Abstract
Child abuse includes all forms of physical and emotional ill treatment, sexual abuse, neglect, and exploitation that results in actual or potential harm to the child's health, development, or dignity. In Taiwan, the Child Protection Medical Service Demonstration Center (CPMSDC) was established to protect children from abuse and neglect. We further analyzed and compared the trends and clinical characteristics of cases reported by CPMSDC to evaluate the function of CPMSDC in approaching child abuse and neglect in Taiwan. We prospectively recorded children with reported child abuse and neglect in a CPMSDC in a tertiary medical center from 2014 to 2015. Furthermore, we analyzed and compared age, gender, scene, identifying settings, time of visits, injury type, injury severity, hospital admission, hospitalization duration, and outcomes based on the different types of abuse and the different settings in which the abuse or neglect were identified. Of 361 child abuse cases (mean age 4.8 ± 5.36 years), the incidence was highest in 1- to 6-year-old children (n = 198, 54.85%). Physical abuse and neglect were predominant in males, while sexual abuse was predominant in females (P < 0.001). Neglect was most common (n = 279, 75.85%), followed by physical (n = 56, 15.51%) and sexual abuse (n = 26, 7.2%). The most common identifying setting was the emergency department (n = 320, 88.64%), with neglect being most commonly reported. Head, neck, and facial injuries were more common in physically abused children than in neglected and sexual abused children (P < 0.005), leading to longer hospitalization (P = 0.042) and a higher Injury Severity Score (P = 0.043). There were more skin injuries in neglect (P < 0.001). The mortality rate was 2.49% (n = 9). The CPMSDC could enhance the ability, alertness, and inclination of professionals to identify suspected cases of child abuse, and to increase the rate of registry. Cases of physical abuse had a higher Injury Severity Score, longer duration of hospitalization, and more injuries of head, face, and neck compared with other types of abuse. The reported rate of neglect was highly elevated after the CPMSDC established during the study period. Recognition of neglect is not easy, but the consequent injury, especially asphyxia, may lead to mortality.
Keywords: child abuse, high-risk families, neglect, physical abuse, sexual abuse
1. Introduction
Caring for a child can be stressful and it is not always easy. A child may be harmed by any family member, caregiver, or neighbor. Child abuse and neglect affects more and more children in the world, and it remains a serious and important issue. According to the World Health Organization (WHO), child abuse includes all forms of physical and emotional ill treatment, sexual abuse, neglect, and exploitation that results in actual or potential harm to the child's health, development or dignity.[1] The 4 major types of child abuse are physical abuse, sexual abuse, emotional abuse, and neglect. Physical abuse is defined as those acts of commission by a caregiver that cause actual physical harm or have the potential for harm. Sexual abuse is defined as those acts in which a caregiver or adult in a power and trust position uses a child for sexual gratification. Emotional abuse includes the failure of a caregiver to provide an appropriate and supportive environment, and includes acts that have an adverse effect on the emotional health and development of a child. Neglect refers to the failure of a parent to provide for the development of the child in 1 or more of the following areas: health, education, emotional development, nutrition, shelter, and safe living conditions.[1]
In 2014, the incidence of child abuse was 17.24 per 1000 child population in the United States,[2] while it was 3.02 per 1000 child population in Taiwan according to Ministry of Health and Welfare. The incidence of child abuse in Taiwan is much lower than in the United States. The lack of education about the recognition and management of child abuse for workers, including medical professionals, may be the main reason. All clinical workers have a responsibility to protect children from harm. In addition, other reasons may be associated with the low reported rate in Taiwan such as some other cultural factors, including the severity of punishments, effectiveness of the legal system, level of parental education, and socioeconomic factors. In order to enhance medical professionals’ abilities to recognize and manage child abuse and neglect, The Child Protection Medical Service Demonstration Center (CPMSDC) was established in Taiwan from August 2014. The CPMSDC is a referral center receiving cases transferred from local clinics, regional hospitals, social and politic institutions, and composed of social workers, case managers, psychologists, and medical doctors of pediatrics, ophthalmology, obstetrics and gynecology, neurosurgery, radiology, orthopedics, and psychiatry. The center is dedicated to identify and protect children who have been harmed or are at risk of harm, and whose parents are unable to provide adequate care or protection. In this study, we analyzed the trends and compared the clinical characteristics of reported cases in a CPMSDC in a tertiary medical center based on different types of abuse, age, gender, and settings in which the abuses and neglect were identified.
2. Methods
2.1. Patient population
From August 2014 to July 2015, the CPMSDC prospectively recorded all cases with reported child abuse and neglect in our tertiary medical center in Taiwan. All suspected cases suffering from child abuse and neglect reported to the CPMSDC via the emergency department (ED), outpatient department (OPD), and ward were included in our survey. The study was approved by the Institutional Review Board of the Chang Gung Memorial Hospital.
2.2. Methods
We identified patients with child abuse and neglect by searching the records database of the CPMSDC during the study period. The types of child abuse categorized in mutually exclusive categories in the setting included physical abuse a, sexual abuse, emotional abuse, and neglect. In addition, children in high-risk families were also recorded. The high-risk families were defined as families with poor socioeconomic backgrounds, domestic violence histories, parental drug addiction, alcoholism, or psychological disorders, and poor supports from other famines, etc. The following information was obtained from each patient's records: age, gender, scene of the events, identifying settings (ED, OPD, and wards), time of visits (8 am to 5 pm, 5 pm to 0 am, and 0 am to 8 am), abuse types, admission units (wards or intensive care units [ICU]), injury types, injury severity, duration of hospitalization, and clinical outcomes. All cases were categorized into 5 different age groups: less than 3 months, 3 months to less than 12 months, 1 to less than 6 years, 6 to less than 12 years, and 12 to 18 years. Injury severity was evaluated by using the Injury Severity Score (ISS).[3] Six body regions are used to calculate the ISS including head and neck, face, thorax, abdomen, extremities, and external. These regions are not mutually exclusive. The ISS of cases who did not have obviously traumatic injuries were classified as “not available.” Children with sustained head injury were classified into 3 mutually exclusive subsets: skull fracture—those with single or multiple skull fractures but no intracranial injury; intracranial injury—those with intracranial injury with or without skull fractures; and other—those with concussion or not otherwise specified closed head injury.[4] We further analyzed the trends of reported months, age, and identifying settings in cases of abuse and neglect. In addition, related clinical variables of the reported cases were analyzed and compared based on gender, abuse types, and identifying settings.
2.3. Statistical analysis
The data of categorical variables were analyzed by using the chi-square test or Fisher exact test. Continuous variables were analyzed by using the t test and the Kruskal–Wallis test. A P value less than 0.05 was considered to be statistically significant. Distributions of variables were reported as percentages and means ± standard deviation. Statistical analyses were performed with SPSS software (version 19.0, SPSS Inc., Chicago, IL).
3. Results
3.1. Demographics and gender of child abuse
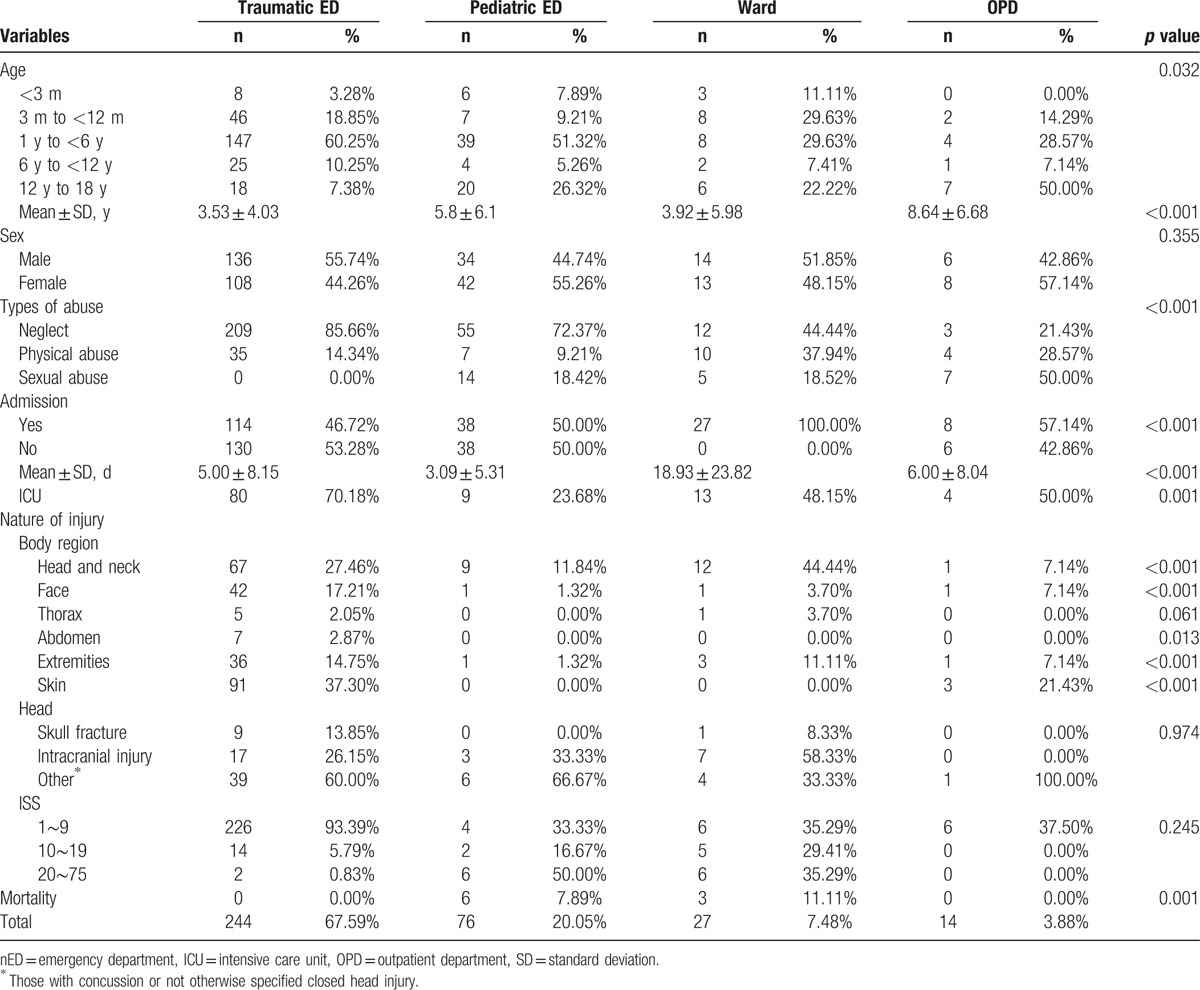
During the study period, 361 cases of child abuses were reported via the CPMSDC in our medical center, and 20 cases were reported as high-risk families. The number of cases increased monthly in 2014, and remained steady in 2015 (Fig. 1A). Most cases were reported from the ED (88.64%), followed by the wards (7.48%). There were 190 boys (52.63%) and 171 girls (47.37%) with the mean age of 4.8 ± 5.36 years (Table 1). The mean age was higher in girls than that in boys (3.64 vs 4.94 years, P = 0.012; Table 2). The highest incidence of reported cases with abuse occurred in the age group of 1 to less than 6 years (n = 198, 54.86%), followed by 3 months to less than 12 months (n = 63, 17.45%). Children under 2 years accounted for about half of reported cases (45.71%; Fig. 1B). For children aged 3 to less than 12 months and 6 to less than 12 years, boys were in the majority, but girls were predominant in the age group of 12 to 18 years (P = 0.002; Table 2). Most events occurred at home (n = 301, 83.38%). The most common reported abuse type was neglect (n = 279, 77.29%), followed by physical abuse (n = 56, 15.51%), and sexual abuse (n = 26, 7.2%). Both physical abuse and neglect were male predominant, but sexual abuse was female predominant (P < 0.001). In most abused cases, the perpetrators were unknown. In identified perpetrators, father (50%) and mother (7%) were the most common. Other perpetrators included a parent's domestic partner, babysitter, and other relatives. Most cases were reported during the day (8 am to 5 pm; n = 166, 45.98%), and least were reported after midnight (0 am to 8 am; n = 46, 12.74%) (Fig. 2 A). The rate of admission in child abuse was 51.8% and ICU admission was 29.4% (Fig. 3). The mean duration of hospitalization was 5.68 ± 10.43 days. The mortality rate was 2.49% (n = 9). Of the 9 mortality cases, 2 were reported as physical abuse which were identified as abused head injury (shaken infant syndrome), and 7 were reported as neglect, including 3 cases of drowning and 4 cases of asphyxia.
Figure 1.
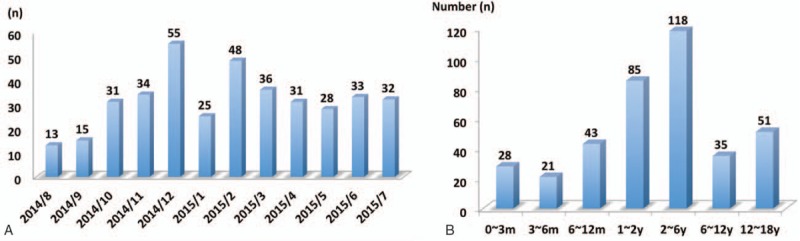
Case numbers of reported child abuse in different months (A) and different age groups (B).
Table 1.
Demographic data of abused and neglected children.
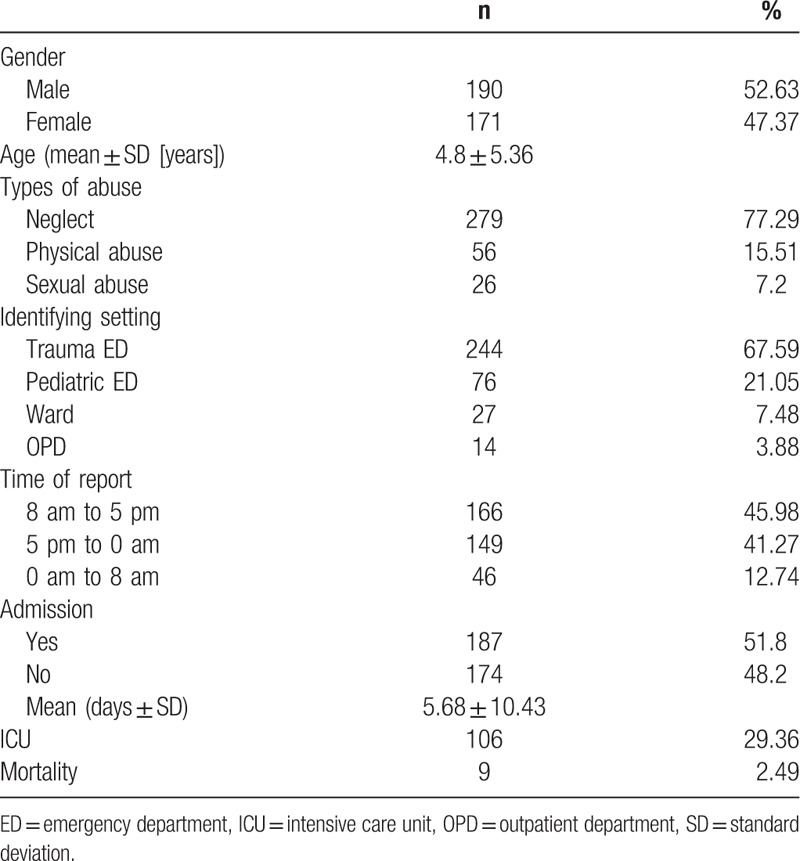
Table 2.
Comparison of related clinical factors in children with abuse and neglect based on gender.
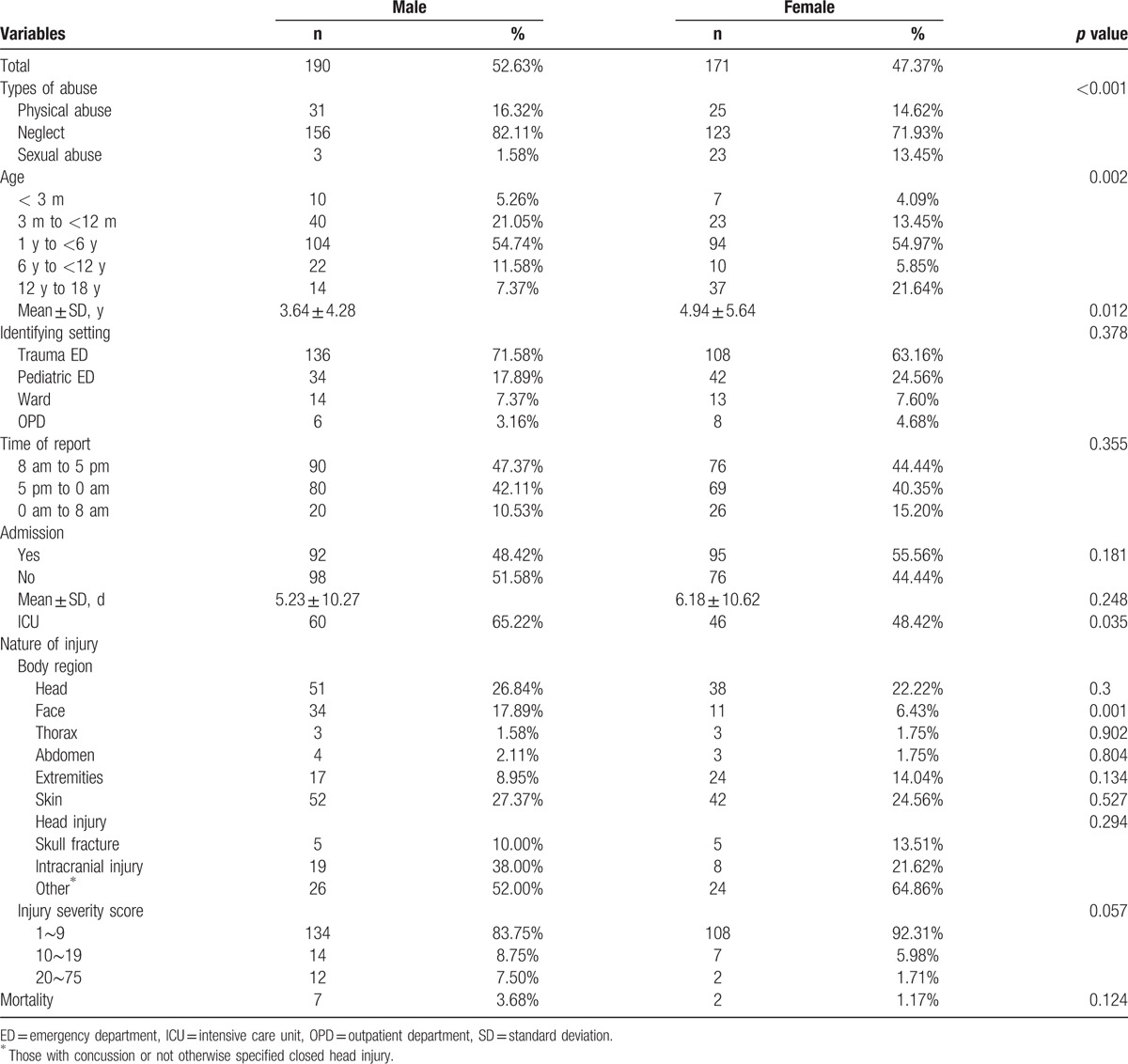
Figure 2.
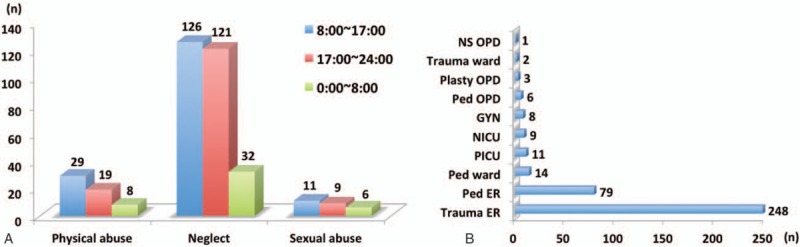
Time of report of different abuse types: 8 am to 5 pm (8:00–17:00), 5 pm to 0 am (17:00–24:00), and 0 am to 8 am (0:00–8:00) (A) and details of the identifying settings of child abuse (B).
Figure 3.
Disposition of reported cases of child abuse (discharge, admission to ward, and intensive care unit) based on different months.
3.2. Analysis based on abuse type and identifying settings
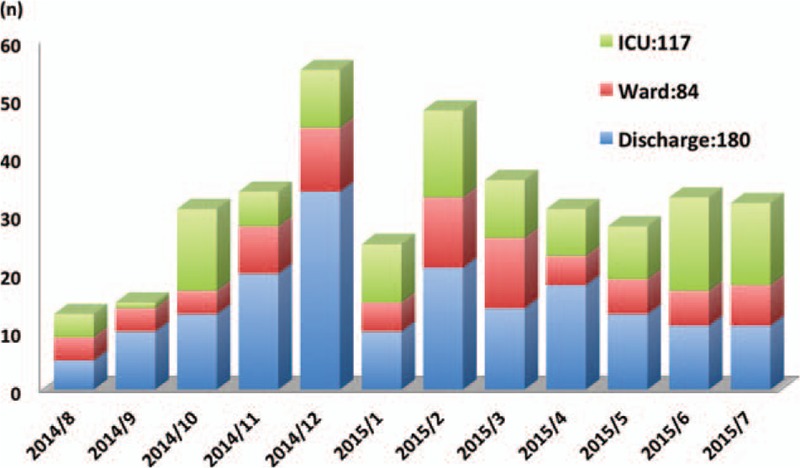
The sexually abused children had the highest mean age (13.73 ± 4.56 years), while the neglected children had the youngest age (3.10 ± 3.56 years; P < 0.001) (Table 3). The most common identifying setting was the traumatic ED (n = 244, 67.59%), followed by the pediatric ED (n = 76, 20.05%) and the wards (n = 27, 7.48%). Details of the identifying settings are shown in Fig. 2B. Most cases with neglect and physical abuse were reported by the traumatic ED, and most sexually abused cases were reported by the pediatric ED (P < 0.001; Table 4). In the OPD, sexual abuse was most commonly reported abuse type (43%). There was no significant difference of reported time among the abuse types and identifying settings. Physically abused children had a longer duration of hospitalization (P = 0.042). Boys admitted to the ICU were more than girls (P = 0.03), and the abused cases admitted to the ICU transferred from the ED were more than those from other units (P = 0.001).
Table 3.
Comparison of related clinical factors based on different types of abuse.
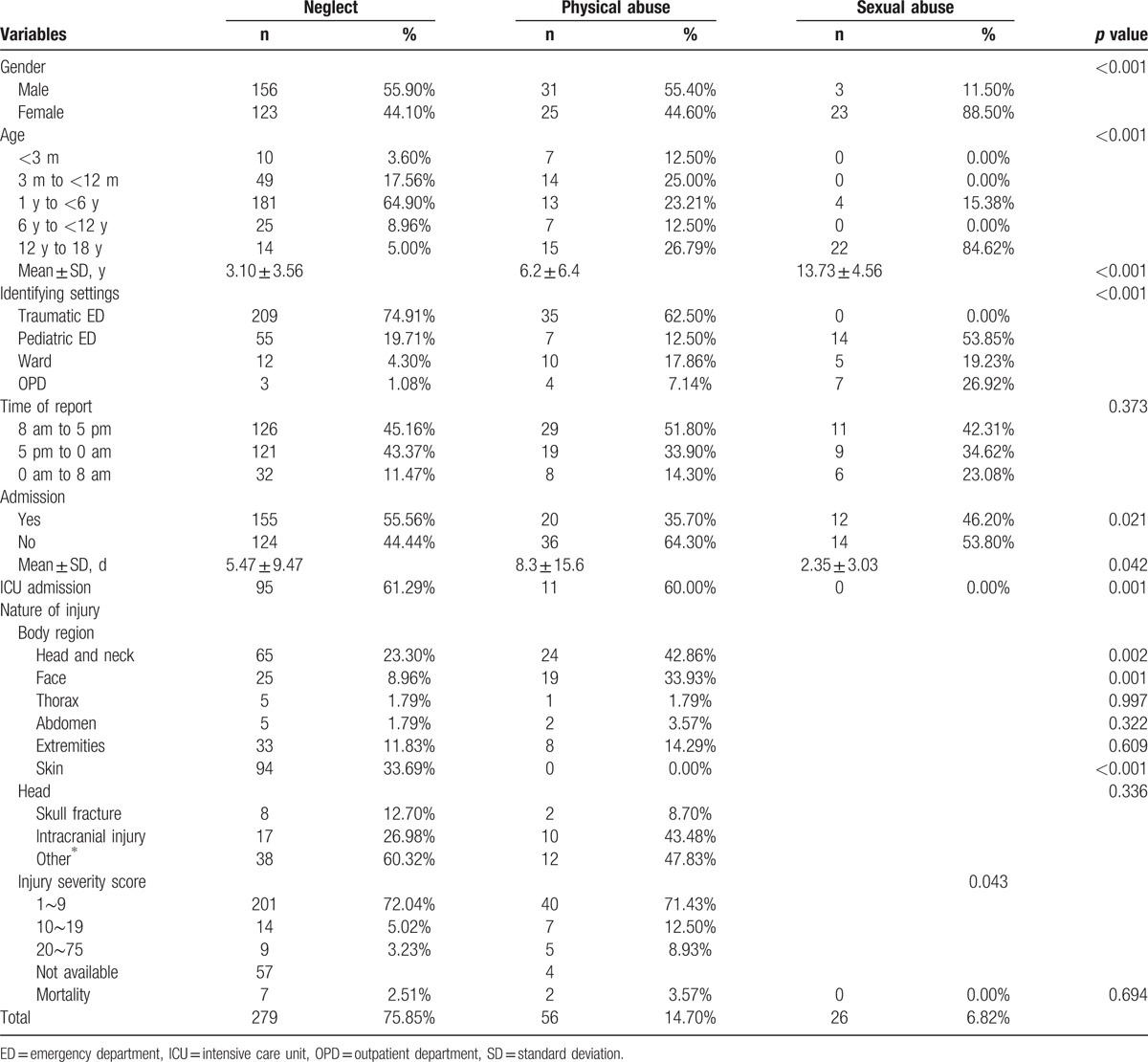
Table 4.
Comparison of related clinical factors in children with abuse and neglect based on the different identifying settings.
Head, neck and face injuries were more common in physically abused children than those in neglected and sexually abused children (P = 0.002; P < 0.001, respectively). More boys had facial injuries than girls (P = 0.001). However, there were no significant differences between types of head injuries and abuse types. Otherwise, skin injuries were more common in neglected children than those in other abuse types (P < 0.001). Children reported from the traumatic ED tended to have head, face, extremity, and skin injuries (P < 0.001). Physically abused children had a higher ISS than those with other abuse types (P = 0.043). However, there was no significant difference in ISS among cases reported from the different identifying settings. Boys and girls had no significantly different ISS and mortality rates. In addition, there was no significant difference in mortality rate among the abuse types.
4. Discussion
Annually, the incidence of child abuse and neglect is approximately 700,000 to 1.25 million children in the United States,[5] 107,200 to 160,000 children in the Netherlands,[6] and 12,500 to 20,300 children in Taiwan. Worldwide, about 155,000 deaths occur annually in children as a result of abuse or neglect,[7] and when combined with child homicide, it is the second leading cause of death of children in the United States.[8] Child maltreatment, therefore, remains a serious and important public health problem associated with a broad range of negative outcomes that can extend into adulthood.
Some previous studies have reported that physical abuse affects 1 in 11 children in the United Kingdom each year and it is estimated that about 1% of all injured children visiting the ED do so due to physical abuse.[9] In our study, of the 361 children reported to the CPMSDC as child abuse, the reported rate was 0.71%, which accounted for 5.2% of all injured children in the ED. The rate was higher than the national rate in Taiwan. However, according to the Child Maltreatment Report in the United States in 2010, neglect was the most common form of child abuse (neglect 78.3%, physical abuse 17.6%, sexual abuse 9.2%, and emotional maltreatment 8.1%).[5] In our study, the results also showed that neglect was the most common form (77.29%), but no emotional maltreatment was identified. According to the national data in Taiwan in 2014, physical abuse was the most common form (31.52%), followed by sexual abuse (15.69%), emotional abuse (10.78%), and neglect (9.98%). Some previous studies also showed that physical abuse was the most common type of child abuse detected in the ED.[10] Neglect is sometimes difficult to identify because the injuries may be subtle, and staffs may not report even suspected cases due to the lack of sufficient evidences. However, we think that early recognition and identification of neglect could be helpful to educate the family or caregivers to enhance their ability to care for their children, and to prevent children from further abuse. Moreover, we noticed that most cases of neglect and physical abuse were under the age of 6 years, and the mean age of neglect was even younger than that of physical abuse. Children under 6 years old are vigorous and curious, and injuries easily happen under insufficient surveillance, especially for boys. In other studies, injuries were found in only 2% of cases of supervisory neglect and half of these injuries were not severe enough to require medical treatments.[11] Thus, the reported cases of neglect from the hospital may still be an underestimation. The reported rate of neglect in our study was higher than that in other studies.[11] Based on the findings, we consider this may be attributed to the increased training of professionals regarding the recognition of abused injuries by an educational series from the CPMSDC, and elevated willingness to report suspicions of abuse and to recognize variations in what is considered to be abuse by a well-organized teamwork. Therefore, we think the role of the CPMSDC could enhance the ability, alertness, and inclination of professionals to identify suspected cases of child abuse, and to increase the rate of registry.
In most neglected and abused cases, events happened unexpectedly. Children were commonly sent to the ED with various degrees of injury. Thus, the ED staffs were often the first professionals to contact with these victims. It is necessary and essential for them to be alert to children with suspected abuse in clinical practice. In our study, the ED was also the most common identifying setting for child abuse and neglect while the wards were the most common identifying setting for high-risk families. As the staffs in the wards have more time to get along with hospitalized children and their caregivers, they may have more opportunities to identify potential high-risk families in the wards. In contrast, sexual abuse was the most common type reported from the OPD. The reason might be that cases with sexual abuse may feel ashamed and be afraid to inform others about what happened. So they would like to choose the obstetrician-gynecologists to approach their related sexual problems instead of the ED doctors.
In our study, cases with physical abuse commonly suffered from head, neck, and facial injuries (76.8%), and had higher ISS, and longer duration of hospitalization. Although it has been reported that bruising may show a high sensitivity and specificity in predicting child abuse,[12] only 9 cases of physical abuse had bruises over their bodies in our study. This low reported rate of bruises in our study might be due to incomplete chart records or incomplete physical examination of the medical staffs and social workers. This may reflect the importance and persistence of the CPMSDC in promoting the ability, alertness, and inclination of professionals to identify child abuse. For any children with unexplained injuries, even without obvious bruising, physical abuse should be considered along with a serious course of action. Especially for cases injured by suspected abuse, early recognition of head, neck, and facial injuries, and immediate managements could be helpful for their survival and functional outcome. Abdominal injuries were found in 7 cases of physical abuse and neglect (2.1%), and 4 (1.2%) were admitted. All 7 cases had no bruising, echoing previous studies that abdominal bruising was absent in up to 80% of cases.[13] Clinicians should always keep in mind that the absence of bruising may not preclude intraabdominal abused injuries.
In our study, 2 of the 9 mortality cases presented with out-of-hospital cardiac arrest caused by abused head injury (shaken infant syndrome). Both were younger than 6 months old. Head injury is the leading cause of death in abused children under 2 years of age.[14] Younger children, especially those who have regularly visited the EDs or clinics for accidental injuries, may be more likely to sustain an abusive fatal injury.[15] In the ED, if children under 2 years of age initially present with severe injuries, brain imaging examinations should be considered to rule out brain insults caused by abuse. The other 7 mortality cases were caused by drowning and asphyxia due to the caregiver's neglect. Asphyxia usually results in irreversible morbidity and mortality if it cannot be detected and rescued in time. Therefore, it is necessary and important to educate caregivers in performing immediate basic life support for asphyxiated children. As caring for a child can be stressful and difficult, the prevention of child abuse and protection for children remain an important issue now and in the future.
Child abuse is an issue of public health. Different countries in United States, Europe, Africa, and Asia could have different outcomes and causes of child abuse and neglect. Moreover, some further problems for child abuse are also important and necessary to be discussed and focused on such as the structure of health care systems, the settings, environments, cardiovascular diseases, social environment,[16–20] and social inequalities, especially in children.[21,22] Health is a very complicated issue including multidimensional compositions such as social inequalities and economy, setting (environment, healthy cities), empowerment (education and literacy), sense of coherence (salutogenesis and mental well-being), behavior (physical activity, nutrition, and demographic change), medical care, and scientific approach1.[16] The structure of health care systems and the setting are different all around the world, and our world is full of inequalities that cause different health performance. Social inequalities are one of the most important factors associated with health.[17] Various socioeconomic statuses are associated with inequalities in health. One of the largest problems is access to medical care and support for patients with low socioeconomic status.[18] Income is related to health because it is a determinant of material living standards exerting a major direct influence on health. Greater income equality tends to improve social cohesion and reduce the social divisions, associated with better health. Meanwhile, psychosocial pathways provide a new route through which they affect health. For instance, the very well-established relation between violence and inequality, the causal chain must run all the way from the material facts of inequality to the psychosocial effects which lead to violence. Psychosocial effects of social position account for the larger part of health inequalities.[16,18] Inequalities in access to good-quality health care have a role in generating inequalities in mortality. These inequalities might be reduced by improving educational opportunities, income distribution, or access to health care.[19]
Previous study showed that access to health care and the quality of health care are suboptimal for uninsured and underinsured children.[22] Those lacking insurance are more likely to have needed care that is delayed of forgone; less access to preventive, specialist, or long-term care; lower utilization rates; and poor health outcomes.[22] Children who are ignored are at risk of being abuse and are hardly being identified. Low socioeconomic status and income also make people feel disrespected and have bad psychosocial effects which lead to violence.[18] Consequently, low socioeconomic status may be a common risk factor for physical abuse and neglect. On the other hand, higher socioeconomic status could be associated with better health because it may enhance social cohesion and reduce social division.[20] In some studies, they also illustrated that bigger income differences may lead to poor health.[16,18]
Some important differences in the development of health among different countries include different industrial developments, and different social developments. For example with some developing areas in Asia and Africa which are lack of salutogenetic promotion ideas may lead to increasing cardiovascular diseases and diabetes.[16,23,24] However, in the developed areas in some European countries or United States, the development of health is better than those in developing countries due to well organized salutogenetic promotion ideas, for instance, improved educational opportunities and income distribution.[19]
Health promotion in a country is the key way to reduce child maltreatments. According to the recommendations of WHO, firstly the government should build healthy public policy including legislation, fiscal measures, taxation to reduce poverty and income differences. Secondarily, creating supportive environments is very important because safe, inspiring, satisfying working and living circumstance can promote health efficiently. Thirdly, the government should enhance personal skills such as providing knowledge, education for health, and strengthening life skills. Finally the government should reorient the health services to support the needs of personals and communities, and make good connection between the health part and the social, political, and economical environmental compositions.[25,26] Every country should take above actions to improve individual healthy condition, and then the family could supply a sound environment for their children to prevent child maltreatments. According to Ottawa Charter, health is a resource of everyday life, not the objective of living. Health promotion action aims at reducing differences in current health status and ensuring equal opportunities and resources to enable all people to achieve their fullest health potential.[27] Everyone, including children, has the right to maintain their health. CPMSDC aimed to protect children from being deprived of their health, create a supportive environment for them, and strengthen community action. As the concept of the WHO Healthy cities project, health is the business of all sectors, and the government should promote systemic policy for health and ameliorate inequalities of health.
Nevertheless, there were some limitations in this study. First, given geographical and country differences in clinical practice, the different distribution of abuse types may exist. Second, child abuse includes 4 types as physical abuse, sexual abuse, neglect, and emotional abuse. However, for emotional abuse, it was difficult in identification due to the ambiguous manifestation and seldom to be reported in this study. For child neglect, the difference of recognition standard may exist due to the potentially different clinical judgments by primary clinicians, and some cases of neglect might be missed in this survey. Third, the establishment of the CPMSDC in Taiwan was in August, 2014 and the study period was only 1 year. During the 1-year study period, the definite effect of the CPMSDC may not be identified well and entirely, and we think this study may appear as a pilot study for the CPMSDC to prevent child abuse in Taiwan. However, in our ongoing study, we will analyze all issues in detail and show the outcome of measures taken by CPMSDC.
5. Conclusions
The CPMSDC can enhance the ability, alertness, and inclination of professionals to identify suspected cases of child abuse, and to increase the rate of registry. Children with physical abuse and neglect were under the age of 6 years commonly. Cases of physical abuse had a higher ISS, longer duration of hospitalization, and more injuries of head, face, and neck compared with other types of abuse, and therefore, early recognition of head, neck, and facial injuries, and immediate managements could be helpful for survival and functional outcomes. The reported rate of neglect was highly elevated after the CPMSDC established during the study period. Recognition of neglect is not easy, but the consequent injury, especially asphyxia, may lead to mortality. Clinically it is important for primacy clinicians to pay more attention to cases with neglect.
Acknowledgments
We thank for the contributions of all members of Child Protection Medical Service Demonstration Center in Chang-Gung Memorial hospital to identify and protect child abuse cases. We thank for the statistician in Chang-Gung Memorial hospital to complete the statistical analysis.
Footnotes
Abbreviations: CPMSDC = Child Protection Medical Service Demonstration Center, ED = emergency department, ICU = intensive care unit, ISS = injury severity score, OPD = outpatient department.
C-YC and J-LH contributed equally to this work.
CYC reviewed the medical records, analyzed and interpreted the data, and drafted the manuscript; SHH, FSO, and KLL interpreted the data. IJC, YCH, and EPL reviewed the medical records and interpreted the data. CHC and JLH interpreted the data and oversaw the study, and CTW analyzed the data. HPW designed and oversaw the study, interpreted the data, and revised the manuscript. All authors have read and approved the final manuscript for publication.
The authors have no conflicts of interest to declare.
References
- 1.Child abuse and neglect by parents and other caregivers, in World report on violence and health, L.L.D. Krug EG, Mercy JA, Zwi AB er al. Editor. 2002. p. 59–60. [Google Scholar]
- 2.Sedlak AJ, MJ, Basena M, et al. Fourth National Incidence Study of Child Abuse and Neglect (NIS–4): Report to Congress. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families. 2010. [Google Scholar]
- 3.Salehi O, Tabibzadeh Dezfuli SA, et al. A New Injury Severity Score for Predicting the Length of Hospital Stay in Multiple Trauma Patients., Namazi SS, Dehghan Khalili M, Saeedi M. Trauma Mon. 2016; 21:e20349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DiScala C, Sege R, Li G, et al. Child abuse and unintentional injuries: a 10-year retrospective. Arch Pediatr Adolesc Med 2000; 154:16–22. [PubMed] [Google Scholar]
- 5.Child Maltreatment 2010: Summary of Key Findings, in Children's Bureau, Child Welfare Information Gateway, Protecting Children Strengthening Families. Retrieved May 2012. [Google Scholar]
- 6.Euser EM, van Ijzendoorn MH, Prinzie P, et al. Prevalence of child maltreatment in The Netherlands. Child Maltreat 2010; 15:5–17. [DOI] [PubMed] [Google Scholar]
- 7.Gilbert R, Widom CS, Browne K, et al. Burden and consequences of child maltreatment in high-income countries. Lancet 2009; 373:68–81. [DOI] [PubMed] [Google Scholar]
- 8.Johnson CF. Child maltreatment 2002: recognition, reporting and risk. Pediatr Int 2002; 44:554–560. [DOI] [PubMed] [Google Scholar]
- 9.Woodman J, Pitt M, Wentz R, et al. Performance of screening tests for child physical abuse in accident and emergency departments. Health Technol Assess 2008; 12.iii, xi–xiii 1–95. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert R, Kemp A, Thoburn J, et al. Recognising and responding to child maltreatment. Lancet 2009; 373:167–180. [DOI] [PubMed] [Google Scholar]
- 11.Ruiz-Casares M, Trocmé N, Fallon B. Supervisory neglect and risk of harm. Evidence from the Canadian Child Welfare System. Child Abuse Negl 2012; 36:471–480. [DOI] [PubMed] [Google Scholar]
- 12.Pierce MC, Kaczor K, Aldridge S, et al. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 2010; 125:67–74. [DOI] [PubMed] [Google Scholar]
- 13.Gaines BA, Shultz BS, Morrison K, et al. Duodenal injuries in children: beware of child abuse. J Pediatr Surg 2004; 39:600–602. [DOI] [PubMed] [Google Scholar]
- 14.Roaten JB, Partrick DA, Nydam TL, et al. Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. J Pediatr Surg 2006; 41:2013–2015. [DOI] [PubMed] [Google Scholar]
- 15.Ortega HW, Vander Velden H, Kreykey NS, et al. Childhood death attributable to trauma: is there a difference between accidental and abusive fatal injuries? J Emerg Med 2013; 45:332–337. [DOI] [PubMed] [Google Scholar]
- 16.Leischik R, Dworrak B, Strauss M, et al. Plasticity of health. Ger J Med 2016; 1:1–17. [Google Scholar]
- 17.Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ 1997; 314:591–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 2006; 62:1768–1784. [DOI] [PubMed] [Google Scholar]
- 19.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008; 358:2468–2481. [DOI] [PubMed] [Google Scholar]
- 20.Sallis JF, Cervero RB, Ascher W, et al. An ecological approach to creating active living communities. Annu Rev Public Health 2006; 27:297–322. [DOI] [PubMed] [Google Scholar]
- 21.Inchley J, Currie D, T. Y, Samdal O, et al. Growing up unequal: gender and socioeconomic differences in young people's health and well-being. Health Behaviour in School-aged Children (HBSC) study: international report from the 2013/2014 survey. Health Policy for Children and Adolescents No. 7. WHO Regional Office for Europe, Copenhagen, Denmark. 2016. [Google Scholar]
- 22.Kogan MD, Newacheck PW, Blumberg SJ, et al. Underinsurance among children in the United States. N Engl J Med 2010; 363:841–851. [DOI] [PubMed] [Google Scholar]
- 23.Laatikainen T, Critchley J, Vartiainen E, et al. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol 2005; 162:764–773. [DOI] [PubMed] [Google Scholar]
- 24.Viswanathan V, Sathyamurthy S. Global increase in the prevalence of diabetes with special reference to the Middle East and Asia. Diabetes Technol Ther 2015; 17:676–678. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organisation. The Ottawa Charter for Health Promotion. Health Promotion. 1986. [Google Scholar]
- 26.World Health Organisation. Healthy Cities 2016. [Google Scholar]
- 27.World Health Organization. Ottawa charter for health promotion. Can J Public Health 1986; 77:425–430. [PubMed] [Google Scholar]


