Abstract
BACKGROUND
Perioperative regional anaesthesia may protect from persistent postsurgical pain (PPSP) and improve outcome after total knee arthroplasty (TKA).
OBJECTIVES
Aim of this study was to evaluate the impact of regional anaesthesia on PPSP and long-term functional outcome after TKA.
DESIGN
A web-based prospective observational registry.
SETTING
Five Italian Private and University Hospitals from 2012 to 2015.
PATIENTS
Undergoing primary unilateral TKA, aged more than 18 years, informed consent, American Society of Anesthesiologists (ASA) physical status classes 1 to 3, no previous knee surgery.
INTERVENTION(S)
Personal data (age, sex, BMI and ASA class), preoperative pain assessed by numerical rating scale (NRS) score, and risk factors for PPSP were registered preoperatively. Data on anaesthetic and analgesic techniques were collected. Postoperative pain (NRS), analgesic consumption, major complications and patient satisfaction were registered up to the time of discharge. PPSP was assessed by a blinded investigator during a phone call after 1, 3 and 6 months, together with patient satisfaction, quality of life (QOL) and walking ability.
MAIN OUTCOME MEASURES
Experience of PPSP according to the type of peri-operative analgesia.
RESULTS
Five hundred sixty-three patients completed the follow-up. At 6 months, 21.6% of patients experienced PPSP, whereas autonomy was improved only in 56.3%; QOL was worsened or unchanged in 30.7% of patients and improved in 69.3%. Patients receiving continuous regional anaesthesia (epidural or peripheral nerve block) showed a lower NRS through the whole peri-operative period up to 1 month compared with both single shot peripheral nerve block and those who did not receive any type of regional anaesthesia. No difference was found between these latter two groups. Differences in PPSP at 3 or 6 months were not significantly affected by the type of anaesthesia or postoperative analgesia. A higher NRS score at 1 month, younger age, history of anxiety or depression, pro-inflammatory status, higher BMI and a lower ASA physical status were associated with a higher incidence of PPSP and worsened QOL at 6 months.
CONCLUSION
Continuous regional anaesthesia provides analgesic benefit for up to 1 month after surgery, but did not influence PPSP at 6 months. Better pain control at 1 month was associated with reduced PPSP. Patients with higher expectations from surgery, enhanced basal inflammation and a pessimistic outlook are more prone to develop PPSP.
TRIAL REGISTRATION
Clinicaltrials.gov identifier: NCT02147730
Introduction
Postoperative analgesia after total knee arthroplasty (TKA) is challenging. Inadequate pain relief is associated with peri-operative complications, difficult rehabilitation and prolonged recovery.1,2 Regional anaesthesia has been proven to offer some advantages in this surgical setting. A continuous postoperative peripheral nerve block (PNB) (either femoral or adductor canal) after TKA helps to fulfil three specific discharge criteria: adequate analgesia, independence from intravenous opioids, and ambulation targets.3–6
Long-term rehabilitation following TKA is a subject of current interest, and chronic persistent postsurgical pain (PPSP) has been shown to be a problem common to a variety of surgical procedures.7 PPSP is a complex condition in which inflammatory, nociceptive and neuropathic components are involved.8 Its incidence varies widely, according to the type of surgery, and after TKA it ranges between 20 and 50% at 1 year.9,10 Given the number of TKA performed every year11 a large number of individuals must be affected.
Among the risk factors for PPSP, the severity of acute postoperative pain is often listed. Those individuals who experience intense acute postoperative pain may be the ones most vulnerable to chronic PPSP and the severity of pre-operative pain is also a documented risk for PPSP development.7,12,13 TKA patients are doubly vulnerable being exposed to both factors: pre-operative pain is the main motivation for surgery, and TKA can be associated with severe postoperative pain. They are at high risk of PPSP, which serves to undermine their efforts and expectations, leaving them demoralised and disillusioned.
Regional anaesthesia can improve postoperative analgesia, but it is uncertain whether it can influence the development of chronic PPSP and improve long-term outcome.14
We performed this prospective observational study to evaluate the effects of different anaesthetic and analgesic techniques on both short-term and long-term outcome after TKA, with special interest on PPSP, functional outcome and the quality of life (QOL).
Methods
The current prospective-based, observational-based, population-based multicentre registry was part of the bigger A.L.I.C.E. study (regional anaesthesia in Italy – complications and outcomes) designed according to STROBE guidelines.15
The study received ethical approval from the coordinating centre (IRCCS Policlinico San Matteo, Pavia, Italy). It was approved by the collaborating institutions (ASST-Gaetano Pini-CTO – Milano, Ospedale di Circolo-Varese, Ospedale Cottolengo-Torino, ASST-Monaldi-Napoli, Italy). The study was advertised in national anaesthesia meetings between 2012 and 2015, and at the ESRA Italian Chapter Annual Meeting. Any centre willing to participate was provided with all the documents needed for local approval, and a local representative was nominated to coordinate the project and take responsibility for data collection.
Patients to be included were scheduled for primary unilateral TKA, aged more than 18 years and able to give written and informed consent. Those with American Society of Anesthesiology (ASA) physical status class more than 3, those unable to give consent, and any undergoing bilateral TKA or with previous knee surgery were excluded.
Data were collected in a prospective fashion on universal case report forms used by all participants, which were sent to the coordinating centre quarterly.
Enrolment was at the pre-operative visit when the study was explained by either the surgeon or the anaesthesiologist and consent was obtained. Each patient was assigned with a code to protect privacy.
Data noted at the pre-operative visit included: age, sex, BMI, ASA class, the presence and intensity of pre-operative pain [numerical rating scale (NRS) score both at rest and during walking], and the risk factors for PPSP as currently understood. These are anxiety or depression, a pessimistic outlook, obesity, diabetes and pro-inflammatory conditions (immune/rheumatologic disease, headache, irritable bowel syndrome or inflammatory bowel diseases and fibromyalgia), low back pain with or without radicular symptoms and home therapy. The pre-operative ability to walk was also registered: no walking (<50 m), poor walking (up to 500 m), good walking (between 500 and 1000 m) and unlimited (>1000 m).
Data of both anaesthetic and the analgesic techniques were registered on the day of surgery: General and regional anaesthesia alone or combined, the use of local infiltration analgesia (LIA), as well as PNB, epidural analgesia, local anaesthetic infusion and adjuvants. An infusion of local anaesthetic was registered as ‘continuous analgesia’ only when lasting for more than 24 h. We also collected data regarding the use of steroids, NSAIDs, paracetamol and opioids.
Postoperative assessment included pain measured with NRS (11 point scale from 0 – no pain to 10 – worst imaginable pain) both at rest and moving (both active and passive knee flexion) analgesic consumption, postoperative complications (postoperative nausea and vomiting (PONV), neurological dysfunction, systemic infection, ischaemia and patient satisfaction at first (POD1) and second (POD2) postoperative day, and again on discharge.
An investigator blind to the data evaluated the presence of PPSP at 1, 3 and 6 months (defined as a NRS more than 3 either at rest or during daily activity, and the associated consumption of any analgesic drugs for knee pain), patient satisfaction (on a 1 to 10 scale), the subjective QOL and the walking distance using a standardised questionnaire (see appendix).
Statistical analysis
The statistical analysis was performed with the dedicated software programme Stata 11.1 (StataCorp. LP, College Station, Texas, USA).
The primary outcome for this study was the incidence of PPSP. Secondary outcomes were the comparison of PPSP incidence by peri-operative regimen, the ability to walk, the QOL, patient satisfaction and the incidence of complications with respect to the type of peri-operative analgesia.
Given a reported incidence of PPSP between a minimum of 10% and a maximum of 50%,7 we planned to enrol a total of 600 patients. This sample size yields 95% confidence interval of 7.7 to 12.7% for the minimum incidence (10%) and of 44 to 54% for the maximum incidence (50%).
We built three different logistic regression models taking the following as the dependent variables: PPSP (‘no’/‘yes’ if either daily analgesic consumption or NRS > 3; since pain at rest was absent in all of the patients, movement-evoked pain was sought), improved autonomy (‘no’ if reduced or unchanged where restricted before surgery/‘yes’ if improved or unchanged where unrestricted before surgery) and improved health-related QOL (‘no’ if worsened or unchanged/‘yes’ if improved). Moreover, we built a linear regression model taking satisfaction (continuous on a 10-cm visual analogue scale) as the dependent variable.
These four predictive models were assembled for assessments taken 6 months after surgery. Similar models were implemented for assessments obtained on POD1, POD2 and 1 month after surgery for NRS more than 3.
Variable selection (likelihood ratio test or linear regression as appropriate, with P < 0.20) was applied to the following variables: age, BMI, pre-operative NRS (continuous variables), sex, pre-operative inflammatory state, pre-operative lumbar pain (categorical no/yes variables), ASA status (I, II and III), type of anaesthesia (general, spinal and PNB) and postoperative use of regional analgesia [none, single-shot PNB (ssPNB), continuous both epidural or PNB]. In the final models, significance was set at P less than 0.05.
Results
The current trial was registered on Clinicaltrials.gov (registration number NCT02147730).
Between January 2013 and April 2015, 614 patients were assessed for eligibility, and 563 of them completed the 6-month follow-up (Fig. 1). Of these, 421 (69.4%) were women and 185 were men. The median [IQR (range)] age was 72 [67 to 77 (26 to 88)], median BMI was 28 [25 to 31 (16 to 41)]. Thirty-three (5.4%) were ASA class 1, 510 (80.8%) were ASA class 2 and 58 (9.6%) were ASA class 3. Preoperative NRS was seven [5 to 8 (0 to 10)]. Our cohort reflects the general pattern of patients undergoing TKA.16
Fig. 1.
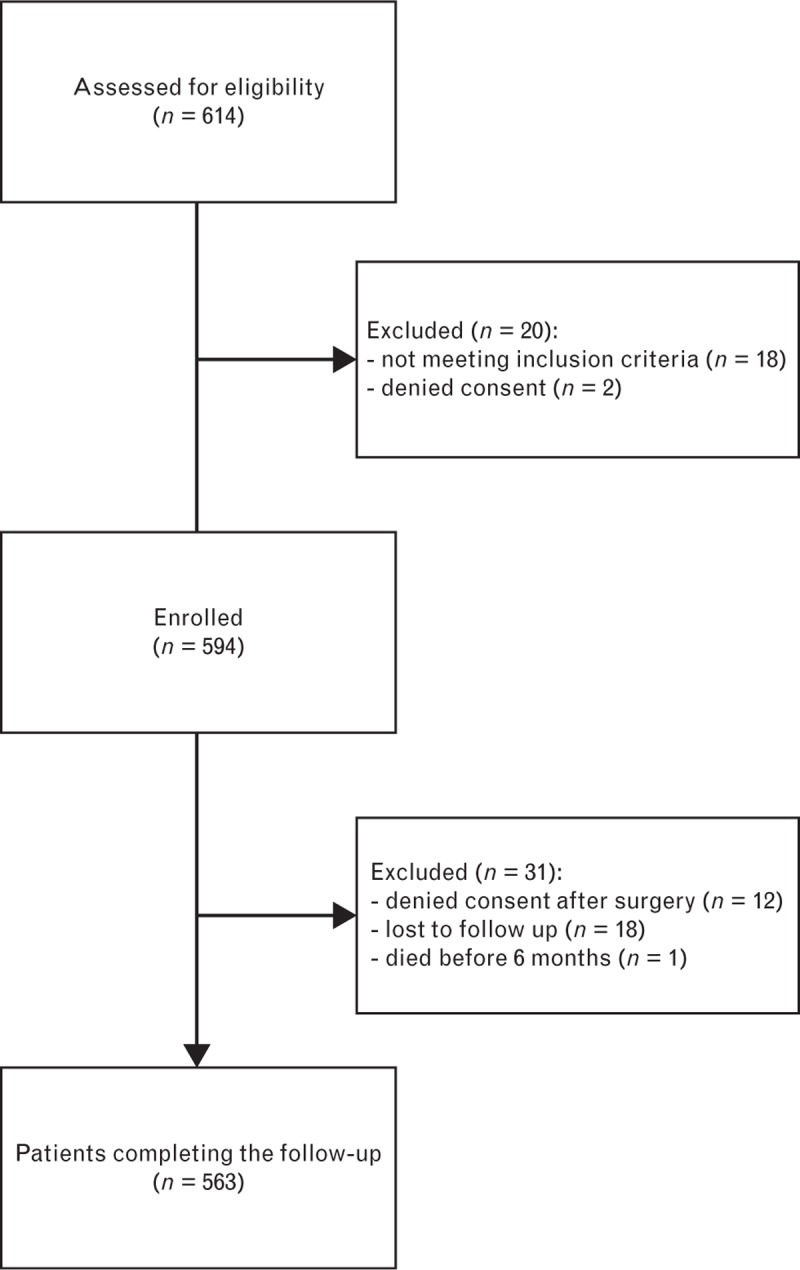
Study flow chart.
General anaesthesia was given to 302 patients (50.2%), spinal anaesthesia to 263 (43.7%) and the remainder 36 (6.1%) received lumbar plexus + sciatic nerve block (PNB).
Six months after surgery 122/563 (21.6%) of patients reported PPSP. The ability to walk was improved in 317 (56.3%) and the QOL was worsened or unchanged in 173 (30.7%) and improved in 390 (69.3%).
Logistic regression identified the following independent risk factors for the evaluated 6-month outcomes (PPSP, walking distance, QOL and satisfaction): age, NRS more than 3 at 1 month, preoperative inflammatory status, BMI, anxiety-depression, ASA and the preoperative NRS (Table 1).
Table 1.
Predictive model for persistent postsurgical pain, quality of life, ability to walk and satisfaction 6 months after total knee arthroplasty
| Dependent variable | Predictors | |||
| PPSP | OR (95% CI) | P | Whole-model P | |
| Age | 0.977 (0.956 to 0.998) | 0.025 | <0.0001 | |
| NRS > 3 1 month after surgery | 3.710 (2.305 to 5.974) | <0.0001 | ||
| QOL | OR (95% CI) | P | Whole-model P | |
| Preoperative NRS | 1.195 (1.093 to 1.306) | <0.0001 | <0.0001 | |
| Inflammation | 0.448 (0.237 to 0.847) | 0.014 | ||
| Walking distance | OR (95% CI) | P | Whole-model P | |
| ASA > 1a | 2.783 (1.103 to 7.026) | 0.030 | 0.030 | |
| Satisfaction | Coeff. (95% CI) | P | Whole-model P/Adj. R2 | |
| Anxiety/depression | −0.346 (−0.652 to 0.040) | 0.027 | 0.0035/0.0167 | |
| BMI | 0.035 (0.006 to 0.063) | 0.017 | ||
ASA, American Society of Anesthesiologists; CI, confidence interval; NRS, numerical rating scale; OR, odds ratio; PPSP, persistent postsurgical pain; QOL, quality of life.
aASA II did not differ from ASA III, whereas both ASA II and III differed from ASA I. Hence ASA has been recoded into ASA > 1 (no/yes).
For perioperative management, 50 (8.2%) patients did not receive any type of regional anaesthesia (noRA), 295 (48.7%) received a ssPNB, either femoral or femoral + sciatic nerve block, whereas 260 (42.7%) received a continuous local anaesthetic infusion (cPNB) defined as at least one peripheral nerve catheter as part of a femoral, lumbar plexus or adductor canal block, or an epidural catheter. Local infiltration analgesia (LIA) was infused in only 42 (6%) patients in the noRA group. In the cPNB group, seven (2%) patients received the local anaesthetic infusion for only 24 h due to the catheter being dislodged. In the remainder, the infusion was maintained for 48 (60% – 158/260) or 72 h (37% – 95/260). On POD1, POD2 and 1 month after surgery the continuous local anaesthetic infusion was a significant predictor of lower NRS compared with systemic analgesia or ssPNB (refer to multivariate logistic models in Table 2). This difference ceased to reach significance at three and 6 months after surgery (Fig. 2).
Table 2.
Predictive model for NRS more than 3 both at rest and incident on first postoperative day, second postoperative day and 1 month after total knee arthroplasty
| Dependent variable | Predictors | OR (95% CI) | P | Whole-model P | |
| POD1 | NRS > 3 (rest) | Preoperative pain | 1.447 (1.010 to 2.073) | 0.044 | 0.0001 |
| Continuous analgesia | 0.476 (0.454 to 0.905) | <0.001 | |||
| NRS > 3 (incident) | Preoperative NRS | 0.904 (0.830 to 0.984) | 0.020 | 0.0030 | |
| Continuous analgesia | 0.640 (0.453 to 0.904) | 0.011 | |||
| POD2 | NRS > 3 (rest) | Preoperative pain | 1.893 (1.300 to 2.758) | 0.001 | 0.0001 |
| Continuous analgesia | 0.567 (0.386 to 0.834) | 0.004 | |||
| NRS > 3 (incident) | Continuous analgesia | 0.629 (0.448 to 0.884) | 0.008 | 0.008 | |
| 1 month after surgery | NRS > 3 (rest) | No model | |||
| NRS > 3 (incident) | Male sex | 0.567 (0.392 to 0.821) | 0.003 | <0.0001 | |
| BMI | 0.944 (0.906 to 0.983) | 0.005 | |||
| Continuous analgesia | 0.616 (0.907 to 0.983) | 0.005 |
CI, confidence interval; NRS, numerical rating scale; OR, odds ratio; POD1, first postoperative day; POD2, second postoperative day.
Fig. 2.
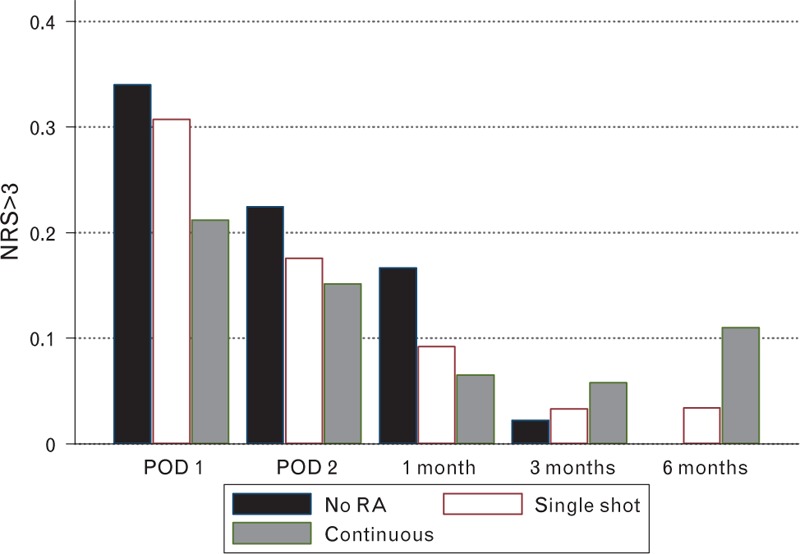
Fraction of patients reporting numerical rating scale more than 3.
No difference was found between intraoperative anaesthesia modes and any evaluated long-term outcome. Patients receiving general anaesthesia showed an overall higher incidence of postoperative adverse effects (P = 0.002) compared with regional anaesthesia (spinal or lumbar plexus + sciatic nerve block), including PONV (18% – 55/302 versus 7% – 23/299), and major events such as acute cardiac ischaemia (three in general anaesthesia group and none in regional anaesthesia group) and deep venous thrombosis (three in general anaesthesia and two in regional anaesthesia).
All centres involved in the study used a multimodal analgesia protocol, including administration of NSAIDs beginning with intraoperative ketorolac in 62%, paracetamol in 68% and opioids (including tramadol) in 56% given as required or as rescue. Intra-operative dexamethasone was given to only 98 (16%) (mean dose 6.3 ± 2.2 mg). Characteristics of multimodal analgesia with respect the adopted regional anaesthesia are reported in Table 3.
Table 3.
Perioperative management with respect to the use of multimodal analgesia in patients receiving single-shot peripheral nerve block, continuous peripheral nerve block or any type of regional anaesthesia
| Analgesia groups | NSAIDs, n (%) | Paracetamol, n (%) | Opioids, n (%) | LAI, n (%) | Dexamethasone, n (%) |
| noRA | 45 (90) | 44 (88) | 43 (82) | 42 (84) | 42 (84) |
| ssPNB | 203 (69) | 200 (68) | 216 (73) | – | 44 (14) |
| cPNB | 123 (47) | 168 (64) | 76 (29) | – | 12 (4) |
cPNB, continuous peripheral nerve block; noRA, any type of regional anaesthesia; ssPNB, single-shot peripheral nerve block.
Discussion
TKA is a complex procedure intended to improve the QOL. Unfortunately, it does not satisfy 20% of patients at 1 year after surgery and, unexpectedly, this percentage increases to 44% at 4 years after the procedure.9,10 The primary cause of dissatisfaction is PPSP.17,18 We report an incidence of PPSP of 21.6% 6 months after surgery (NRS > 3 and/or daily consumption of analgesic for knee pain), and an unchanged or even worsened QOL in 30.7%. Our results are consistent with previous reports.9,19
The main purpose of this study was to assess the influence of regional anaesthesia on the development of PPSP after TKA. We did not find any association between the type of anaesthesia and PPSP 6 months after surgery, even though continuous regional analgesia (both peripheral and epidural) significantly decreased pain in the early postoperative period up to 1 month compared with single-PNB. There was no difference in NRS between patients who were treated with ssPNB or without regional anaesthesia, with or without LIA. Taken together, these findings indicate the superiority of continuous techniques for postoperative analgesia, and that a ssPNB is not the best strategy for reducing postoperative pain and opioid consumption, the goals of fast-track perioperative care.
Our data suggest fewer postoperative complications in patients receiving regional anaesthesia compared with those receiving general. The superiority of regional anaesthesia in improving surgical outcome has been recently confirmed19–21; major complications after joint arthroplasty both unilateral and bilateral, were less common in all patient groups, irrespective of age and co-morbidity. Our data mainly show a reduction in the incidence of PONV, and the reduced risk of major complications is biased by the few cases (three cardiac ischaemia and five deep venous thromboses) that occurred during the study. Studies with the appropriate sample size are required to address this issue, but our data confirm the trend seen in previous large database studies.19–21
Some authors have recently questioned the role of continuous regional anaesthesia in the context of enhanced recovery after surgery: complications are a concern22,23 and even minor side effects, particularly motor block, can derail the fast-track approach. But even if all goes well, the positive impact of enhanced recovery is reduced if the quality of the long-term outcome is impaired, as it is in those who experience PPSP. Our study suggests that the benefits of a continuous RA technique are extended beyond the pharmacological half-life, since pain relief is maintained for up to 1 month, potentially influencing the long-term outcome. This could prompt a reconsideration of the role of continuous RA techniques, since the drawbacks of the immediate postoperative period may be overcome by the long-term benefits.
Pain at 1 month was found to be an independent risk factor for PPSP at 6 months, in keeping with previous reports.7 In our study, the use of continuous regional anaesthesia as a part of a multimodal analgesia regimen significantly reduced the opioid requirement in the early postoperative period, and provided better pain control up to 1 month after surgery, making a continuous RA technique the first choice. Unfortunately, the superior analgesic efficacy of continuous regional anaesthesia was no longer in evidence at 3 and 6 months. The hypothesis that regional anaesthesia has a protective effect on PPSP is confirmed by our study; continuous regional anaesthesia produces superior analgesia in the immediate postoperative period, and the benefit extends from the peri-operative period to support rehabilitation. The reason for the lack of evidence of benefit of both continuous regional analgesia and the other groups at 3 and 6 months may be related to the quality of rehabilitation. Typically, rehabilitation in the early postoperative days is limited by pain4,24 and is, therefore, dependent on the efficacy of postoperative analgesia. Beyond that, the success of TKA is strictly linked to rehabilitation, the standard of which varies according to the experience of the clinician. Rehabilitation after TKA has been defined as the most useful and least studied practice.25 Although it has a major impact on the global outcome it is often not investigated, and the confounding effect on published data may have been underestimated. The variability in the provision of physiotherapy may possibly hide clinically important differences in the analgesic techniques used in our study. Any attempt to overcome this bias will require a larger sample because of the low incidence of patients not receiving RA.
Our data also show other independent risk factors for PPSP. In common with earlier reports,12,14 we found that a younger age and a history of anxiety or depression, in addition to the pro-inflammatory status, led to a higher incidence of PPSP and a 30% worsened health-related QOL 6 months after surgery. Other important factors in dissatisfaction were a higher BMI and a lower ASA physical status. Some of these factors are linked to expectation of TKA. The refusal rate for second stage surgery in bilateral TKA was 36.9%, when patients’ expectations were unmet after the first intervention.26 A young and healthy patient with good baseline autonomy arguably displays a higher expectation towards the QOL and physical performance after surgery, which may sometimes be inconsistent with those provided by TKA. By contrast, an elderly patient with more comorbidities and severe arthritis will report a significant subjective relief with a smaller range of knee movement.27
We had previously investigated the association of the background inflammatory state and PPSP in minor surgery,28,29 and this was confirmed here. Inflammation is a key mechanism in postoperative pain and central sensitisation. The pro-inflammatory response to the surgical trauma is believed to be particularly intense in patients with a higher baseline inflammatory status,30,31 in whom pro-inflammatory and anti-inflammatory mechanisms are un-balanced by higher BMI, rheumatologic diseases or inflammatory bowel diseases. Further investigations are needed, but this is the first study, to our knowledge, suggesting such correlation.
The main strength of our study relies on the large sample size and in the prospective design. Our cohort is one of the largest ever presented in a study on PPSP after TKA, identifying a larger number of PPSP cases and allowing correlation with different types of anaesthesia and analgesia. The prospective nature of our study, together with the sample size improves on previous published reports on this topic.
A limitation of this study is the lack of a standardised postoperative analgesia protocol that could have better highlighted the effect of including different types of regional anaesthesia techniques. Our study was conceived as multicentre and observational, with each participating centre free to follow its own analgesic protocol. Nevertheless, the protocols in use in the five participating centres were broadly similar one to each other. Postoperative analgesia always included both paracetamol and NSAIDs, with opioid as rescue analgesic. Even if the multimodal protocols had included a broader spectrum of drugs (namely a larger use of dexamethasone),32,33 our sample was homogeneously treated with respect to postoperative analgesia, thus reducing the confounding effect on our endpoints.
We did not provide data on duration of hospital stay, nor on the use of the fast-track regimen. Although relevant, we did not include them in our design which was slanted towards long-term outcome. However, the correlation between length of hospital stay, the use of continuous techniques and long-term outcome is worthy of a future study.
We did not use specific tests to evaluate functional status and QOL (such as Western Ontario and McMaster Universities Ostearthritis Index or Short Form 36 Health Survey) because we consider them time-consuming for both patients and researchers. Given the number of evaluations planned during the study, such specific questionnaires would have probably reduced compliance with follow-up evaluation. We acknowledge that the veracity of our findings may be partially undermined, but our approach was to obtain a large amount of data on the primary endpoint (PPSP and regional anaesthesia) rather than on secondary outcomes. Although this might attract criticism, there is still the option to use validated questionnaires in future studies of non-analgesic outcomes.
In conclusion our prospective, observational, multicentre study demonstrated that continuous regional anaesthesia techniques significantly improve postoperative analgesia after TKA, maintaining superior pain relief for up to 1 month after surgery compared with multimodal analgesia without regional anaesthesia or with a ssPNB. We also found that PPSP was present 6 months after surgery in 21.6% of patients irrespective of the type of anaesthesia and analgesia. We identified younger age, anxiety or depression, and pre-inflammatory status as independent risk factors for PPSP with a worsened QOL. Future studies should address the correlation between the type and timing of continuous regional anaesthesia and long-term rehabilitation to extend the benefit of analgesia over the first month.
Supplementary Material
Acknowledgements relating to this article
Assistance with the study: BBraun organised the meeting that started the study, conducted audits of the study and promoted contacts between the members of the group.
Sponsorship and funding: none in addition to the above.
Conflicts of interest: none.
Presentation: preliminary data were presented to the SIMPAR Meeting (Rome, 2015) and the ASA meeting (new Orleans 2014)
The ALICE Group included:
Astrid Ursula Behr, MD: Department of Medicine, Anaesthesiology and Intensive Care, University of Padua, Padua, Italy
Valentina Bellini: Department of Anaesthesiology, Intensive Care and Pain Therapy, University Hospital of Parma, Parma, Italy
Silvia Bettinelli: Department of Anaesthesiology, Intensive Care and Pain Therapy, University Hospital of Parma, Parma, Italy
Mirko Binda: Department of Anaesthesiology, Intensive Care and Pain Therapy, Ospedale di Circolo, Varese, Italy
Giorgio Danelli, MD: Department of Anaesthesiology and Intensive Care, Arcispedale Santa Maria nuova, Azienda Ospedaliera Reggio Emilia, Italy
Luisa Fedele, MD: Department of Anaesthesiology and Intensive Care, ASST-Rhodense, Garbagnate Milanese, Milano, Italy
Daniela Ghisi: Department of Anaesthesia and Postoperative Intensive Care, Istituto Ortopedico Rizzoli, Bologna, Italy
Christian Lanza: Department of Anaesthesiology, Intensive Care and Pain Therapy, Ospedale di Circolo, Varese, Italy
Maurizio Marchesini, MD: Department of Anaesthesiology, Intensive Care and Pain Therapy, University Hospital of Parma, Parma, Italy
Footnotes
Published online 1 August 2017
References
- 1.Grosu I, Lavand’homme P, Thienpont E. Pain after knee arthroplasty: an unresolved issue. Knee Surg Sports Traumatol Arthrosc 2014; 22:1744–1758. [DOI] [PubMed] [Google Scholar]
- 2.Bauer M, Pogatzki-Zahn EM, Zahn PK. Regional analgesia techniques for total knee replacement. Curr Opin Anesthesiol 2014; 27:501–506. [DOI] [PubMed] [Google Scholar]
- 3.Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthroplasty 2014; 29:2224–2229. [DOI] [PubMed] [Google Scholar]
- 4.Ilfeld BM, Le LT, Meyer RS, et al. Ambulatory continuous femoral nerve blocks decrease time to discharge readiness after tricompartment total knee arthroplasty: a randomized, triple-masked, placebo-controlled study. Anesthesiology 2008; 108:703–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012; 56:357–364. [DOI] [PubMed] [Google Scholar]
- 6.Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg 2014; 118:1370–1377. [DOI] [PubMed] [Google Scholar]
- 7.Perkins FM, Kelhet H. Chronic pain as an outcome from surgery. A review of predictive factors. Anesthesiology 2000; 93:1123–1133. [DOI] [PubMed] [Google Scholar]
- 8.Sachs D, Cunha FQ, Pooleb S, et al. Tumour necrosis factor-a, interleukin-1b and interleukin-8 induce persistent mechanical nociceptor hypersensitivity. Pain 2002; 96:89–97. [DOI] [PubMed] [Google Scholar]
- 9.Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain 2011; 152:566–572. [DOI] [PubMed] [Google Scholar]
- 10.Puolakka PA, Rorarius MG, Roviola M, et al. Persistent pain following knee arthroplasty. Eur J Anaesthesiol 2010; 27:455–460. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; 89:780–785. [DOI] [PubMed] [Google Scholar]
- 12.Liu SS, Buvanendran A, Rathmell JP, et al. A cross-sectional survey on prevalence and risk factors for persistent postsurgical pain 1 year after total hip and knee replacement. Reg Anesth Pain Med 2012; 37:415–422. [DOI] [PubMed] [Google Scholar]
- 13.Baker PN, Van der Meulen JH, Lewsey J, et al. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the national joint registry for England and Wales. J Bone Joint Surg Br 2007; 89:893–900. [DOI] [PubMed] [Google Scholar]
- 14.Scott CEH, Howie CR, MacDonald D, et al. Predicting dissatisfaction following total knee replacement; a prospective study of 1217 patients. J Bone Joint Surg Br 2010; 92:1253–1258. [DOI] [PubMed] [Google Scholar]
- 15.Von Elm E, Altman DG, Egger M, et al. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61:344–349. [DOI] [PubMed] [Google Scholar]
- 16.Singh JA, Lewallen DG. Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care Res (Hoboken) 2014; 66:897–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002; 183:630–641. [DOI] [PubMed] [Google Scholar]
- 18.Carli F, Clemente A. Regional anesthesia and enhanced recovery after surgery. Minerva Anestesiol 2014; 80:1228–1233. [PubMed] [Google Scholar]
- 19.Memtsoudis SG, Rasul R, Suzuki S, et al. Does the impact of the type of anesthesia on outcomes differ by patient age and comorbidity burden? Reg Anesth Pain Med 2014; 39:112–119. [DOI] [PubMed] [Google Scholar]
- 20.Memtsoudis SG, Poeran J, Cozowicz C, et al. The impact of peripheral nerve blocks on perioperative outcome in hip and knee arthroplasty – a population-based study. Pain 2016; 157:2341–2349. [DOI] [PubMed] [Google Scholar]
- 21.Stundner O, Chiu YL, Sun X, et al. Comparative perioperative outcomes associated with neuraxial versus general anesthesia for simultaneous bilateral total knee arthroplasty. Reg Anesth Pain Med 2012; 37:638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manassero A, Ugues S, Coletta G, et al. Spinal epidural abscess: stay focused, stay tuned! A clinical report with negative neurological outcome from the ‘Italian Registry of Complications Associated with Regional Anesthesia – RICALOR’. Minerva Anestesiol 2016; 82:492–493. [PubMed] [Google Scholar]
- 23.Allegri M, Bugada D, Grossi P, et al. Italian Registry of Complications associated with Regional Anesthesia (RICALOR). An incidence analysis from a prospective clinical survey. Minerva Anestesiol 2016; 82:392–402. [PubMed] [Google Scholar]
- 24.Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999; 91:8–15. [DOI] [PubMed] [Google Scholar]
- 25.Rankin EA, Alarcon GS, Chang RW, et al. NIH consensus development conference on total knee replacement. 8–10 December 2003. [Google Scholar]
- 26.Sesen H, Demirkale I, Karaduman M, et al. Why two-thirds of patients accepted the second session in staged bilateral total knee arthroplasty: a prospective analysis of 111 patients. Knee Surg Sports Traumatol Arthrosc 2015; 23:3585–3590. [DOI] [PubMed] [Google Scholar]
- 27.Liu SS, Wu CL. The effect of analgesic technique on postoperative patient-reported outcomes including analgesia: a systematic review. Anesth Analg 2007; 105:789–808. [DOI] [PubMed] [Google Scholar]
- 28.Bugada D, Lavand’homme P, Ambrosoli AL, et al. Effect of preoperative inflammatory status and comorbidities on pain resolution and persistent postsurgical pain after inguinal hernia repair. Mediators Inflamm 2016; 2016:5830347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bugada D, Lavand’homme P, Ambrosoli AL, et al. Effect of postoperative analgesia on acute and persistent postherniotomy pain: a randomized study. J Clin Anesth 2015; 27:658–664. [DOI] [PubMed] [Google Scholar]
- 30.Grosu I, de Kock M. New concepts in acute pain management: strategies to prevent chronic postsurgical pain, opioid-induced hyperalgesia, and outcome measures. Anesthesiol Clin 2011; 29:311–327. [DOI] [PubMed] [Google Scholar]
- 31.Omoigui S. The biochemical origin of pain – proposing a new law of pain: the origin of all pain is inflammation and the inflammatory response – a unifying law of pain. Med Hypotheses 2007; 69:70–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lunn TH, Kristensen BB, Andersen LØ, et al. Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty: a randomized, placebo-controlled trial. Br J Anaesth 2011; 106:230–238. [DOI] [PubMed] [Google Scholar]
- 33.Backes JR, Bentley JC, Politi JR, et al. Dexamethasone reduces length of hospitalization and improves postoperative pain and nausea after total joint arthroplasty: a prospective, randomized controlled trial. J Arthroplasty 2013; 28:11–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


