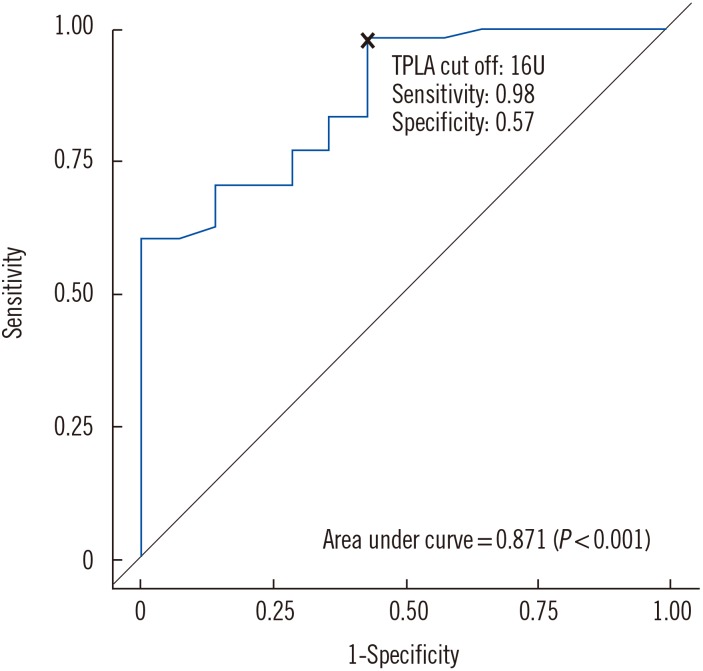
The AUROC for syphilis screening was 0.871 (P<0.001). The optimal COI for syphilis screening by TPLA was 16 U, which had a sensitivity of 0.98 (95% CI, 0.94 1.00), specificity of 0.57 (95% CI, 0.31–0.83), NPV of 0.889 (95% CI, 0.684–1.0), and PPV of 0.887 (95% CI, 0.801–0.972) (Fig. 3).
Fig. 3. Area under the receiver operator curve of TPLA for syphilis screening.
Abbreviation: TPLA, Treponema pallidum latex agglutination.
DISCUSSION
The results of this study indicate that the positivity rate of the reverse syphilis screening algorithm was higher than that of the traditional syphilis screening algorithm. The proportion of subjects with TPLA-reactive serology in this study (6.8%) was lower than the positivity rates detected in a Treponema pallidum particle agglutination (TPPA)-based screen (11.4%) involving patients at a Chinese university hospital [7], but higher than the proportion determined in a chemiluminescent immunoassay (CIA)-based screen (2%) involving individuals from a large integrated health-care system in the USA [8], as well as that determined in an IgG multiplex flow immunoassay (MFI)-based screen (1.5%) involving individuals who underwent routine syphilis tests at the Mayo Clinic [9]. These differences in positivity rates for syphilis reverse screening may be attributable to differences in the epidemiology of syphilis and false-positive rates between the CIA and the immunoturbidimetric assay.
Although the false-reactive rate was higher for the reverse sequence algorithm (1.4%) than for the traditional sequence algorithm (0.5%), the former was able to detect 48 subjects with possible latent syphilis that were not detected by the latter. Discriminating between treated syphilis and latent syphilis requires knowledge of patient clinical history; however, we were unable to determine whether these 48 subjects had latent syphilis or previously treated (and resolved) syphilis because of insufficient clinical information. The probability of having syphilis might have been higher for subjects with latent syphilis that was not detected by RPR screening [e.g. CIA(+)/RPR(-)/TPPA(+)] than for TPPA(-) subjects, even after excluding those with a known history of syphilis [8]. Therefore, subjects with possible latent syphilis should be monitored and provided with options for syphilis infection evaluation during their health checkups.
A previous study found that enzyme immunoassay (EIA)-based screening algorithms were slightly more expensive than traditional RPR/VDRL-based algorithms, and also showed a three-fold increase in the number of follow-ups and an escalation in the number of patients receiving overtreatment [10]. That study analyzed a cohort of 200,000 individuals, including 1,000 current syphilis infections and 10,000 previous infections. The overtreatment cases were due to the relatively low specificity of the treponemal tests (EIA and TPPA) for previously infected individuals. In contrast, the high detection sensitivity obtained by using an antibody specific for T. pallidum is advantageous in situations of low syphilis prevalence, such as in general health checkups. Moreover, the commercial T. pallidum-specific immunoassays currently in use exhibit high sensitivity and specificity [11].
The second treponemal test performed to resolve the discordant results of the syphilis serologic tests (EIA/CIA-reactive, RPR-nonreactive specimen), is currently recommended by the US Centers for Disease Control and Prevention [12]. Interestingly, the CMIA-reactive subjects in this study were older than the CMIA-nonreactive subjects. Twelve of the 14 TPLA-reactive, RPR-nonreactive, and CMIA-nonreactive specimens were non-reactive by using the FTA-ABS test, indicating that the initial TPLA results were false reactives. However, the other two specimens were weakly reactive by the FTA-ABS test and had relatively high TPLA COI values (65 U and 71 U), suggesting that these two CMIA results were false nonreactives. The median and range of the TPLA COI values for the 12 false-reactive TPLA cases [TPLA(+)/RPR(-)/CMIA(-)] were lower than those of the true-reactive TPLA results [TPLA(+)/RPR(-)/CMIA(+)]. Furthermore, the majority (66.7%) of the 12 false-reactive TPLA cases had a COI value within a range of 10–15 U. These findings were helpful in ruling out cases of false-reactive TPLA results. In other words, cases with a COI<20 U were more likely to have false reactive initial TPLA test results. Although the manufacturer's recommended cutoff was 10 U, the optimal COI determined in this study for syphilis screening by TPLA was 16 U. The COI value correlating with TPLA positivity needs to be validated separately in each individual laboratory.
This study has some limitations. First, it was difficult to discriminate between previously treated syphilis and latent syphilis because of insufficient subject information. Second, the study subjects might not represent the general population of health examinees because most of them were men.
Notwithstanding these limitations, the current study shows that the reverse screening algorithm can detect subjects with possible latent syphilis, who could be provided with the opportunity for further infection evaluation. In addition, it demonstrates that the COI values of initial TPLA tests are helpful for excluding false-reactive TPLA cases. Conclusively, the reverse algorithm by using quantitative turbidimetric assay would be more efficient for syphilis screening during general health checkups.
Acknowledgments
This study was supported by Korea Association of Health Promotion.
Footnotes
Authors' Disclosures of Potential Conflicts of Interest: No potential conflicts of interest relevant to this article were reported.
References
- 1.Greenblatt RM, Lukehart SA, Plummer FA, Quinn TC, Critchlow CW, Ashley RL, et al. Genital ulceration as a risk factor for human immunodeficiency virus infection. AIDS. 1988;2:47–50. doi: 10.1097/00002030-198802000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Mehta SD, Ghanem KG, Rompalo AM, Erbelding EJ. HIV seroconversion among public sexually transmitted disease clinic patients: analysis of risks to facilitate early identification. J Acquir Immune Defic Syndr. 2006;42:116–122. doi: 10.1097/01.qai.0000200662.40215.34. [DOI] [PubMed] [Google Scholar]
- 3.Morshed MG. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015;22:137–147. doi: 10.1128/CVI.00681-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Müller I, Brade V, Hagedorn HJ, Straube E, Schörner C, Frosch M, et al. Is serological testing a reliable tool in laboratory diagnosis of syphilis? Meta-analysis of eight external quality control surveys performed by the German infection serology proficiency testing program. J Clin Microbiol. 2006;44:1335–1341. doi: 10.1128/JCM.44.4.1335-1341.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Workowski KA, Berman S Centers for Disease Control and Prevention (CDC) Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59:1–110. [PubMed] [Google Scholar]
- 6.Loeffelholz MJ. It is time to use treponema-specific antibody screening tests for diagnosis of syphilis. J Clin Microbiol. 2012;50:2–6. doi: 10.1128/JCM.06347-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tong ML, Lin LR, Liu LL, Zhang HL, Huang SJ, Chen YY, et al. Analysis of 3 algorithms for syphilis serodiagnosis and implications for clinical management. Clin Infect Dis. 2014;58:1116–1124. doi: 10.1093/cid/ciu087. [DOI] [PubMed] [Google Scholar]
- 8.Park IU, Chow JM, Bolan G, Stanley M, Shieh J, Schapiro JM. Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J Infect Dis. 2011;204:1297–1304. doi: 10.1093/infdis/jir524. [DOI] [PubMed] [Google Scholar]
- 9.Binnicker MJ, Jespersen DJ, Rollins LO. Direct comparison of the traditional and reverse syphilis screening algorithms in a population with a low prevalence of syphilis. J Clin Microbiol. 2012;50:148–150. doi: 10.1128/JCM.05636-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owusu-Edusei K, Jr, Peterman TA, Ballard RC. Serologic testing for syphilis in the United States: a cost-effectiveness analysis of two screening algorithms. Sex Transm Dis. 2011;38:1–7. doi: 10.1097/OLQ.0b013e3181ec51f1. [DOI] [PubMed] [Google Scholar]
- 11.Park BG, Yoon JG, Rim JH, Lee A, Kim HS. Comparison of six automated Treponema-Specific antibody assays. J Clin Microbiol. 2016;54:163–167. doi: 10.1128/JCM.02593-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Discordant results from reverse sequence syphilis screening-five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011;60:133–137. [PubMed] [Google Scholar]