Abstract
Background
India is considering the scale-up of the Xpert MTB/RIF assay for detection of tuberculosis (TB) and rifampicin resistance. We conducted an economic analysis to estimate the costs of different strategies of Xpert implementation in India.
Methods
Using a decision analytical model, we compared four diagnostic strategies for TB patients: (i) sputum smear microscopy (SSM) only; (ii) Xpert as a replacement for the rapid diagnostic test currently used for SSM-positive patients at risk of drug resistance (i.e. line probe assay (LPA)); (iii) Upfront Xpert testing for patients at risk of drug resistance; and (iv) Xpert as a replacement for SSM for all patients.
Results
The total costs associated with diagnosis for 100,000 presumptive TB cases were: (i) US$ 619,042 for SSM-only; (ii) US$ 575,377 in the LPA replacement scenario; (iii) US$ 720,523 in the SSM replacement scenario; and (iv) US$ 1,639,643 in the Xpert-for-all scenario. Total cohort costs, including treatment costs, increased by 46% from the SSM-only to the Xpert-for-all strategy, largely due to the costs associated with second-line treatment of a higher number of rifampicin-resistant patients due to increased drug-resistant TB (DR-TB) case detection. The diagnostic costs for an estimated 7.64 million presumptive TB patients would comprise (i) 19%, (ii) 17%, (iii) 22% and (iv) 50% of the annual TB control budget. Mean total costs, expressed per DR-TB case initiated on treatment, were lowest in the Xpert-for-all scenario (US$ 11,099).
Conclusions
The Xpert-for-all strategy would result in the greatest increase of TB and DR-TB case detection, but would also have the highest associated costs. The strategy of using Xpert only for patients at risk for DR-TB would be more affordable, but would miss DR-TB cases and the cost per true DR-TB case detected would be higher compared to the Xpert-for-all strategy. As such expanded Xpert strategy would require significant increased TB control budget to ensure that increased case detection is followed by appropriate care.
Introduction
According to the 2015 World Health Organization (WHO) Global TB Report, India has the highest tuberculosis (TB) burden in the world. In 2015, an estimated 2.8 million people in India developed active TB, of which approximately 59% were diagnosed [1]. 28,876 patients received a laboratory-confirmed MDR-TB diagnosis, which is approximately one third of the estimated total number of MDR-TB cases [1]. Improving the detection of active TB and of MDR-TB is among the top priorities of the Revised National TB Control Program (RNTCP) [2], in line with the WHO End TB Strategy to improve patient-centered TB care and prevention.
The Xpert MTB/RIF assay (hereafter referred to as Xpert) for the diagnosis of TB and DR-TB offers great promise as a tool for TB control in India. The WHO-endorsed assay has greater sensitivity for TB detection than sputum smear microscopy (SSM) [3], high accuracy for the detection of rifampicin resistance [4], and provides a diagnosis of TB and MDR-TB from a single sample within 2 hours. Furthermore, a previous economic evaluation found Xpert to be cost-effective as a replacement for SSM in India [5], with the benefit of increased case detection. A multisite, phased implementation study conducted to collect evidence for the scale-up of the Xpert assay for TB and MDR-TB diagnosis in India found that the proportion of bacteriologically-confirmed TB cases identified, out of the presumptive TB cases tested, increased by 33% (95% CI 16–52%), while the detection of all patients diagnosed with bacteriologically-confirmed or clinically-diagnosed pulmonary TB, combined, increased by 11% (95% CI 3–21%) compared to SSM [6,7].
Although Xpert has been shown to be easy to implement, and is potentially cost-effective and successful in increasing the detection of TB and MDR-TB in India [6,7], Xpert access and uptake in India have been hindered by issues related to cartridge cost, procurement and supply chain management, a lack of engagement of the private sector (the first point of contact with the healthcare system for about 70% of patients in India), and a major national TB control program (NTP) financial deficit [8,9]. A country-wide implementation of Xpert would require a considerable increase in the NTP budget [10], and the projected, increased costs for TB diagnosis and treatment of additional, identified TB and MDR-TB cases through Xpert scale-up may well exceed the available budget and compete with other cost-effective health interventions [11]. For these reasons, it is critical to explore the benefits and trade-offs of different strategies to Xpert implementation in order to inform decisions about the scale-up of the Xpert assay in India. We conducted an economic analysis to determine the per-patient and overall costs of diagnosing and treating TB and rifampicin-resistant TB given different diagnostic scenarios.
Methods
Overview
We developed a decision analytical model to simulate a cohort of patients who report to public health facilities in India with symptoms or signs suggestive of TB and require diagnostic testing for pulmonary TB [7]. We compared four different scenarios that consider different combinations of diagnostic tests and the target population, or sub-population, for each test. True and false positive (TP/FP) and true and false negative (TN/FN) cases were estimated for all scenarios, assuming that the tests perform with reported sensitivity and specificity (Table 1) [3,4,12,13]. We estimated the total costs (in 2013 US dollars) of diagnosing and treating TB and rifampicin-resistant TB for the cohort, as well as average costs per presumptive TB patient tested, per true TB case and per rifampicin-resistant TB case detected and initiated on treatment. The primary analysis was conducted from the perspective of a public, TB health care provider. We also estimated the impact of the total costs of each scenario on the national budget for TB control [1].
Table 1. Model parameters.
| Parameter | Point estimate | Range for deterministic sensitivity analysis | ||
|---|---|---|---|---|
| Low | High | Source | ||
| Prevalence among simulated cohort | ||||
| Proportion of patients known to have tuberculosis who require drug resistance testing ("MDR-suspect") | 0.0245 | 0.000 | 0.0254 | Sachdeva et al. 2014 [7] |
| Proportion of presumptive TB patients previously treated for TB | 0.168 | 0.019 | 0.3522 | Sachdeva et al. 2014 [7]; average and range observed across sites |
| Prevalence of true PTB among new presumptive TB patients | 0.15 | 0.08 | 0.23 | Assumption |
| Prevalence of true PTB among previously treated presumptive TB patients | 0.266 | 0.183 | 0.3982 | Assumption |
| Prevalence of RIF resistance among new patients | 0.022 | 0.019 | 0.0260 | WHO report 2014 [1] |
| Prevalence of RIF resistance among previously treated patients and DR-suspects | 0.150 | 0.110 | 0.1900 | WHO report 2014 [1] |
| Diagnostic test accuracy | ||||
| Sensitivity of Xpert MTB/RIF for diagnosing TB | 0.89 | 0.85 | 0.92 | Steingart et al. 2014 [4] |
| Specificity of Xpert MTB/RIF for diagnosing TB | 0.99 | 0.98 | 0.99 | Steingart et al. 2014 [4] |
| Sensitivity of Xpert MTB/RIF for Rif detection | 0.95 | 0.90 | 0.97 | Steingart et al. 2014 [4] |
| Specificity of Xpert MTB/RIF for Rif detection | 0.98 | 0.97 | 0.99 | Steingart et al. 2014 [4] |
| Sensitivity of sputum smear microscopy (ZN) | 0.62 | 0.44 | 0.79 | Steingart et al. 2006 [12] |
| Specificity of sputum smear microscopy (ZN) | 0.98 | 0.96 | 1.00 | Steingart et al. 2006 [12] |
| Sensitivity of LPA in detecting rifampicin resistance | 0.99 | 0.96 | 1.00 | Bwanga et al. 2009 [26] |
| Specificity of LPA in detecting rifampicin resistance | 0.99 | 0.98 | 1.00 | Bwanga et al. 2009 [26] |
| Sensitivity of clinical diagnosis in case found negative sputum smear microscopy | 0.160 | 0.10 | 0.22 | Vassall 2011[5] |
| Alternative source for Sensitivity of clinical diagnosis in case found negative sputum smear microscopy | 0.610 | Walusimbi 2013 [24] | ||
| Specificity of clinical diagnosis in case found negative sputum smear microscopy | 0.942 | 0.93 | 0.97 | Vassall 2011[5] |
| Alternative source for specificity of clinical diagnosis in case found negative sputum smear microscopy | 0.690 | Walusimbi 2013 [23] | ||
| Proportion of sputum smear negative patients getting CXR | 0.037 | 0 | 1 | Vassall 2011[5] |
| Ratio of proportion of Xpert-negative patients who get CXR, compared to proportion of smear-negative | 0.5 | 0 | 1 | Assumption |
| Proportion of Xpert positive patients who are smear negative | 0.36 | 0.355 | 0.368 | Sachdeva et al. 2014 [7] |
| Diagnostic test unit costs (in US$ 2013) | ||||
| Cost of sputum smear microscopy (per patient tested) | 0.83 | 0.60 | 1.10 | Microcosting study. Rupert et al. 2017 [15] |
| Cost of Xpert testing, per patient tested | 13.17 | 12.06 | 14.72 | Microcosting study. Rupert et al. 2017 [15] |
| Cost of liquid culture, per patient tested | 13.42 | 10.51 | 16.21 | Microcosting study. Rupert et al. 2017 [15] |
| Cost of line probe assay for DST, per patient tested (1) | 21.34 | 19.50 | 23.07 | Microcosting study. Rupert et al. 2017 [15]; adjusted for 2.2% error rate |
| Cost of antibiotic trial in clinical diagnosis | 3.86 | 3.86 | 3.86 | Vassall 2011[5] |
| Cost of CXR | 4.0 | 2.98 | 5.00 | WHO planning and budgeting tool [17] |
| Cost of clinical diagnosis = cost of antibiotic trial in all patients + cost of CXR multiplied by the proportion of patients getting CXR | ||||
| Treatment costs | ||||
| Full first-line regimen (2RH/4EHRZ) | $148 | $93 | $188 | S1 |
| Full first-line retreatment regimen | $189 | $185 | $305 | S1 |
| Second-line standard regimen, average for 24 months | $5,812 | $4,204 | $7,421 | S1; Fitzpatrick 2012 [21] |
| Number of weeks on first-line treatment until confirmatory results of LPA are returned in new Xpert RIF positive patients | 2.5 | Assumption | ||
| Loss to follow-up before treatment initiation (3) | ||||
| Proportion of sputum smear positive patients not starting treatment in the baseline | 0.092 | 0 | 0.20 | Sachdeva et al. 2014 [7] |
| Proportion of bacteriologically positive TB patients not starting treatment in the intervention phase | 0.099 | 0 | 0.20 | Sachdeva et al. 2014 [7] |
| Proportion clinically diagnosed TB patients not starting treatment | 0 | Assumption | ||
| Additional initial default in DR-TB patients | 0.10 | 0 | 0.2 | Sachdeva et al. 2014 [7] |
Population
The simulated population represented adult patients requiring diagnostic testing for TB, rifampicin-resistant TB or both. In the primary analysis, the cohort characteristics were stipulated as observed in the implementation study [7], except for the prevalence of bacteriologically-confirmed (culture positive) pulmonary TB, which was adapted to the national average (15% in new patients and 27% in patients previously treated for TB) in order to make the conclusion more attributable to the national program and not just to the areas included in the implementation study. In the implementation study [7], the proportion of presumptive TB patients previously treated for TB, out of all patients with presumptive TB was 16.8% (11,922/70,556) and the prevalence of rifampicin resistance was 5.6% in new and 24.6% in previously treated TB patients. Two percent of the cohort comprised TB patients requiring drug resistance testing because of treatment failure (DR-TB suspects). HIV-infection was not considered due to low prevalence of HIV in India. See Supplement S1 File for further details.
Diagnostic scenarios
Scenario 1. Baseline: Sputum smear microscopy (SSM) only
The baseline scenario represents the recommended practice in India [14], with SSM being the primary diagnostic tool for screening of all presumptive TB patients followed by line probe assay (LPA) screening of patients at increased risk for MDR-TB as recommended by RNTCP. Briefly, SSM was performed on two samples from all presumptive TB patients. Patients with ≥1 positive SSM were considered a TB case and required TB treatment. SSM negative patients were clinically evaluated following the RNTCP algorithm (Fig A of S1 File). For patients with two negative smears, the recommendation consisted of 10–14 days of antibiotics followed by two repeat SSM examinations if cough persisted. If these SSM results were negative, TB treatment may be initiated based on a chest x-ray (CXR) suggestive of TB [7]. In the primary analysis we attempted to closely reflect actual practice, and thus assumed that all patients received an antibiotic trial, though only a portion of patients received a CXR [4,13]. In a sensitivity analysis, the NTP’s newly-proposed algorithm that includes a CXR for all SSM negative patients with presumptive TB (in locations where Xpert is not accessible) was explored.
To diagnose rifampicin resistance, the sputum of SSM positive TB patients at increased risk for MDR was tested by LPA. In the model, in all scenarios, patients at increased risk for MDR included TB patients who failed first-line treatment (DR-TB suspects) as well as patients with a history of TB treatment in the past. This was chosen to stay close to the RCNTP guidelines which define high-risk TB cases as those TB cases with previous history of anti TB treatment, TB cases on treatment with positive sputum smear result at any follow up smear examination, diagnosed TB cases with HIV-co-infection and all pulmonary TB cases who are contacts of a known MDR TB case [9]. Patients with SSM negative (i.e. clinically diagnosed) TB were not further tested for drug resistance. Patients with a rifampicin-resistant LPA result were eligible for second-line TB treatment, according to RNTCP guidelines [9]. Patients newly diagnosed with TB were started the standard first-line, 6-month treatment regimen (Cat I), and those previously treated were started on a first-line, 8-month re-treatment regimen (Cat II).
Scenario 2. Xpert MTB/RIF as a replacement for LPA testing
This scenario was identical to the baseline scenario, except that the Xpert assay replaced LPA for DST following SSM, and thus was only applied to SSM-positive TB patients at increased risk for MDR.
Scenario 3. Upfront Xpert MTB/RIF testing for presumptive TB patients at increased risk of MDR
In the third scenario, presumptive TB patients at increased risk for MDR-TB (as defined in scenario 1) received upfront Xpert testing, rather than SSM. New patients were tested with SSM as in the baseline scenario. Thus, if new patients were diagnosed with pulmonary TB, they were not subjected to drug resistance testing.
Scenario 4. Upfront Xpert MTB/RIF for all presumptive TB patients
In the upfront Xpert-for-all scenario, all presumptive TB patients were tested up-front by Xpert, instead of SSM, regardless of previous history of TB. This scenario is in line with WHO recommendations [5]. If positive for MTB by Xpert testing, the patient was considered a TB case and required TB treatment. For presumptive TB cases with a negative Xpert result for MTB, we assumed that with significantly higher detection rates with Xpert, the proportion of patients subjected to the clinical diagnostic process would be half of those undergoing the clinical diagnostic process following SSM (the baseline scenario) [7]. In the sensitivity analysis, we explored the possibility of fewer patients being subjected to clinical diagnosis after a negative Xpert result.
After a rifampicin-sensitive Xpert result, a first-line treatment regimen was started (Cat I or II, according to retreatment status). In case of a rifampicin-resistant result for previously treated TB cases, second-line treatment was indicated without further diagnostic confirmation. In new cases, a sputum sample for confirmatory DST by LPA was required. Xpert MTB-positive, SSM-negative patients, assumed to be 36% [7], for which direct LPA cannot be done on the patient specimen, required a culture followed by an LPA on the isolate. Second-line treatment was started and changed to first-line treatment if MDR was not confirmed by LPA.
Costs of diagnostic testing
An observational micro-costing study (or ‘bottom-up’ approach) was conducted at seven study sites to determine the cost of each bacteriological test (SSM, Xpert, LPA, culture, DST) per patient tested. The results are reported elsewhere [15]. The costs of clinical diagnosis were taken from earlier studies conducted in India [4]. The costs of TB treatment regimens were obtained by applying country-specific cost estimates, including cost of drugs, as well as tests and visits required for treatment monitoring [16–24] (Table 1; A detailed example is available in the Supplement S1 File).
Outcome measures
The outcomes calculated by the model were the number of TB cases detected and initiated on TB treatment, divided into true positive and false positive cases as determined by phenotypic methods. Similarly, MDR cases detected and initiated on treatment were divided in true positive and false positive cases. For the primary analysis, estimates for primary loss to follow-up between bacteriological TB diagnosis and treatment initiation were taken from the two arms of the Xpert implementation study (9.2 and 9.9% in the baseline and Xpert-for-all scenario, respectively). Loss to follow-up for DR-TB cases before treatment initiation was also estimated to be 10% based on the previous implementation study [7]. To calculate the impact of the rollout of different scenarios to the whole country on the national budget for TB control, we assumed 610 presumptive TB patients were tested per 100,000 people per year, as observed in the implementation study [7]. Assuming a population of 1,252 million and a TB control budget of 252 million US$ [1], 7,637,200 presumptive TB patients would be tested per year.
Sensitivity analyses
Deterministic sensitivity analyses were conducted to explore how assumptions and variations in the parameter estimates affected the total costs of different scenarios, including variation in the epidemiological parameters, assumptions about test accuracy, as well as the costs of diagnostic tests and treatment. Additionally, the assumptions about the use and interpretation (i.e. sensitivity and specificity) of CXR were explored in more detail, as little data is available regarding the proportion of patients receiving CXR in different diagnostic algorithms, despite the fact that the availability of CXR results could substantially affect clinicians’ decisions regarding empiric therapy and affect diagnostic costs. In the primary analysis, all patients with negative bacteriology (SSM) results were clinically evaluated, though only 4% of these patients received a CXR as part of their TB clinical assessment. This estimate was based on previous observations [4, 13], and resulted in low sensitivity and high specificity of the clinical diagnostic algorithm. In a sensitivity analysis, we explored the effect of different clinical diagnostic scenarios on cost and case detection in patients negative for MTB by bacteriological tests. We also explored the effect of increasing the proportion of these patients receiving a CXR to 100%, which would increase the sensitivity and lower the specificity [10].
Ethics
Ethical approval was not obtained for this study, as only secondary data were used in these analyses.
Results
Cohort of 100,000 persons
The proportion of true pulmonary TB cases diagnosed and initiated on treatment among presumptive TB patients was 62% in both the SSM-only and LPA replacement scenarios, 67% in the SSM replacement scenario, and 81% in the Xpert-for-all scenario (Table 2). The total number of patients on TB treatment, in a cohort of 100,000 persons, was highest in the Xpert-for-all scenario (16,076), but the proportion of false-positive TB diagnoses was lowest in this scenario. Detection of true rifampicin-resistant TB cases was highest (73%) in the Xpert-for-all scenario, compared to SSM-only (48%), Xpert as an LPA replacement (46%) and Xpert as a SSM replacement (59%).
Table 2. TB and rifampicin resistant-TB cases detected and initiated on treatment by each of the 4 diagnostic strategies, in a cohort 100,000 persons.
| TB case detection | DR-TB case detection | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| True TB cases detected and initiated on treatment (TP) | False TB cases detected and initiated on treatment (FP) | Total number on TB treatment (TP+FP) | True DR-TB cases detected and initiated on treatment (TP) | False DR-TB cases detected and initiated on treatment (FP) | % of all persons with DR-TB diagnosis | Total number on DR-TB treatment (TP+FP) | |||
| Diagnostic Strategy* | n | (%**) | n | n | n | (%) | n | % | n |
| 1. SSM Only | 10,188 | 62% | 5,365 | 15,553 | 620 | 48% | 36 | 5% | 655 |
| 2. Xpert MTB/RIF as a replacement for LPA testing | 10,188 | 62% | 5,365 | 15,553 | 595 | 46% | 71 | 11% | 665 |
| 3. Xpert MTB/RIF as a replacement for SSM for patients with previous TB history | 11,016 | 67% | 4,969 | 15,985 | 762 | 59% | 99 | 12% | 861 |
| 4. Xpert MTB/RIF for all patients | 13,380 | 81% | 2,697 | 16,076 | 945 | 73% | 101 | 10% | 1,046 |
TP = true positive; DR-TB = drug-resistant TB, i.e. rifampicin-resistant; FP = false positive; SSM = sputum smear microscopy
*Scenario 1: Perform SSM. If SSM positive and patient has been previously treated for TB, use LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 2: Perform SSM. If SSM positive and patient has been previously treated for TB, use Xpert in place of LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 3: Perform SSM only for patients not at DR-TB risk. Perform Xpert MTB/RIF for patient has been previously treated for TB.
Scenario 4: Perform Xpert MTB/RIF for all patients, regardless of DR-TB risk.
**Out of 16,492 true pulmonary TB cases among presumptive TB patients and 1,288 rifampicin resistant cases in the cohort
The diagnostic costs for the diagnosis of TB and rifampicin-resistant TB in a cohort of 100,000 persons (Table 3) were: US$ 619,042 in the SSM-only scenario, US$ 575,377 in the LPA replacement scenario, US$ 720,523 in the SSM replacement scenario, and US$ 1,639,643 in the Xpert-for-all scenario. In all scenarios, diagnostic costs were a minor proportion (8–16%) of total cohort costs, of which treatment costs were the largest component. Total cohort costs increased by 46% in the Xpert-for-all scenario and 19% in the LPA replacement scenario compared to SSM-only. This increase is largely due to the increased costs associated with second-line treatment of the additional rifampicin-resistant TB patients identified upon up-front Xpert testing. The incremental total cohort cost per true TB case initiated on treatment, compared to baseline was US$ 1040 for scenario 4, and $ 1614 for scenario 3 (Table 4).
Table 3. Total diagnostic costs and treatment costs to test 100,000 patients, for 4 diagnostic strategies (Cost in US$2013).
| Total diagnostic costs** | % of Total cohort costs | Patients on TB treatment (TP+FP), any regimen | Patients on DR-TB treatment (TP+FP) | Costs for 1st line treatment | Costs for 2nd line treatment | Total Treatment costs | % of Total cohort costs | Total cohort costs | Incremental total cohort costs compared to baseline | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Strategy* | US$ 2013 | n | n | US$ 2013 | US$ 2013 | US$ 2013 | US$ 2013 | US$ 2013 | % | ||
| 1. Baseline: SSM. Clinical diagnosis. If prev treated, LPA if SSM+ or Culture/LPA/DST if SSM negative. | 619,042 | 9% | 15,553 | 655 | 2,747,408 | 3,807,122 | 6,554,530 | 91% | 7,173,573 | ||
| 2. Baseline: SSM. Clinical diagnosis. If prev treated, Xp to diagnose Rif Res if SSM+ | 575,377 | 8% | 15,553 | 665 | 2,745,435 | 3,867,745 | 6,613,180 | 92% | 7,188,556 | 14,984 | 0.2% |
| 3. Xpert MTB/RIF for presumptive TB cases with prev TB history. SSM for new patients. | 720,523 | 8% | 15,985 | 861 | 2,782,695 | 5,006,646 | 7,789,340 | 92% | 8,509,863 | 1,336,290 | 19% |
| 4. Xpert MTB/RIF for all patients | 1,639,643 | 16% | 16,076 | 1,046 | 2,771,662 | 6,081,091 | 8,852,753 | 84% | 10,492,396 | 3,318,823 | 46% |
TP = true positive; DR-TB = drug-resistant TB, i.e. rifampicin-resistant; FP = false positive; SSM = sputum smear microscopy
*Scenario 1: Perform SSM. If SSM positive and patient has been previously treated for TB, use LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 2: Perform SSM. If SSM positive and patient has been previously treated for TB, use Xpert in place of LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 3: Perform SSM only for patients not at DR-TB risk. Perform Xpert MTB/RIF for patient has been previously treated for TB.
Scenario 4: Perform Xpert MTB/RIF for all patients, regardless of DR-TB risk.
**Total diagnostic costs include costs for all bacteriological TB and resistance tests and for CXR and/or antibiotic trial
Table 4. Incremental cohort and diagnostic costs per true TB case detected and treated, for 4 diagnostic strategies (Cost in US$2013).
| Total cohort costs | Total cohort diagnostic costs** | Total cohort treatment costs | True TB cases detected and initiated on treatment (TP) | Incremental True TB cases compared to baseline | Incremental total cohort costs compared to baseline | Incremental total diagnostic cost (US$2013) per incremental true TB case detected and initiated on treatment. Compared to: | Incremental total cohort cost (US$2013) per incremental True TB cases detected and initiated on treatment. Compared to: | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Strategy* | US$ 2013 | US$ 2013 | US$ 2013 | n | n | US$ 2013 | Baseline | Strategy 3† | Baseline | Strategy 3† |
| 1. Baseline: SSM. Clinical diagnosis. If prev treated, LPA if SSM+ or Culture/LPA/DST if SSM negative. | 7,173,573 | 619,042 | 6,554,530 | 10,188 | ||||||
| 2. Baseline: SSM. Clinical diagnosis. If prev treated, Xp to diagnose Rif Res if SSM+ | 7,188,556 | 575,377 | 6,613,180 | 10,188 | - | 14,984 | n.a. | n.a. | ||
| 3. Xpert MTB/RIF for presumptive TB cases with prev TB history. SSM for new patients. | 8,509,863 | 720,523 | 7,789,340 | 11,016 | 828 | 1,336,290 | 123 | 1614 | ||
| 4. Xpert MTB/RIF for all patients | 10,492,396 | 1,639,643 | 8,852,753 | 13,380 | 3,192 | 3,318,823 | 320 | 389 | 1040 | 839 |
TP = true positive; DR-TB = drug-resistant TB, i.e. rifampicin-resistant; SSM = sputum smear microscopy
*Scenario 1: Perform SSM. If SSM positive and patient has been previously treated for TB, use LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 2: Perform SSM. If SSM positive and patient has been previously treated for TB, use Xpert in place of LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 3: Perform SSM only for patients not at DR-TB risk. Perform Xpert MTB/RIF for patient has been previously treated for TB.
Scenario 4: Perform Xpert MTB/RIF for all patients, regardless of DR-TB risk.
**Total diagnostic costs include costs for all bacteriological TB and resistance tests and for CXR and/or antibiotic trial
† Strategy 3 being the next most effective option
Population of 7.64 million
When applied to the whole country (Table 5), the total costs for diagnosis of TB and rifampicin resistance (not including treatment) among an estimated 7.64 million presumptive TB patients were highest for the Xpert-for-all scenario. Total diagnostic costs would comprise 19% of the annual TB control budget for SSM-only, 17% for the LPA replacement scenario, 22% for the SSM replacement scenario, and 50% for the Xpert-for-all scenario. The expanded Xpert deployment and usage across different scenarios, would lead to an increase in the case detection of TB, more significantly rifampicin resistant TB cases, which would warrant a substantial increase in budget for initiating the detected cases with appropriate treatment regimen. In the Xpert-for-all scenario the cost for 1st line treatment would increase minimally compared to SSM-only. However, cost for 2nd line treatment would increase by 59%, resulting in an overall expected 22% increase in total treatment costs. Compared to the SSM-only scenario, the Xpert-for-all scenario is predicted to result in a $253 million increase in total national costs for TB diagnosis and treatment.
Table 5. Total diagnostic costs and treatment costs under the TB control program for 4 diagnostic strategies.
| Number of patients tested | Total diagnostic costs | Diagnostic costs as % of the budget** | Total number on TB treatment: TP+FP | 1st line treatment | 2nd line treatment | Total number on DR-TB treatment: TP+FP | Total treatment costs | Total costs | |
|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Strategy* | n [millions/year] | Million US$ 2013 | (%) | n [millions/year] | Million US$ 2013 | Million US$ 2013 | n [millions/year] | Million US$ 2013 | Million US$ 2013 |
| 1. SSM Only | 7.64 | $47.3 | 19% | 1.19 | $210 | $291 | 0.050 | $453 | $548 |
| 2. Xpert MTB/RIF as a replacement for LPA testing | 7.64 | $43.9 | 17% | 1.19 | $210 | $295 | 0.051 | $461 | $549 |
| 3. Xpert MTB/RIF as a replacement for SSM for patients with previous TB history | 7.64 | $55.0 | 22% | 1.22 | $213 | $382 | 0.066 | $540 | $650 |
| 4. Xpert MTB/RIF for all patients | 7.64 | $125.2 | 50% | 1.23 | $212 | $464 | 0.080 | $552 | $801 |
All costs are in millions, US$ 2013
TP = true positive; DR-TB = drug-resistant TB, i.e. rifampicin-resistant; FP = false positive; SSM = sputum smear microscopy
*Scenario 1: Perform SSM. If SSM positive and patient has been previously treated for TB, use LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 2: Perform SSM. If SSM positive and patient has been previously treated for TB, use Xpert in place of LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 3: Perform SSM only for patients not at DR-TB risk. Perform Xpert MTB/RIF for patient has been previously treated for TB.
Scenario 4: Perform Xpert MTB/RIF for all patients, regardless of DR-TB risk.
**The budget of the TB control program reported in the WHO 2014 report. (US$ 252 Million)
The mean diagnostic costs (for TB and rifampicin-resistant TB combined) per patient more than doubled for the Xpert-for-all scenario, from US$ 6.2 for SSM-only to US$ 16.4 (Table 6), representing a 102% increase in a mean diagnostic cost per true TB case initiated on treatment. The increase in mean total costs (including treatment) per true TB case initiated on treatment was about 11% from the baseline scenario to the Xpert-for-all scenario. Mean total costs per MDR case initiated on treatment were lowest in the Xpert-for-all scenario (US$ 11,099), and highest in scenario 2, with SSM as primary diagnostic tool and Xpert based DST, instead of LPA, for high risk TB cases (US$ 12,092).
Table 6. Mean costs per patient for 4 diagnostic strategies.
| Mean diagnostic costǂ | Mean treatment costǂ | Mean total costǂ | ||||||
|---|---|---|---|---|---|---|---|---|
| Diagnostic Strategy* | per patient tested | per TP TB case initiated on treatment** | per TP MDR case detected | per TP TB case detected | per TP MDR case detected | per patient tested | per TP TB case detected | per TP MDR case detected |
| 1. SSM Only | $6.2 | $60.8 | $999 | $643 | $10,579 | $71.7 | $704.1 | $11,578 |
| 2. Xpert MTB/RIF as a replacement for LPA testing | $5.8 | $56.5 | $968 | $649 | $11,124 | $71.9 | $705.6 | $12,092 |
| 3. Xpert MTB/RIF as a replacement for SSM for patients with previous TB history | $7.2 | $65.4 | $945 | $707 | $10,218 | $85.1 | $772.5 | $11,163 |
| 4. Xpert MTB/RIF for all patients | $16.4 | $122.5 | $1,734 | $662 | $9,364 | $104.9 | $784.2 | $11,099 |
TP = true positive; DR-TB = drug-resistant TB, i.e. rifampicin-resistant; FP = false positive; SSM = sputum smear microscopy
ǂAll costs in US$ 2013
*Scenario 1: Perform SSM. If SSM positive and patient has been previously treated for TB, use LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 2: Perform SSM. If SSM positive and patient has been previously treated for TB, use Xpert in place of LPA. If SSM negative and patient has been previously treated for TB, perform culture, LPA and/or DST.
Scenario 3: Perform SSM only for patients not at DR-TB risk. Perform Xpert MTB/RIF for patient has been previously treated for TB.
Scenario 4: Perform Xpert MTB/RIF for all patients, regardless of DR-TB risk.
**All diagnostic costs combined, for TB and DR-TB (16,492 true pulmonary TB cases among presumptive TB patients and 1,288 rifampicin resistant cases in the cohort).
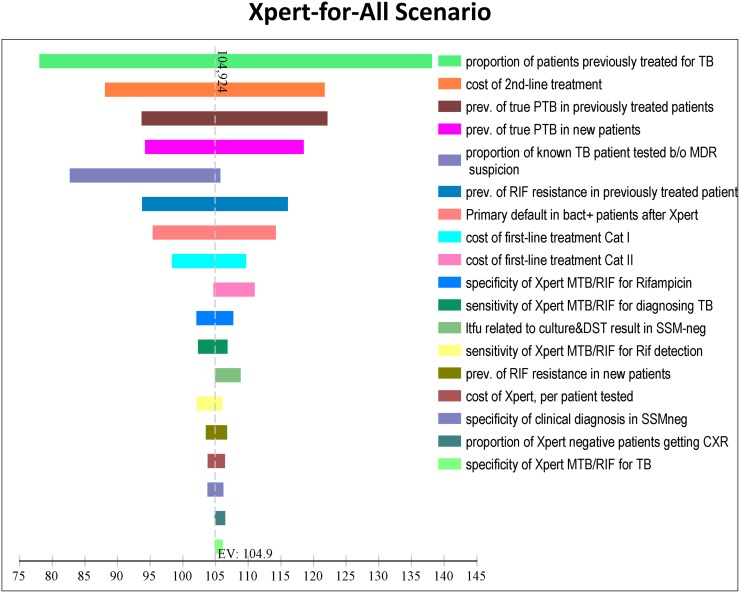
In Fig 1, the one-way effect of variation in model parameter values and assumptions on total cohort costs is shown for the top 18 variables (out of all included) in the Xpert-for all scenario. The largest variation in total costs was due to variation in parameters that increased or decreased the prevalence of TB in the cohort (in line with regional estimates of TB burden in India), and variation in parameters that affected second-line treatment cost.
Fig 1. Tornado diagram showing the effect of variation in each parameter value on total costs (US$ per patient tested) for the Xpert for all scenario.
Use and interpretation of chest x-rays (CXRs)
If all presumptive TB patients with negative bacteriological tests (SSM or Xpert) received CXR, the need for TB treatment, both for a true positive and false positive TB diagnosis, would increase in all scenarios (Table A of S1 File). Total cohort costs would increase by approximately half in all scenarios, largely due to increased cost for first-line treatment. If CXR would be applied after negative SSM, but not after a negative Xpert result, TB case detection of true positive TB cases would be approximately the same in all scenarios. Diagnostic cost would still be highest in the Xpert-for-all scenario, but total cohort costs would be lowest in this scenario, as false positive cases would not be initiated on treatment. DR-TB case detection and associated costs of second-line treatment remained unchanged.
Discussion
The WHO calls for the early diagnosis of TB, including universal DST and systematic screening of high-risk groups, as a critical component of the End TB Strategy. The RNTCP, seeking to control a growing TB epidemic while operating with a restricted budget, will need information regarding the associated costs and benefits to various diagnostic strategies in India to better inform Xpert scale-up and uptake and ultimately make progress towards the WHO End TB goals. This study found the upfront Xpert-for-all strategy to be associated with the greatest increase in TB and DR-TB case detection, and though it would have the highest associated total costs, the cost per true DR-TB case detected would be lower compared to the use of Xpert for DR-TB risk groups only.
The detection of true positive TB and DR-TB cases being highest for the upfront Xpert-for-all scenario is in line with previous findings [6, 7]. The Xpert for all strategy would increase the costs for diagnosis and treatment combined by approximately 46%, of which three quarters would be for increased treatment costs, especially for second-line treatment of additionally identified patients with DR-TB. Algorithms using Xpert only for patients at risk for MDR-TB would be more affordable, but less effective in increasing case detection. Also, the mean total cost per true DR-TB case detected and initiated on treatment would be lower with upfront Xpert-for-all compared to Xpert for DR-TB risk groups, only, primarily due to the Xpert-for-all identifying proportionally more DS-TB cases, which are cheaper to treat. The Xpert-for-all scenario was also the most robust to uncertainty in assumptions about the usage and performance of CXR in TB diagnosis. However, an expanded usage of Xpert across different strategies would require significant increased TB control budget to ensure that increased case detection is followed by appropriate care.
This study modeled the expected cost associated with roll-out of different Xpert scenarios to allow for the consideration of different diagnostic strategies for a set sample size given budget limitations. An earlier study demonstrated Xpert MTB/RIF to be a highly cost-effective as a replacement of SSM in India [4]. This was supported by the even lower average diagnostic costs per patient detected (and initiated on treatment) seen in this modeling study, which is largely explained by a lower per-patient test cost of the Xpert assay [15], and a higher prevalence of TB and drug-resistance TB in the current study under programmatic conditions. Our model predicted a 31% increase in detection of bacteriologically-confirmed pulmonary TB for the Xpert-for-all scenario, which was consistent with the Indian Xpert implementation study [7].
This study had a number of limitations. First, the analysis applied to patients in the public sector only. Diagnostics and treatment in the private sector were not included. Moreover, we assumed that patients made one TB diagnostic effort only, and so test-costs or cases detected at additional diagnostic visits were not considered [25]. Additionally, HIV-infected patients were not modeled as a separate group in this study. The HIV prevalence in India is low so the impact of this assumption on the overall result was expected to be small. Presumptive TB patients at increased risk of MDR were approximated by patients with a history of previous TB, comprising 17% of the cohort. Other patients at risk for DR-TB, such as MDR-contacts, were also not modeled as a separate group, as their number was expected to be small. Additionally, it should be noted that varying the assumptions about the prevalence of drug resistance in general showed a large effect on the expected total cohort costs, implying that the estimation of costs for certain regions may vary considerably along with regional variations in the distribution of drug resistance [6].
This study took the perspective of a TB service-provider. Therefore, costs encountered by the patients themselves, whether direct or indirect, were not considered in this analysis. Notably, patient pathways to TB diagnosis are complex and often include providers other than, or in addition to, those encountered in the public sector [25]. However, a diagnostic test such as Xpert, with higher sensitivity, would be expected to reduce the number of TB patient visits, especially given a reduction in the number of additional visits for CXR and/or repeat testing after negative test results were obtained. Practices related to clinical diagnosis and the use of CXR, as well as variation in SSM sensitivity (reflecting smear method and quality variations) may also have a substantial effect on costs, including treatment costs, even if the patients themselves paid the cost of CXR.
The uptake of rapid TB and DR-TB diagnostics such as Xpert MTB/RIF has become an RNTCP implementation priority as India works to control a growing TB epidemic. Economic modeling of the TB epidemic in India and different diagnostic strategies found the Xpert-for-all strategy to be the most costly, though it was the most effective in improving case detection and had the lowest mean total costs per DR-TB case initiated on treatment. Given current budget limitations, the RNTCP will have to consider these findings in the context of other TB control activities to determine the best approach to Xpert scale-up for TB and DR-TB control in India.
Supporting information
(DOCX)
Acknowledgments
We are very grateful to Sophia Georghiou, who helped to carefully revise this document in its final versions.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
This work was supported by the UK government through a Department for International Development (DFID) grant to FIND (grant number 204074-101). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Global Tuberculosis Report 2014. Geneva: World Health Organization (WHO/HTM/TB/2014.08); 2014.
- 2.Central TB Division DGoHSMoH&FW. Revised National Tuberculosis Control Programme: Guidelines on Programmatic Management of Drug Resistant TB (PMDT) in India. Central TB Division,Directorate General of Health Services,Ministry of Health & Family Welfare,Nirman Bhavan,New Delhi.110011; 2012 May.
- 3.World Health Organization. Policy Statement: Automated Real-time Nucleic Acid Amplification Technology for Rapid and Simultaneous Detection of Tuberculosis and Rifampicin Resistance: Xpert MTB/RIF System. Geneve, Switzerland: World Health Organization; 2011. [PubMed] [Google Scholar]
- 4.Steingart KR, Sohn H, Schiller I, Kloda LA, Boehme CC, Pai M, et al. Xpert(R) MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults (updated). Cochrane Database Syst Rev 2014;1:CD009593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vassall A, van Kampen S., Sohn H, Michael JS, John K, den Boon S., et al. Rapid diagnosis of tuberculosis with the Xpert MTB/RIF assay in high burden countries: a cost-effectiveness analysis. PLoS Med 2011. November;8(11):e1001120 doi: 10.1371/journal.pmed.1001120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raizada N, Sachdeva KS, Sreenivas A, Vadera B, Gupta RS, Parmar M, et al. Feasibility of Decentralised Deployment of Xpert MTB/RIF Test at Lower Level of Health System in India. PLoS One 2014;9(2):e89301 doi: 10.1371/journal.pone.0089301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sachdeva KS, Raizada N, Sreenivas A, van't Hoog AH, van den Hof S, Dewan PK, et al. Use of Xpert MTB/RIF in Decentralized Public Health Settings and Its Effect on Pulmonary TB and DR-TB Case Finding in India. PLoS One 2015. May;10(5):e0126065 doi: 10.1371/journal.pone.0126065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albert A, Nathavitharana RR, Isaacs C, Pai M, Denkinger CM, Boehme CC. Development, roll-out and impact of Xpert MTB/RIF for tuberculosis: what lessons have we learnt and how can we do better? Eur Respir J 2016; 48(2):516–25. doi: 10.1183/13993003.00543-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joint Monitoring Mission. 2015 Report on the Indian revised National TB Control Proframme from Joint Monitoring Mission. http://www.tbonline.info/media/uploads/documents/jmmdraft2015.pdf
- 10.Pantoja A, Fitzpatrick C, Vassall A, Weyer K, Floyd K. Xpert MTB/RIF for diagnosis of tuberculosis and drug-resistant tuberculosis: a cost and affordability analysis. Eur Respir J 2013. September;42(3):708–20. doi: 10.1183/09031936.00147912 [DOI] [PubMed] [Google Scholar]
- 11.Revill P, Walker S, Madan J, Ciaranello A, Mwase T, Gibb DM, et al. Using cost-effectiveness thresholds to determine value for money in low-and middle-income country healthc are systems: Are current international norms fit for purpose? CHE Research Paper 98. 2014. The University of York Centre for Helath Economics.
- 12.Steingart KR, Henry M, Ng V, Hopewell PC, Ramsay A, Cunningham J, et al. Fluorescence versus conventional sputum smear microscopy for tuberculosis: a systematic review. 2006;6(9):570–81. [DOI] [PubMed] [Google Scholar]
- 13.Boehme CC, Nicol MP, Nabeta P, Michael JS, Gotuzzo E, Tahirli R, et al. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. 2011;377(9776):1495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Revised National Tuberculosis Control Program (RNTCP). Training Module for Medical Practitioners. 2010. http://www.tbcindia.nic.in/showfile.php?lid=2908
- 15.Rupert S, Vassall A, Raizada N, Khaparde SD, Boehme C, Salhotra SS, et al. Bottom-up or top-down: unit cost estimation of TB diagnostic tests in India. Int J Tuberc Lung Dis 2017. [DOI] [PubMed] [Google Scholar]
- 16.Pantoja A, Lonnroth K, Lal SS, Chauhan LS, Uplekar M, Padma MR, et al. Economic evaluation of public-private mix for tuberculosis care and control, India. Part II. Cost and cost-effectiveness. Int J Tuberc Lung Dis 2009. June;13(6):705–12. [PubMed] [Google Scholar]
- 17.World Health Organization. CHOosing Interventions that are Cost Effective (WHO-CHOICE). http://www.who.int/choice/en/ [DOI] [PMC free article] [PubMed]
- 18.Floyd K, Arora VK, Murthy KJ, Lonnroth K, Singla N, Akbar Y, et al. Cost and cost-effectiveness of PPM-DOTS for tuberculosis control: evidence from India. Bull World Health Organ 2006. June;84(6):437–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodchild M, Sahu S, Wares F, Dewan P, Shukla RS, Chauhan LS, et al. A cost-benefit analysis of scaling up tuberculosis control in India. Int J Tuberc Lung Dis 2011. March;15(3):358–62. [PubMed] [Google Scholar]
- 20.Tupasi TE, Gupta R, Quelapio MI, Orillaza RB, Mira NR, Mangubat NV, et al. Feasibility and cost-effectiveness of treating multidrug-resistant tuberculosis: a cohort study in the Philippines. PLoS Med 2006. September;3(9):e352 doi: 10.1371/journal.pmed.0030352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fitzpatrick C, Floyd K. A systematic review of the cost and cost effectiveness of treatment for multidrug-resistant tuberculosis. Pharmacoeconomics 2012. January;30(1):63–80. doi: 10.2165/11595340-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 22.GDF Procurement. MDR TB Drugs for the year 2012–13. http://www.stoptb.org/gdf/drugsupply/drugs_available.asp. 2013.
- 23.Ramachandran R, Nalini S, Chandrasekar V, Dave PV, Sanghvi AS, Wares F, et al. Surveillance of drug-resistant tuberculosis in the state of Gujarat, India. Int J Tuberc Lung Dis 2009. September;13(9):1154–60. [PubMed] [Google Scholar]
- 24.Walusimbi S, Bwanga F, De CA, Haile M, Joloba M, Hoffner S. Meta-analysis to compare the accuracy of GeneXpert, MODS and the WHO 2007 algorithm for diagnosis of smear-negative pulmonary tuberculosis. BMC Infect Dis 2013;13:507 doi: 10.1186/1471-2334-13-507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charles N, Thomas B, Watson B, Raja SM, Chandrasekeran V, Wares F. Care seeking behavior of chest symptomatics: a community based study done in South India after the implementation of the RNTCP. PLoS One 2010;5(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bwanga F, Hoffner S, Haile M, Joloba M. Direct susceptibility testing for multi drug resistant tuberculosis: a meta-analysis. BMC Infect Dis. 2009. May 20; 9:67 doi: 10.1186/1471-2334-9-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.