Abstract
Objective
To analyze the financial burden of complementary and alternative medicine (CAM) in cancer treatment.
Materials and Methods
Based on a systematic search of the literature (Medline and the Cochrane Library, combining the MeSH terms ‘complementary therapies’, ‘neoplasms’, ‘costs’, ‘cost analysis’, and ‘cost-benefit analysis’), an expert panel discussed different types of analyses and their significance for CAM in oncology.
Results
Of 755 publications, 43 met our criteria. The types of economic analyses and their parameters discussed for CAM in oncology were cost, cost-benefit, cost-effectiveness, and cost-utility analyses. Only a few articles included arguments in favor of or against these different methods, and only a few arguments were specific for CAM because most CAM methods address a broad range of treatment aim parameters to assess effectiveness and are hard to define. Additionally, the choice of comparative treatments is difficult. To evaluate utility, healthy subjects may not be adequate as patients with a life-threatening disease and may be judged differently, especially with respect to a holistic treatment approach. We did not find any arguments in the literature that were directed at the economic analysis of CAM in oncology. Therefore, a comprehensive approach assessment based on criteria from evidence-based medicine evaluating direct and indirect costs is recommended.
Conclusion
The usual approaches to conventional medicine to assess costs, benefits, and effectiveness seem adequate in the field of CAM in oncology. Additionally, a thorough deliberation on the comparator, endpoints, and instruments is mandatory for designing studies.
Key Words: Complementary medicine, Costs, Economic evaluation, Evidence-based medicine, Benefit, Cancer
Introduction
Cancer patients are highly interested in complementary and alternative medicine (CAM). In Western countries, 40-90% of cancer patients use CAM [1,2,3]. In most countries, patients have to pay for CAM [4,5]. Hence, there is an ongoing discussion regarding whether health insurance companies should reimburse payments and, if so, under what terms. Different models are conceivable. Reimbursement might include compulsory statutory health services or might be offered as an additional service in which insurees can select a special tariff that includes CAM. Because most biologically based CAM are over-the-counter drugs, reimbursement could be free, restricted to methods on a list from an official institution, or they may be restricted to a prescription by a physician. In the latter cases, the institution or the prescribing physician would need qualifications the definition of which would need to be integrated into the health care system. Authorized physicians may be specialists in naturopathy, oncologists with training in CAM, or those who have attended a specified curriculum.
In the German health care system, the Federal Joint Committee (Gemeinsamer Bundesausschuss; G-BA) is responsible for decisions on reimbursement. The G-BA decides based on cost-effectiveness analyses compared to standard therapy. So far, most types of CAM are not part of these decisions for the following two reasons: (a) in Germany, most CAM drugs are not registered as medical drugs but rather as nutritional supplements and (b) some types of naturopathy have ‘special treatment’ (besondere Therapierichtungen) status, which means that they are not regulated as conventional medicines but are instead regulated according to so-called internal proofs (Binnenbeweis) [6].
Proponents for a comprehensive integration of CAM methods into the health care and reimbursement system point to patient preferences for ‘natural’ therapies, benefits such as supportive therapies, improvement of the quality of life, and the comparably low costs of most CAM methods [7,8,9,10,11]. Accordingly, the hypothesis is that CAM in oncology may prove to be cost effective.
Very few data exist on this topic. Recently, a review identified a few controlled studies on CAM in which a better or similar effectiveness was reported compared to conventional treatments. The costs were lower in some of these studies, but they were similar or even higher than those of conventional therapy alone in others [4].
In 2013, Coulter et al. [5] published an article on economic analyses of complementary and alternative medicine. In that paper, an expert panel defined the following 5 topics which they considered important: standardization of economic evaluation methods for both CAM and conventional medicines, identification of key questions, the target audience and whose perspective is used, description of the analytic methods to be used, definition of the outcomes to be measured, and consideration of the overall healthcare costs.
To date, in oncology, only a few studies have provided economic data combined with data on effectiveness or benefits. All of these studies have methodological fallacies and are not appropriate to support decision making [6].
Additionally, ethical considerations in cancer care are highly relevant for individuals (due to the severity of the disease and its sequels), as well as for the health care system (due to the high number of members of a society affected and the high consumption of resources).
Accordingly, we resolved to provide a framework for CAM economic analysis in cancer care that may help scientists to plan acquisition of data on CAM and policy makers to decide which data to use for legal decisions.
Materials and Methods
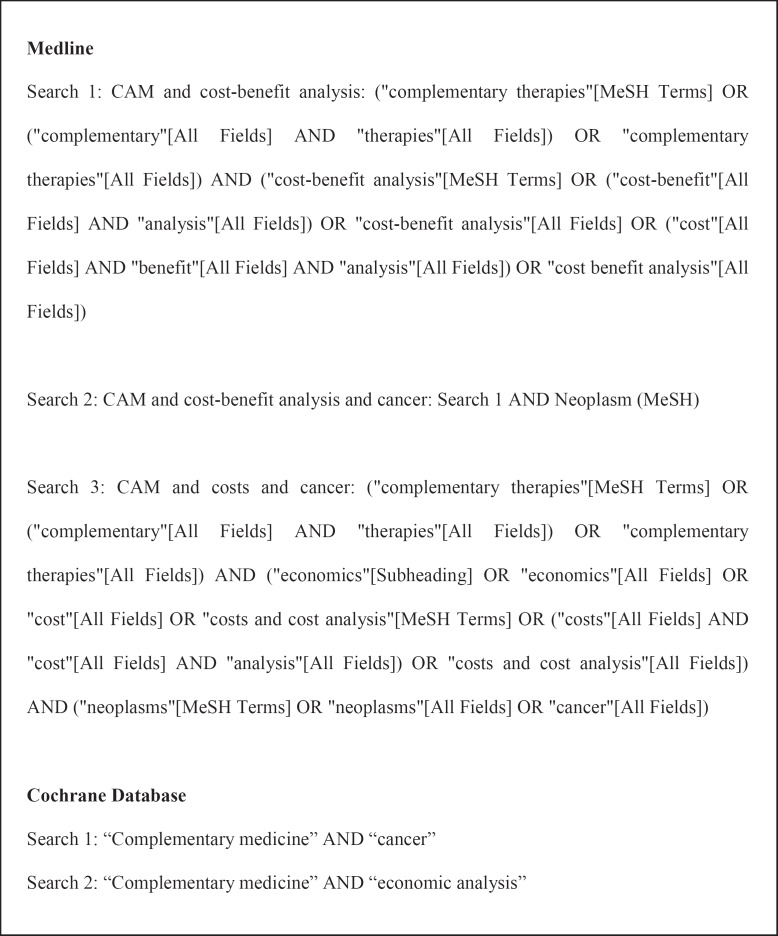
A systematic search of the literature was completed in Medline and the Cochrane Library, adapting the search strings from Coulter et al. [5] (fig. 1). We restricted the publication date from 1950 up to the end of 2013 and set language filters for English and German publications.
Fig. 1.
Search strings.
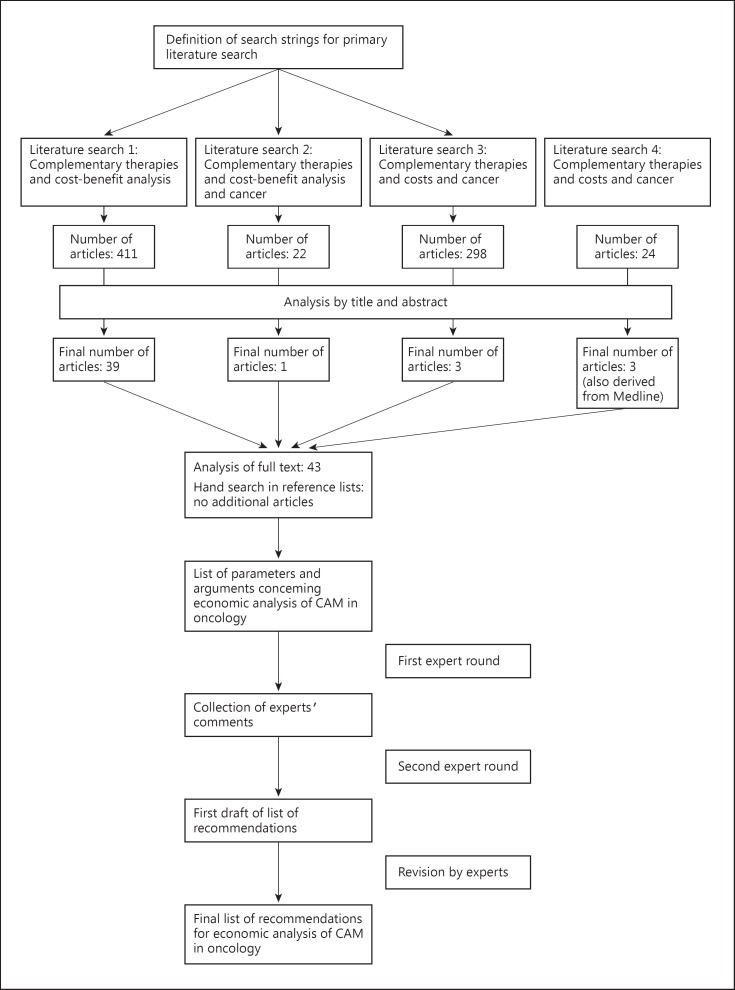
The results were screened by title and abstract. We excluded all articles that did not focus on CAM or did not provide data on costs and efficacy. All of the remaining articles were fully analyzed. Moreover, all reference lists from these articles were searched for additional publications. We prepared an overview of the different types of economic analyses and the parameters considered in these analyses. Arguments provided in the articles regarding these parameters with respect to CAM in oncology were compiled.
This first overview was sent to the experts on complementary oncology of the Prevention and Integrative Oncology Working Group of the German Cancer Society. All experts were working in certified cancer centers in Germany, mainly in a leading position, such as head of a department caring for cancer patients (medical oncology, radio-oncology, gynecology, rhino-otopharyngology, and/or palliative medicine). All experts had experience in a range of complementary medicines, mostly in biological (substance-based) methods but also in homeopathy, anthroposophical medicine, and acupuncture. They were asked to comment on the different types of analyses and the arguments from the literature. We summarized the different arguments and asked the experts to approve, reject, or comment on each issue. With these answers, we set up a list of recommendations that was sent to all participants for further comments (fig. 2).
Fig. 2.
Document development process.
As this work did not refer to patients or patients' data, no ethical vote was necessary.
Results
We identified 755 publications from our literature search. After checking the articles by title and abstract, the remaining 43 articles were assessed as full text.
The types of economic analyses and their parameters discussed for CAM in oncology are cost, cost-benefit, cost-effectiveness, and cost-utility analysis (table 1). Only 7 articles included arguments in favor of or against these different methods and only a few arguments were specific for CAM. Direct, indirect, and intangible cost analyses or cost-cost analyses are assessed in all of the methods [4,12]. Direct costs include practitioners, diagnostics, and treatment costs (table 1). These costs may very between different institutions. Indirect costs include treatment facility provisions for the methods that are not a part of regular institution services, patient out-of-pocket costs, etc. Intangible costs stem from the burden of the therapy on the side of the patient as pain or adherence to conventional treatment. The different treatment modalities may be assessed in terms of survival time or quality of life and compared for different patient populations with the benefit construct. The effectiveness construct is used to compare alternative treatments in specific situations, while utility is used to compare alternative treatments in one situation with diverse outcomes, such as survival time and quality of life [4,12,13]. Utility is used to compare treatments with different integrating outcomes, such as quality of life.
Table 1.
Parameters for analysis of the costs and effectiveness of CAM in oncology as discussed or used in the literature
| Type of analysis | Description | Parameters for costs | Arguments and questions to consider using these parameters |
|---|---|---|---|
| General consideration How relevant are data from study populations for the individual patient? Because CAM focuses on the needs of the individual patient, should the relevance of the data from studies be questioned? |
|||
| Cost analysis and cost-cost analysis | Direct costs of therapy1, 7 | Practitioner fees Diagnostic costs Therapy costs Service costs Facilities and equipment Ancillary staff Transportation Time off work (patient and relatives) Time Costs may vary with time in case of longer periods, discount rates have to be regarded Places Costs may be variable in different places Costs are different between countries Cost perspective Overall cost perspective or diagnosis of specific perspectives?5 |
|
| Indirect costs1 | Provisions of the treatment facility for a method that is not part of regular health care Out-of-pocket costs to the patient Private costs Equipment purchase costs Productivity loss (patient and relatives) Time spent by the patient or relatives (including traveling and waiting) Other costs for society (pension, home care, care for minor children, or resources spent as manpower by professionals) Costs for caregivers Costs due to treatment failures |
||
| Intangible costs1 | Pain Suffering Grief Adherence |
||
| Cost-benefit analysis | Assigning a monetary value to the benefit (effect) of a treatment | Benefit in terms of Survival time Quality of life Allows for comparison of different treatment modalities and between different patient groups1, 3, 7 For costs, see previous page |
How and by whom is the benefit defined and measured? A monetary value for benefits may be difficult to define and consent (e.g. life) Most CAM methods address a broad range of treatment aims at the same time in the same individual Other benefits, such as ‘wholeness’ and ‘well-being’, are often discussed for CAM Examples of intangible benefits or humanistic outcomes1, 2 Sense of safety Physical comfort Enjoyment Meaningful activity Relationships Functional competence Dignity Privacy Individuality Autonomy Spiritual well-being Instruments from conventional medicine may not be adequate to measure the benefits and outcomes of CAM treatments |
| Cost-effectiveness and cost-utility analysis | Effectiveness | Effectiveness helps to compare alternative treatments in the same situation Direct comparability between different treatments with respect to the health-related outcomes1, 3, 7 For costs, see previous page Incremental cost-effectiveness analysis (ICER): ratio of the difference between costs and the difference between effectiveness between two treatments6 |
Choice of comparative treatment How should comparative treatment be determined? (Conventional method, CAM methods with similar goals or with a similar approach, or method with a similar amount of evidence?) How and by whom is effectiveness defined and measured? Is the concept of effectiveness different in CAM? |
| Utility | Allows one to compare treatments with different integrating outcomes and consequences, e.g. QoL measured in units and QALY1, 3, 4, 7 Utility may be measured using a visual analogue scale, time trade-off, and standard gamble For costs, see previous page |
Defining utility is highly subjective Often healthy subjects are used for these judgments Using healthy subjects for ratings does not take into account that patients with a life-threatening disease may judge the situation completely differently Healthy people may not be able to perceive the benefits of holistic care |
|
We did not find any arguments in the literature that were directed at the economic analysis of CAM in oncology. For CAM in general, several main issues are discussed in the literature. A more general question is whether data from study populations are relevant for individual patients. This question is also valid in conventional medicine. However, as with many CAM methods, the active continuous contribution of the patient is mandatory; this may be even more important. Medical benefits are mostly described in terms of survival and quality of life. However, most CAM methods address a broad range of treatment aims at the same time in the same individual, meaning that a monetary value for the benefits may be hard to define and consent. Furthermore, other CAM benefits are often discussed as ‘wholeness’ or ‘well-being’. Accordingly, intangible benefits may also be defined as humanistic outcomes, such as a sense of safety, physical comfort, enjoyment, meaningfulness, relationships, dignity, privacy, individuality, autonomy, and spiritual well-being. Some of these items, such as autonomy, are also acknowledged in conventional medicine. However, though most are accepted, there are no validated instruments to measure these factors, which makes assessment nearly impossible. Moreover, a monetary value for these outcomes (e.g. ‘wholeness’) may be hard to define and evaluate in a diverse society. Some CAM experts challenge whether instruments from conventional medicine are valid to measure the outcomes of CAM treatments.
Because most CAM methods address a broad range of treatment aims at the same time in the same individual, parameters to assess their effectiveness are hard to define and evaluate. To assess effectiveness, the choice of comparative treatment is difficult. There is no agreement as to whether this comparator should be derived from conventional or complementary methods. In the case of other CAM methods, this might be one with similar goals or with a similar approach. For the evaluation of utility, healthy subjects are often used. This does not take into account that patients with a life-threatening disease may be judged quite differently, especially with respect to holistic treatment approaches.
Discussion
As a first step, the experts consented that all 4 types of analyses can be used for CAM in oncology. The general concern in the literature [14] that data from study populations may not be relevant for individual patients was not considered a problem typical of CAM but rather a general problem. The solution is for evidence based-medicine to build treatment recommendations based on external as well as internal evidence, though patient preferences were thought to be adequate for conventional as well as complementary medicine.
The experts consented that assessment of the costs, including direct and indirect costs as well as intangible costs, must be considered. They should be assessed not only during active treatment but also during some follow-ups, as treatments often have long-lasting consequences and, even in the case of complete remission, patients may relapse in the ensuing months or years. For some entities, curation is not completely possible and patients may live with a chronic disease with several different treatments for years. In all of these cases, patients with positive CAM experiences may want to continue these efforts. For example, a woman with hot flashes who has been under endocrine adjuvant therapy for 5 or 10 years and benefits from yoga may want to continue the exercises.
The argument in favor of CAM that its costs are lower than those of conventional medicines was questioned for oncology. In fact, complementary medicine in oncology is an add-on and no substitute for conventional cancer treatments. CAM will not replace supportive therapy. Accordingly, additional costs are to be expected [15]. Furthermore, using CAM may impact adherence to conventional medicines, which may be increased or reduced. Moreover, biologically based CAM may have side effects and interactions with conventional drugs. Both may lead to additional treatment costs that may influence treatment results and cause side effects due to conventional treatment [16,17,18]. Accordingly, a comprehensive assessment of costs from CAM may result in more or fewer costs. This result may vary from the short term to the long term, which entails the necessity for long-term surveillance. For the example, in the woman with hot flashes, reducing these side effects may improve adherence and reduce the risk of relapse and consecutive costs. In contrast, yoga classes may add to the costs on the side of the woman but may provide other benefits, such as more physical fitness and fewer complaints of musculoskeletal problems. Additionally, considering the benefits, effectiveness, or utility, adequate measurements must include data on survival and (health-related) quality of life. The experts did not see any convincing arguments for a decisive difference between the definition of benefit effectiveness or utility for conventional versus complementary medicine. Accordingly, from the point of view of a health care system, the same steps for defining these measurements were adequate for both conventional treatments and CAM. For a comprehensive analysis of the benefits of CAM, evidence-based medicine methods are adequate and necessary. However, assessing the impact of CAM on survival or quality of life may be difficult because CAM is provided as an add-on to conventional therapy. To assess its effectiveness, a study comparing conventional medicine combined with CAM versus conventional medicine alone was not rated as adequate. Defining a portion of conventional medicine added in the control arm was thought to be decisive. Examples discussed were physiotherapy versus yoga or more time for discussion with the patient versus homeopathy.
Criticism of quality-of-life instruments used in studies for conventional treatments argues that these instruments are not comprehensive and do not take into account the individual's preferences [19]. Coulter et al. [5] also pointed to the goals of CAM, which aim toward a more holistic approach. Accordingly, an economic analysis of CAM should include the patient's perspective and a broader range of benefits.
In contrast, the experts did not find systematic or inherent differences in the benefit measurements between CAM and conventional medicines. Accordingly, there is no reason to acknowledge different outcome parameters for conventional medicine and CAM. In oncology, survival endpoints are of great relevance to patients and should not be neglected. In contrast, validated instruments exist and should be used to determine patient-reported outcomes. More individualized assessments integrating individuals' priorities are possible even with these standardized instruments [20].
Another point discussed in the literature is the lack of adequate comparators in CAM studies because conventional medicine lacks patient-centered approaches. Again, the experts did not see a principal difference between CAM and conventional oncology. As a consequence, in the case of a direct comparison of CAM with conventional medicine and psychological methods, physical activity and lifestyle interventions, communication, providing information, and psycho-education should be regarded.
The effects of different CAM methods may result from so-called unspecific effects due to patient-professional interactions. However, the experts did not agree on a concept of unspecific effects that are entirely restricted to CAM. In contrast, these effects may also arise in conventional treatment (e.g. supportive care, communication). As a consequence, for a thorough cost-benefit-analysis, the facilitators of unspecific effects in conventional medicine could be described in a study and costs could be assessed. In the case of no such conventional treatment existing, an incremental cost-effectiveness analysis for the economic analysis could be completed.
Conclusions and Recommendations
From this discussion, we would like to suggest 8 recommendations that were agreed upon by the experts. Recommendations for the economic analysis of CAM in oncology include: cost-cost, cost-benefit, cost-effectiveness, and cost-utility analyses are adequate for assessing CAM in oncology if all of the necessary data are available. All of these economic analyses are based on criteria from evidence-based medicine for effects and effectiveness. To determine the comparative treatment, all options (from conventional oncology, psycho-oncology, psycho-education, palliative care, etc.) need to be considered. When planning a study, the settings should be comparable to the settings of usual care and the study populations should be comparable to the patients in usual care. For assessing costs, a comprehensive approach based on direct as well as indirect costs is recommended; costs that are directly and indirectly paid for by patients and their families must be included. Assessment of intangible costs should be integrated. The same parameters should be analyzed when comparing CAM and conventional oncology. The influences of CAM on treatment costs in conventional medicine and vice versa should be assessed. Benefit and effectiveness should be compared using the same parameters for CAM as for conventional oncology. These parameters should include clinically relevant data on survival and quality of life and comprehensive reporting of adverse events. Outcomes reported by patients should also be included. Integrating the patient's perspective into the assessment of benefits and risks is recommended in CAM as well as in conventional oncology. Using the perspective of healthy people to rate or rank benefits is not recommended.
Disclosure Statement
None.
References
- 1.Eschiti VS. Lesson from comparison of CAM use by women with female-specific cancers to others: it's time to focus on interaction risks with CAM therapies. Integr Cancer Ther. 2007;6:313–344. doi: 10.1177/1534735407309257. [DOI] [PubMed] [Google Scholar]
- 2.Horneber M, Bueschel G, Dennert G, et al. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11:187–203. doi: 10.1177/1534735411423920. [DOI] [PubMed] [Google Scholar]
- 3.Molassiotis A, Fernadez-Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655–663. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 4.Herman PM, Craig BM, Caspi O. Is complementary and alternative medicine (CAM) cost-effective? A systematic review. BMC Complement Altern Med. 2005;5:11. doi: 10.1186/1472-6882-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coulter ID, Herman PM, Nataraj S. Economic analysis of complementary, alternative, and integrative medicine: considerations raised by an expert panel. BMC Compl Altern Med. 2013;13:191. doi: 10.1186/1472-6882-13-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bundesinstitut für Arzneimittel und Medizinprodukte Besondere Therapierichtungen und traditionelle Arzneimittel. http://www.bfarm.de/DE/Arzneimittel/zul/zulassungsarten/besTherap/_node.html (accessed May 22, 2016).
- 7.Kienle GS, Albonico HU, Fischer L, et al. Complementary therapy systems and their integrative evaluation. Explore. 2011;7:175–187. doi: 10.1016/j.explore.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Schad F, Axtner J, Happe A, et al. Network Oncology (NO) – a clinical cancer register for health services research and the evaluation of integrative therapeutic interventions in anthroposophic medicine. Forsch Komplementmed. 2013;20:353–360. doi: 10.1159/000356204. [DOI] [PubMed] [Google Scholar]
- 9.Gerst T. Dialogforum Pluralismus in der Medizin: politische Absicherung des Erreichten. Dtsch Arztebl Int. 2010;107:2286. [Google Scholar]
- 10.Karl und Veronica Carstens-Stiftung Presseinformation: Stellungnahme der Carstens-Stiftung. http://www.carstens-stiftung.de/service/presse_downloads/SPIEGEL_ Stellungnahme_KVC.pdf (assessed May 22, 2016).
- 11.Kienle GS, Kiene H, Albonico HU. Anthroposophic medicine: health technology assessment report – short version (in German). Forsch Komplementmed. 2006;3(suppl 2):7–18. doi: 10.1159/000093481. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy DA, Hart J, Seely D. Cost effectiveness of natural health products: a systematic review of randomized clinical trials. Evid Based Complement Alternat Med. 2009;6:297–304. doi: 10.1093/ecam/nem167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witt CM. Health economic studies on complementary and integrative medicine. Forsch Komplementmed. 2001;18:6–9. doi: 10.1159/000324615. [DOI] [PubMed] [Google Scholar]
- 14.Awad AI, Al-Ajmi S, Waheedi MA. Knowledge, perceptions and attitudes toward complementary and alternative therapies among Kuwaiti medical and pharmacy students. Med Princ Pract. 2012;21:350–354. doi: 10.1159/000336216. [DOI] [PubMed] [Google Scholar]
- 15.Spinks J, Hollingsworth B. Are the economics of complementary and alternative medicine different to conventional medicine? Expert Rev Pharmacoecon Outcomes Res. 2009;9:1–4. doi: 10.1586/14737167.9.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Izzo AA. Interactions between herbs and conventional drugs: overview of the clinical data. Med Princ Pract. 2012;21:404–428. doi: 10.1159/000334488. [DOI] [PubMed] [Google Scholar]
- 17.Zeller T, Muenstedt K, Stoll C, et al. Potential interactions of complementary and alternative medicine with cancer therapy in outpatients with gynecological cancer in a comprehensive cancer center. J Cancer Res Clin Oncol. 2013;139:357–365. doi: 10.1007/s00432-012-1336-6. [DOI] [PubMed] [Google Scholar]
- 18.Loquai C, Dechent D, Garzarolli M, et al. Risk of interactions between complementary and alternative medicine and medication for comorbidities in patients with melanoma. Med Oncol. 2016;33:52. doi: 10.1007/s12032-016-0764-6. [DOI] [PubMed] [Google Scholar]
- 19.Bridges JF. Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Appl Health Econ Health Policy. 2003;2:213–224. [PubMed] [Google Scholar]
- 20.Huebner J, Rosé C, Geissler J, et al. Integrating cancer patients' perspectives into treatment decisions and treatment evaluation using patient-reported outcomes – a concept paper. Eur J Cancer Care. 2013 doi: 10.1111/ecc.12095. DOI: 10.1111/ecc12095. [DOI] [PubMed] [Google Scholar]
- 21.Hollinghurst S, Shaw A, Thompson EA. Capturing the value of complementary and alternative medicine: including patient preferences in economic evaluation. Complement Ther Med. 2008;16:47–51. doi: 10.1016/j.ctim.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Chuang LH, Soares MO, Tilbrook H, et al. A pragmatic multicentered randomized controlled trial of yoga for chronic low back pain: economic evaluation. Spine (Phila Pa 1976) 2012;37:1593–1601. doi: 10.1097/BRS.0b013e3182545937. [DOI] [PubMed] [Google Scholar]
- 23.Robinson N, Donaldson J, Watt H. Auditing outcomes and costs of integrated complementary medicine provision – the importance of length of follow up. Complement Ther Clin Pract. 2006;12:249–257. doi: 10.1016/j.ctcp.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Willich SN, Reinhold T, Selim D, et al. Cost-effectiveness of acupuncture treatment in patients with chronic neck pain. Pain. 2006;125:107–113. doi: 10.1016/j.pain.2006.06.006. [DOI] [PubMed] [Google Scholar]