ABSTRACT
Aim:
The implementation of evidence-based practice (EBP) is extremely important and plays a vital role in healthcare practice. There have been few studies concerning the level of healthcare provided to patients in Saudi Arabia, using EBP as an indicator. This study is aimed at investigating physiotherapists’ behaviour, attitudes, awareness and knowledge about EBP, along with barriers that curb the implementation of EBP.
Methods:
A sample of convenience was used and an online survey consisting of 14 closed-ended questions was given to both clinical and academic physiotherapists in Saudi Arabia from May to October 2016. Data regarding demographics, behaviour, attitudes, awareness, knowledge, previous formal training and barriers to implementation of EBP were recorded. The data were analysed using IBM SPSS version 19.
Results:
A total of 604 physiotherapists participated in the survey, out of which 385 respondents provided complete data. Nine participants were undergraduate physiotherapy students or not physiotherapists and their responses were excluded. The final number of participants included in data analysis was 376. The majority of the participants were men (60.4%) and most of them had completed their bachelor degree (66.2%). Although most physiotherapists reported a positive attitude towards the use of research in practice, there were many who were unfamiliar with the terms and implementation of EBP. The majority of physiotherapists had no formal EBP training (70.2%) in universities or any authorized training centres. According to the responses collected, the most important barrier to the implementation of EBP was insufficient teaching in previous education (43.1%), followed by lack of research knowledge and skills (36.4%). The study revealed that there was a significant association between physiotherapists’ attitude and their education level, while no significant associations were identified based on other demographic data. In addition, there were significant associations between physiotherapists’ awareness and knowledge and demographics such as education level, work setting, job title and previous training in EBP.
Conclusion:
There is a prominent gap in terms of understanding and applying the concept of EBP among physiotherapists in Saudi Arabia. Given that the majority of practicing physiotherapists reported no formal training in EBP, there is a need to integrate concepts related to EBP into the undergraduate and graduate curriculum. In addition, strategies must be developed and implemented to encourage practicing physiotherapists for gaining knowledge and proficiency in EBP.
Keywords: cross-sectional study, evidence-based healthcare, evidence-based practice, physiotherapy, Saudi Arabia
BACKGROUND
Healthcare supported by evidence-based practice (EBP) is essential for professionals of all cultural backgrounds. This relates to physicians,1 psychiatrists,2 dentists,3 nurses4,5 and physiotherapists.6,7 EBP implementation has been associated with positive results and improved practitioners’ decisions.8 According to Sackett et al.,9 EBP is defined as ‘the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients’. It has been reported that to make a valid decision using EBP, the following three major requirements must be fulfilled: the availability of best, recent, valid and relevant evidence; the involvement of those people who will receive the care; and support via knowledge and experience of those people who will be providing that care.10 Therefore, EBP provides the best available interventions to patients to improve their health. Although many studies have identified five steps in EBP implementation,11–13 there are some suggesting six steps,14 and others identifying seven steps.15,16 Nevertheless, the main aim of all these classifications is similar, which is to translate the acquired knowledge into practice to provide the best care for patients. The World Confederation for Physical Therapy (WCPT) stated that EBP should be considered as an opportunity for physiotherapists, and not a threat, as the current physiotherapy literature has high-quality evidence that can be used to demonstrate the valuable contribution of physiotherapy in treating several health conditions.17 In addition, it promotes the development of physiotherapy.
Healthcare providers in Saudi Arabia are classified under three sectors18: Ministry of Health (MOH) is the main government body that provides and finances for healthcare services in Saudi Arabia, including all public hospitals, centres and facilities. Other government healthcare sectors are hospitals that are operated by a specific government division and separated from MOH. These hospitals are considered public hospitals, but most of these hospitals only serve members and their families of those who are working in these divisions such as National Guard Health Affairs, Johns Hopkins Aramco Healthcare, Armed Forces Hospitals, Security Forces Hospitals and Royal Commission Hospitals. In addition, other hospitals like King Faisal Specialist Hospital and Research Centre can be accessed with a referral. Private sector includes all other healthcare hospitals, clinics, laboratories and pharmacies that are not operated by the government. All physiotherapy practitioners need to register with the Saudi Commission for Health Specialties (SCHS) in order to practice as physiotherapists in Saudi Arabia.19
According to a statistical report conducted by Saudi MOH in 2012,18 the total number of physiotherapists registered in MOH hospitals was 2495. Only 852 of them were physiotherapy specialists (male = 572; female = 280), whereas 1643 were physiotherapy technicians (male = 1072; female = 571). In addition, the majority of physiotherapy practitioners were men (66%) and most of them were from Saudi Arabia itself (84.6%). Although a large number of patients received care in physiotherapy, its services have not been involved as primary health care.20 Furthermore, although physiotherapists are permitted to make assessments for patients, design plans of care and apply treatments,19 patients do not have the ability to access physiotherapy services directly in MOH hospitals, but they can refer themselves to private practice.
The need for physiotherapy practice has been identified in Saudi Arabia, as evidenced by an increased enrolment in bachelor's and doctor of physical therapy (DPT) degrees in physiotherapy.19 The first physiotherapy degree course in Saudi Arabia started nearly 30 years ago. Currently, 16 universities offer an undergraduate physiotherapy degree,19 but only two of these universities offer a postgraduate (MSc) degree.21,22 There is no doctoral level program for physiotherapy in Saudi Arabia.19 This indicates that there are limited number of physiotherapy programmes in Saudi Arabia, particularly in the postgraduate level. Moreover, the concept of EBP concept has not been discussed widely in the research sphere in Saudi Arabia. Indeed, there are only a few recent Saudi studies that have recognized the need for EBP implementation within physiotherapy23 and medical24 curricula. In addition, it has been suggested that the use of EBP in Saudi Arabia may assist in improving hospital and nursing performance.25 However, the evidence of EBP implementation by Saudi healthcare professionals is limited. A comprehensive review investigated the quality of primary healthcare in Saudi Arabia and indicated an inadequate implementation of evidence-based healthcare.26 The review revealed that clinical judgments of some physicians are not supported by evidence-based medicine (EBM), and that this has led to inappropriate assessments and interventions, inadequate clinical judgements and unsafe practices. However, it is important to acknowledge that this review was relatively old and did not include any study that investigated about physiotherapists as the focus of the review was on physicians and/or may due to the lack of evidence regarding physiotherapy practice in Saudi Arabia. Therefore, its results should be treated with caution.
WCPT has emphasized that physiotherapists need specific skills to apply EBP like that of searching for evidence and being able to critically appraise research articles and the capability to evaluate their practice after implementation.17 Therefore, teaching EBP and research methods to physiotherapists will provide an opportunity to keep the profession familiar with up-to-date evidence. It has been previously suggested that teaching EBP to students can help increase knowledge and confidence when they start using research terms.27 A scoping review suggested that before endorsing the EBP steps/cycle, it is important to identify the knowledge needs of physiotherapists and any knowledge gaps that may exist.28 Therefore, teaching EBP within undergraduate and graduate curricula must focus on addressing the needs of healthcare professionals rather than on the skills of EBP. The use of EBP by physiotherapists in Saudi Arabia has not been investigated. Therefore, the purpose of this study is to determine physiotherapists’ behaviour, attitudes, awareness and knowledge towards EBP and to investigate the barriers of EBP implementation in Saudi Arabia. In addition, this study also aims to examine the association between demographic variables and physiotherapists’ attitudes, awareness and knowledge.
METHODS
Design, sample and participants
A cross-sectional descriptive design with a convenience sample was employed. The participants of the study were physiotherapists who are working in Saudi Arabia in a clinical or academic setting. Both genders and all nationalities were considered in this study. Undergraduate and internship physiotherapy students were excluded as the expected outcome of this study would inform about post-professional educational developments.
Data collection
The data were collected through an online survey using a validated website (www.surveymonkey.com). All information collected was anonymous and only the authors had access to the data. The study was approved by the research committee of the Physiotherapy Department, Faculty of Applied Medical Sciences, Umm Al-Qura University, Mecca, Saudi Arabia.
The survey was structured and designed considering Saudi Arabia's healthcare environment and the relevant cultural influences. In addition, the authors obtained necessary information about EBP surveys based on previous validated sources, including an EBP profile questionnaire29 created by the University of South Australia, and some previous studies with similar objectives30,31 to develop a suitable survey for the target participants. Although the structured survey was developed after referring the previous surveys, it was considerably different due to the difference in present research. In addition, as there are varied number of steps in EBP cycle, this study formulated the survey questions based on Sackett et al.13 five steps in EBP cycle. The survey was implemented over a 5-month timeframe from May 2016 to September 2016. The survey was sent out via social media platforms (Facebook, Twitter, and Instagram), WhatsApp and e-mail. Several reminders were sent out on a monthly basis to promote participation in the study. Based on a sample size calculation, including a 95% confidence interval, a 0.5 null hypothesis proportion and a margin of error of ±5%, the required sample size for this study was 385 responses. This study stopped receiving responses after the total target number of replies was achieved.
Survey structure
The survey consisted of 14 closed-ended questions with the following main elements:
-
(1)
Demographics: This included details such as gender, age, nationality, highest level of education and the university at which the respondent studied, work setting and job title.
-
(2)
Behaviour: Six items were created to determine the research and other sources used by physiotherapists during their daily clinical practice as assessed by a Likert scale ranging from always (1) to never (5). These sources were as follows: (A) personal experience, (B) colleagues opinions, (C) supervisor or expert opinions, (D) internet, (E) books, (F) research reviews and articles.
-
(3)
Attitudes: Four items with a Likert scale ranging from strongly disagree (1) to strongly agree (5) were included to determine physiotherapists’ attitudes towards the use of research in practice. A scoring system of maximum 20 was applied. Each answer option received a different score as following: strongly disagree (score = 1), disagree (score = 2), neutral (score = 3), agree (score = 4), strongly agree (score = 5). Higher scores indicated higher level of attitudes towards EBP implementation.
-
(4)
Awareness: 14 items related to research terminologies were used to assess the physiotherapists’ awareness of EBP. There were five answer options to each question, where each answer had a different score: never heard of it (score = 0), have heard of it but do not understand it (score = 1), understand it a little (score = 2), understand it very well (score = 3), understand it completely and could explain it to others (score = 4). Across all 14 questions, the maximum overall score was 56. Higher scores indicated a higher level of awareness towards EBP implementation.
-
(5)
Knowledge: Six items with three answer options each: (1) agree, (2) disagree and (3) unsure were used. These questions were set to examine physiotherapists’ knowledge pertaining to EBP implementation. They were also structured to allow only one valid answer, which was the second answer (disagree) for all six items; this received two points (for each item) giving a maximum total score of 12, and other answers (agree, unsure) received a score of zero. Higher scores indicated a higher level of knowledge about the use of EBP. It is important to note that it may not be suitable to score ‘unsure’ option to receive a score of 1 as this question aimed to test knowledge. Thus, the participants who selected ‘unsure’ option perhaps did not acknowledge this information and may be similar to participants who selected the wrong answer (agree).
-
(6)
Formal training: Two questions to identify physiotherapists who had previously received formal EBP training from the following options: EBP course as part of university education ‘BSc, MSc, PhD’, EBP workshops and lectures that are organized by the healthcare providers in Saudi Arabia or an online EBP training offered by accredited organizations.
-
(7)
Barriers: The final question included six items regarding possible barriers to EBP implementation. This question was aimed to determine the level of importance to participants regarding EBP barriers to them. This element was assessed by a ranking scale ranging from 1 (the least important barrier) to 10 (the most important barrier).
Reliability test
A pilot test was conducted to assess the clarity and the accuracy of the survey involving 20 physiotherapists. The main aim of performing the reliability test was to assess the logistics of the method and identify any issues in language. In addition, feedback obtained during the pilot test informed modifications to the survey, and the final version of the survey was determined following several consensus meetings amongst the authors. The internal consistency (Cronbach's alpha) was assessed, which indicated an acceptable overall reliability, yielding a value of 0.780. The reliability for each survey item was as follows: behaviour (0.601), attitudes (0.954), awareness (0.934), knowledge (0.805), EBP training (0.584) and barriers (0.800). It is important to note that the reliability of the EBP training section was poor as the two questions pertaining to this were having different format. The first question was a yes and no question, while the second one was a multiple choice question. Only participants who selected their answer to be ‘yes’ in the first question had to answer the second question, whereas participants who selected their answer to be ‘no’ could skip the second question. As a result, this difference in the format of both questions may have affected the reliability level. Although this section should have been removed due to its impact on the overall reliability of the survey, it was useful to determine the number of participants who had previously undergone EBP training and those who had not. Also, it was necessary to identify the issues regarding EBP training as it assisted in providing an overview of the current situation in terms of health education in Saudi Arabia.
Data analysis
Incomplete questionnaires with more than two missing answers were discarded. The data were recorded and analysed using IBM SPSS version 19.0 (Armonk, NY: IBM Corp). The percentages and frequencies of the participants’ responses to each question were analysed and reported. The median score was calculated to identify the middle score in the distribution of participants’ attitudes, awareness and knowledge scores, which assisted to classify the participants into two groups: a group with a higher score than the median score, and a group with an equal or lower score than the median score. Consequently, the results of this calculation were converted into percentages. Pearson's chi-square test (two-sided significance) was performed to examine the association of attitudes, awareness and knowledge scores in relation to the demographics of the participants. The result was considered statistically significant when P < 0.05. Data were reported either in narrative description or quantitative summary as appropriate.
RESULTS
Sample and demographics
A total of 604 respondents participated in the study, but only 385 respondents provided complete information in their questionnaires (64%). Out of these, nine participants were excluded; seven of who were undergraduate physiotherapy students and two others were not physiotherapists (Fig. 1). The final number of participants included in data analysis was 376. Therefore, this study did not achieve the required number of responses by power analysis (385) because nine participants were excluded. Table 1 shows the demographics of participating physiotherapists.
Figure 1.
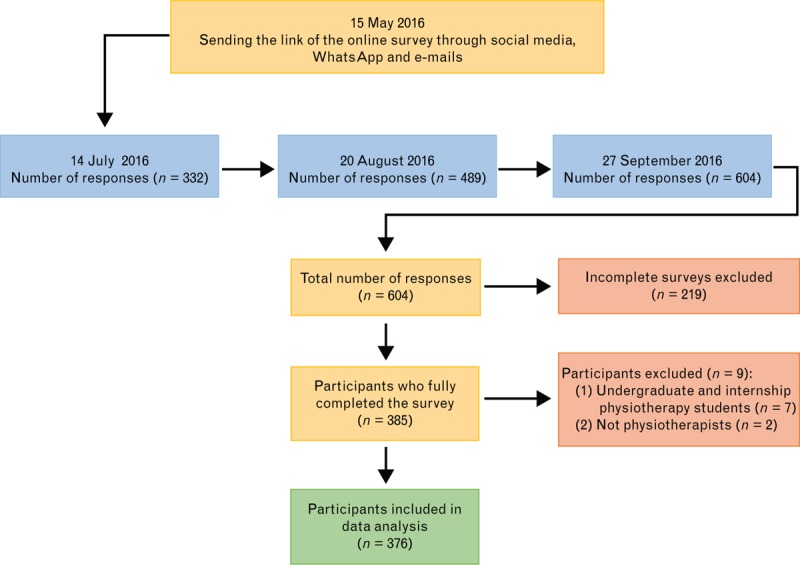
Flow diagram of the study.
Table 1.
Demographics of study participants
| Variable | Demographic | N (%) |
| Gender | Male | 227 (60.4) |
| Female | 149 (39.6) | |
| Age | 20–25 | 118 (31.4) |
| 26–30 | 119 (31.6) | |
| 31–35 | 73 (19.4) | |
| 36–40 | 34 (9.0) | |
| 41 or more | 32 (8.5) | |
| Nationality | Saudi | 319 (84.8) |
| Non-Saudi | 57 (15.2) | |
| Educationa | Diploma | 18 (4.8) |
| BSc | 249 (66.2) | |
| DPT | 3 (0.8) | |
| MSc | 75 (19.9) | |
| PhD | 31 (8.2) | |
| Universityb | King Saud University (Saudi Arabia) | 63 (16.8) |
| Jazan University (Saudi Arabia) | 39 (10.4) | |
| Umm Al-Qura University (Saudi Arabia) | 30 (8) | |
| King Abdulaziz University (Saudi Arabia) | 23 (6.1) | |
| Cairo University (Egypt) | 16 (4.3) | |
| University of Pittsburgh (United States of America) | 9 (2.4) | |
| Cardiff University (United Kingdom) | 8 (2.1) | |
| Loma Linda University (United States of America) | 8 (2.1) | |
| Work setting | Ministry of Health (all public ‘government’ hospitals and public rehabilitation centres) | 153 (40.7) |
| Private health sectors (all private hospitals, centres and clinics) | 62 (16.5) | |
| Other health sectors (such as National Guard Health Affairs, Johns Hopkins Aramco Healthcare, Armed Forces Hospitals, Security Forces Hospitals and Royal Commission Hospitals) | 100 (26.6) | |
| University ‘academic’ | 61 (16.2) | |
| Job titlec | Technician | 26 (6.9) |
| Specialist | 240 (63.8) | |
| Senior Specialist | 44 (11.7) | |
| Consultant | 8 (2.1) | |
| Teaching Assistant | 21 (5.6) | |
| Lecturer | 19 (5.1) | |
| Assistant Professor | 11 (2.9) | |
| Associate Professor | 7 (2.7) | |
| Professor | 0 (0) |
aThe highest qualification received by participants.
bOnly eight universities of 65 different universities were reported; top four Saudi universities and top four non-Saudi universities.
cJob title descriptions:
(1) Technician: Two years diploma after the secondary school certificate.
(2) Specialist: Bachelor's degree with one year of internship or MSc degree before acquiring the required experiences for classification into senior specialist rank.
(3) Senior Specialist: MSc degree after completing the required experience so that the training period and later experience shall equate to a total of four years or PhD degree before completing the required experience for classification into consultant rank.
(4) Consultant: PhD degree with at least three years of experience.
(5) Teaching Assistant: Bachelor's degree holders.
(6) Lecturer: MSc degree holders.
(7) Assistant Professor: PhD holders.
(8) Associate Professor: PhD holders with at least four years of experiences as an assistant professor and completing the required number of research articles.
(9) Professor: PhD holders with at least four years of experiences as an associate professor and completing the required number of research articles.
The majority of the participants were male (60.4%), and in the age group of 20–30 (63%). Almost all participants were from Saudi Arabia (84.8%) with most of them having completed their bachelor's degree (66.2%) and a small proportion with a master's and PhD degree. Approximately 68.1% of participants obtained their highest degree from a university in Saudi Arabia and 28.2% obtained it from universities abroad, and 3.7% of the respondents were not clear about this, or did not provide any information pertaining to this. Almost all the participants worked in a clinical setting (83.8%). These settings particularly included the Ministry of Health (40.7%), private health sector (16.5%), and other health sectors (26.6%). Only 16.2% of the participants worked in an academic setting.
Behaviour and attitude to evidence-based practice
The findings of physiotherapists’ behaviour towards the use of research and other sources revealed that most of the physiotherapists who took part in this study based their clinical decisions ‘always or often’ on personal experiences (75.6%), followed by books (59.9%), research reviews and articles (56.9%), supervisor or expert opinions (50.5%), internet (49%) and colleagues’ opinions (10.5%) (Table 2). However, in general, a positive attitude towards the use of research in practice (81–95%) among physiotherapists was observed. Approximately 84.3% agreed or strongly agreed that research theory and methodology should be included in the curriculum of physiotherapy adopted in educational institutions across Saudi Arabia, and 86.4% felt that understanding research designs and methods was important in the practice of physiotherapy. In addition, 95% of participants believed that reading relevant articles was essential for their practice and 81.4% of physiotherapists agreed or strongly agreed that interventions should be supported by evidence (Table 3).
Table 2.
Participants’ behaviour to the use of research and other sources when making daily clinical decisions
| Sources | N (%) | ||||
| Always | Often | Sometimes | Rarely | Never | |
| My personal experience | 127 (33.8) | 157 (41.8) | 83 (22.1) | 9 (2.4) | 0 (0) |
| My colleagues’ opinions | 29 (7.7) | 97 (2.8) | 198 (52.7) | 45 (12) | 7 (1.9) |
| My supervisor or expert opinions | 64 (17) | 126 (33.5) | 149 (39.6) | 30 (8) | 7 (1.9) |
| Internet | 80 (21.3) | 104 (27.7) | 132 (35.1) | 48 (12.8) | 12 (3.2) |
| Books | 98 (26.1) | 127 (33.8) | 104 (27.7) | 44 (11.7) | 3 (0.8) |
| Research reviews and articles | 115 (30.6) | 99 (26.3) | 106 (28.2) | 51 (13.6) | 5 (1.3) |
Table 3.
Participants’ attitudes towards evidence-based practice implementation
| Items | N (%) | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Understanding of research methods and research designs is important in physiotherapy practice | 11 (2.9) | 8 (2.1) | 32 (8.5) | 149 (39.6) | 176 (46.8) |
| Research theory and methodology should be included in the physiotherapy curriculum | 9 (2.4) | 13 (3.5) | 37 (9.8) | 143 (38) | 174 (46.3) |
| Physiotherapists need to read relevant articles regularly to update their knowledge | 8 (2.1) | 4 (1.1) | 6 (1.6) | 87 (23.1) | 271 (72.1) |
| Physiotherapists should apply treatments that are supported by evidence | 9 (2.4) | 7 (1.9) | 54 (14.4) | 133 (35.4) | 173 (46) |
The results revealed that the median score percentage of physiotherapists’ attitudes in relation to EBP implementation was 90% (score = 18/20). There was a significant association between participants’ attitudes score and their education level (P < 0.001), whereas no significant associations were found on other demographics data (Table 4). This study found that those with a PhD (51.7%) and master's degree (53.3%) were more likely to have a higher attitude score percentage of 90% than those with a BSc (33.7%), DPT (33.3%) or diploma (27.8%).
Table 4.
Association between participants’ attitudes score percentage and their characteristics
| Variable | Characteristics | Participants attitudes scorea N (%) | Chi-square test | P | |
| Median ≤90% | Median >90% | ||||
| Gender | Male | 134 (59) | 93 (41) | 10.67 | 0.638 |
| Female | 96 (64.5) | 53 (35.5) | |||
| Age | 20–25 | 85 (72.1) | 33 (27.9) | 61.98 | 0.162 |
| 26–30 | 65 (54.7) | 54 (45.3) | |||
| 31–35 | 47 (64.4) | 26 (35.6) | |||
| 36–40 | 16 (47.1) | 18 (52.9) | |||
| 41 or more | 17 (53.2) | 15 (46.8) | |||
| Nationality | Saudi | 200 (62.7) | 119 (37.3) | 10.67 | 0.638 |
| Non-Saudi | 30 (52.7) | 27 (47.3) | |||
| Education | Diploma | 13 (72.2) | 5 (27.8) | 1.06 | 0.000* |
| BSc | 165 (66.3) | 84 (33.7) | |||
| DPT | 2 (66.7) | 1 (33.3) | |||
| MSc | 35 (46.7) | 40 (53.3) | |||
| PhD | 15 (48.3) | 16 (51.7) | |||
| Work setting | Ministry of Health | 102 (66.7) | 51 (33.3) | 52.28 | 0.076 |
| Private health sectors | 43 (69.4) | 19 (30.6) | |||
| Other health sectors | 59 (59) | 41 (41) | |||
| University ‘academic’ | 26 (42.7) | 35 (57.3) | |||
| Job title | Technician | 16 (61.6) | 10 (38.4) | 1.01 | 0.217 |
| Specialist | 158 (65.9) | 82 (34.1) | |||
| Senior Specialist | 27 (61.4) | 17 (38.6) | |||
| Consultant | 5 (62.5) | 3 (37.5) | |||
| Teaching Assistant | 8 (38.1) | 13 (61.9) | |||
| Lecturer | 8 (42.2) | 11 (57.8) | |||
| Assistant Professor | 7 (63.7) | 4 (36.3) | |||
| Associate Professor | 1 (14.3) | 6 (85.7) | |||
| EBP training | Yes | 59 (52.7) | 53 (47.3) | 18.15 | 0.152 |
| No | 171 (64.8) | 93 (35.2) | |||
aMedian attitudes score among participants in this study was 90%.
*Statistically significant difference.
Awareness and knowledge of evidence-based practice
The participants’ awareness of EBP phrases and terms varied: 23.1% of participants had never heard of the term ‘EBP’ and 30.9% were not aware of the EBP steps/cycle, whereas 29.8 and 12.2% of the participants completely understood the term EBP and EBP steps/cycle, respectively. In relation to more complex EBP terms, 57.7% of participants had never heard of the term ‘forest plot’ and only 6.9% reported to have completely understood the term. Moreover, 40.2% had never heard the term ‘Population/Patient, Intervention, Comparison, Outcome (PICO)’ and only 21% completely understood that term. However, the participants were aware regarding some other terms such as ‘systematic review’ (64.9%, understood this completely or very well) and ‘randomized controlled trial’ (60.6%, understood this completely or very well) (Table 5).
Table 5.
Participants’ awareness towards evidence-based practice implementation
| Terms or phrases | N (%) | ||||
| Never heard it | Have heard it but do not understand | Understand a little | Understand very well | Understand completely and could explain to others | |
| EBP as a term | 87 (23.1) | 37 (9.8) | 52 (13.8) | 88 (23.4) | 112 (29.8) |
| EBP steps/cycle | 116 (30.9) | 51 (13.6) | 85 (22.6) | 78 (20.7) | 46 (12.2) |
| Quality of evidence | 28 (7.4) | 34 (9) | 103 (27.4) | 120 (31.9) | 91 (24.2) |
| Systematic review | 23 (6.1) | 38 (10.1) | 71 (18.9) | 113 (30.1) | 131 (34.8) |
| Randomized controlled trial | 44 (11.7) | 35 (9.3) | 69 (18.4) | 97 (25.8) | 131 (34.8) |
| PICO | 151 (40.2) | 45 (12) | 57 (15.2) | 44 (11.7) | 79 (21) |
| Critical appraisal | 108 (28.7) | 62 (16.5) | 76 (20.2) | 54 (14.4) | 76 (20.2) |
| Forest plot | 217 (57.7) | 45 (12) | 51 (13.6) | 37 (9.8) | 26 (6.9) |
| Relative risk | 63 (16.8) | 48 (12.8) | 102 (27.1) | 93 (24.7) | 70 (18.6) |
| Likelihood ratio | 144 (38.3) | 48 (12.8) | 88 (23.4) | 48 (12.8) | 48 (12.8) |
| Confidence interval | 96 (25.5) | 63 (16.8) | 88 (23.4) | 63 (16.8) | 66 (17.6) |
| Effect size | 67 (17.8) | 40 (10.6) | 84 (22.3) | 91 (24.2) | 94 (25) |
| Risk of bias | 85 (22.6) | 47 (12.5) | 71 (16.2) | 81 (21.5) | 92 (24.5) |
| Healthcare databases | 70 (18.6) | 39 (10.4) | 61 (16.2) | 73 (19.4) | 133 (35.4) |
EBP, evidence-based practice; PICO, Population/Patient, Intervention, Comparison, Outcome.
With regard to the level of knowledge, there were significant issues. For example, only 10.1% of the participants correctly defined EBP and only 19.4% rightly understood the aim of EBP. Only 32.2% were aware that EBP implementation required a long period. Furthermore, some participants acknowledged that the recognition of patients’ values (43.1%) and personal experiences (43.9%) were important requirements for EBP implementation (Table 6). Most physiotherapists (70.2%) had no formal training in EBP (Table 7).
Table 6.
Participants’ knowledge towards evidence-based practice implementation
| Items | N (%) | ||
| Agree | Disagree | Unsure | |
| EBP is a process of systematic investigation to generate knowledge and test theories | 202 (53.7) | 38 (10.1) | 136 (36.2) |
| The main aim of EBP is to identify the causes of research problems and how to solve them | 156 (41.5) | 73 (19.4) | 147 (39.1) |
| Physiotherapy interventions are mostly supported by EBP | 172 (45.7) | 59 (15.7) | 145 (38.6) |
| Patient's values and preferences are not one of the main requirements of EBP | 70 (18.6) | 162 (43.1) | 144 (38.3) |
| EBP does not take into consideration the clinical experience of the physiotherapist | 64 (17) | 165 (43.9) | 147 (39.1) |
| EBP requires a short period to search for, evaluate and integrate evidence into practice | 102 (27.1) | 121 (32.2) | 153 (40.7) |
EBP, evidence-based practice.
Table 7.
Participants’ responses regarding evidence-based practice training
| Items | Answers | N (%) |
| Have you formally undertaken any training in EBP? | Yes | 112 (29.8) |
| No | 264 (70.2) | |
| If yes, what type of training course have you been involved in? | EBP course as part of university education | 57 (50.9) |
| Comprehensive course (11 to 20 hours) | 12 (10.7) | |
| Short course (3 to 10 hours) | 27 (24.1) | |
| One lecture (1 to 2 hours) | 13 (11.6) | |
| All of the above | 2 (1.8) | |
| Not reported | 1 (0.9) |
EBP, evidence-based practice
The results revealed that median score percentages of physiotherapists’ awareness and knowledge, in relation to EBP implementation, were 50% (score = 28/56) and 16.7% (score = 2/12), respectively. There was a significant association between participants’ awareness score and education level (P < 0.001), university (P < 0.01), work setting (P < 0.05), job title (P < 0.001) and participants who had received EBP training (P < 0.001). Factors not associated with awareness scores include gender, age and nationality (Table 8). This study found that those with a PhD (90.3%) and master's (80%) were more likely to have a higher awareness score percentage of 50% than those with a BSc (35%), DPT (66.7%) and Diploma (27.8%). In addition, academic physiotherapists (77%) were more likely to have a higher awareness score percentage of 50% than other clinical physiotherapists (39.9–48%), as well as physiotherapists who had EBP training (82.1%) when compared with physiotherapists who did not (34%). Furthermore, a more senior position was associated with a higher awareness score among physiotherapists.
Table 8.
Association between participants’ awareness score percentage and their characteristics
| Variable | Characteristics | Participants awareness scorea N (%) | Chi-square test | P | |
| Median ≤ 50% | Median > 50% | ||||
| Gender | Male | 109 (48) | 118 (52) | 47.34 | 0.759 |
| Female | 85 (57) | 64 (43) | |||
| Age | 20–25 | 76 (64.4) | 42 (35.6) | 242.34 | 0.144 |
| 26–30 | 72 (60.5) | 47 (39.5) | |||
| 31–35 | 26 (35.6) | 47 (64.4) | |||
| 36–40 | 10 (29.4) | 24 (70.6) | |||
| 41 or more | 10 (31.2) | 22 (68.8) | |||
| Nationality | Saudi | 173 (54.2) | 146 (45.8) | 48.17 | 0.731 |
| Non-Saudi | 21 (36.8) | 36 (63.2) | |||
| Education | Diploma | 13 (72.2) | 5 (27.8) | 341.11 | 0.000* |
| BSc | 162 (65) | 87 (35) | |||
| DPT | 1 (33.3) | 2 (66.7) | |||
| MSc | 15 (20) | 60 (80) | |||
| PhD | 3 (9.7) | 28 (90.3) | |||
| Work setting | Ministry of Health | 92 (60.1) | 61 (39.9) | 197.36 | 0.043* |
| Private health sectors | 34 (54.8) | 26 (45.2) | |||
| Other health sectors | 52 (52) | 48 (48) | |||
| University ‘academic’ | 14 (23) | 47 (77) | |||
| Job title | Technician | 18 (69.2) | 8 (30.8) | 511.75 | 0.000* |
| Specialist | 145 (60.4) | 95 (39.6) | |||
| Senior Specialist | 14 (31.8) | 30 (68.2) | |||
| Consultant | 2 (25) | 6 (75) | |||
| Teaching Assistant | 9 (42.9) | 12 (57.1) | |||
| Lecturer | 4 (21) | 15 (79) | |||
| Assistant Professor | 2 (18.2) | 9 (81.8) | |||
| Associate Professor | 0 (0) | 7 (100) | |||
| EBP training | Yes | 20 (17.9) | 92 (82.1) | 149.67 | 0.000* |
| No | 174 (66) | 90 (34) | |||
aMedian awareness score among participants in this study was 50%.
*Statistically significant difference.
There was also a significant association between participants’ knowledge score and demographics data (Table 9) with regard to age (P < 0.05), education level (P < 0.001), university (P < 0.001), work setting (P < 0.001), job title (P < 0.001) and participants who had EBP training (P < 0.001). Older physiotherapists were more likely to have a higher knowledge score percentage of 16.7% than younger physiotherapists. In addition, those with a PhD (80.7%) and MSc (66.7%) were more likely to have a higher knowledge score percentage of 16.7% than those with less education, such as BSc (41.4%) and diploma (22.2%). Furthermore, a more senior position was associated with a higher knowledge score among physiotherapists, for example, consultant (75%) compared with technician (23%), or assistant professor (81.8%) compared with teaching assistant (57.1%). In addition, academic physiotherapists (64%) were more likely to have a higher knowledge score percentage of 16.7% than other clinical physiotherapists (34.6–46.8%), except physiotherapists working in other health sectors, such as National Guard health affairs and armed forces hospitals (63%) and physiotherapists who had EBP training (76.8%) compared with physiotherapists who did not (37.1%).
Table 9.
Association between participants’ knowledge score percentage and their characteristics
| Variable | Characteristics | Participants knowledge scorea N (%) | Chi-square test | P | |
| Median ≤ 16.7% | Median > 16.7% | ||||
| Gender | Male | 109 (48) | 118 (52) | 5.78 | 0.448 |
| Female | 83 (55.7) | 66 (44.3) | |||
| Age | 20–25 | 75 (63.6) | 43 (36.4) | 39.09 | 0.027* |
| 26–30 | 60 (50.4) | 59 (49.6) | |||
| 31–35 | 35 (48) | 38 (52) | |||
| 36–40 | 10 (29.4) | 24 (70.6) | |||
| 41 or more | 12 (37.5) | 20 (62.5) | |||
| Nationality | Saudi | 166 (52) | 153 (48) | 7.15 | 0.306 |
| Non-Saudi | 26 (45.6) | 31 (54.4) | |||
| Education | Diploma | 14 (77.8) | 4 (22.2) | 61.05 | 0.000* |
| BSc | 146 (58.6) | 103 (41.4) | |||
| DPT | 1 (33.3) | 2 (66.7) | |||
| MSc | 25 (33.3) | 50 (66.7) | |||
| PhD | 6 (19.3) | 25 (80.7) | |||
| Work setting | Ministry of Health | 100 (65.4) | 53 (34.6) | 50.46 | 0.000* |
| Private health sectors | 33 (53.2) | 29 (46.8) | |||
| Other health sectors | 37 (37) | 63 (63) | |||
| University ‘academic’ | 22 (36) | 39 (64) | |||
| Job title | Technician | 20 (77) | 6 (23) | 111.96 | 0.000* |
| Specialist | 139 (58) | 101 (42) | |||
| Senior Specialist | 10 (22.7) | 34 (77.3) | |||
| Consultant | 2 (25) | 6 (75) | |||
| Teaching Assistant | 9 (42.9) | 12 (57.1) | |||
| Lecturer | 7 (36.8) | 12 (63.2) | |||
| Assistant Professor | 2 (18.2) | 9 (81.8) | |||
| Associate Professor | 3 (42.8) | 4 (57.2) | |||
| EBP training | Yes | 26 (23.2) | 86 (76.8) | 71.19 | 0.000* |
| No | 166 (62.9) | 98 (37.1) | |||
aMedian knowledge score among participants in this study was 16.7%.
*Statistically significant difference.
Perceived barriers to the use of evidence-based practice
Figure 2 demonstrates the barriers to EBP implementation reported by participants, with insufficient teaching in previous education being identified most often (43.1%), followed by lack of research knowledge and skills (36.4%), lack of funding and resources (35.7%), lack of support and encouragement (30.6%), lack of interest (23.4%) and lack of time (22.8%).
Figure 2.
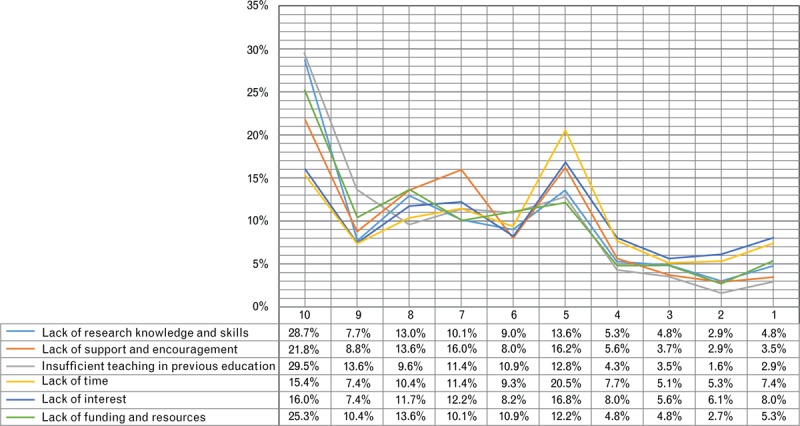
Perceived barriers towards evidence-based practice (EBP) implementation among physiotherapists in Saudi Arabia, where 1 is the least important barrier and 10 is the most important barrier.
DISCUSSION
This study found a limited awareness and knowledge of EBP implementation among the majority of physiotherapists in Saudi Arabia. In addition, the findings confirmed that there were significant associations between some physiotherapists’ demographics (such as education level, work setting, job title and physiotherapists who had received EBP training), awareness and knowledge of EBP. The present study received more than 600 replies, but only 376 responses included in the data analysis, which according to a Saudi MOH report in 201218 represents 15% of physiotherapists (376/2495) in Saudi Arabia. However, it is likely that the number of physiotherapists has increased since 2012. In addition, this report only calculated the number of physiotherapists working in MOH hospitals and its facilities, and does not include physiotherapists working in private and other government health sectors, including staff members from universities.
Behaviour and attitude to evidence-based practice
In the present study, it was found that Saudi Arabia physiotherapists may rely more on personal experiences and much less on research articles and reviews. This finding was opposite to some previous studies, for example, Brazilian physiotherapists used research articles as the first source for their clinical decisions (89.5%), followed by information gained from attending practical courses (88.3%) and then from books (86.3%).32 However, our participants may have some misunderstandings regarding the relationship between the importance of research articles and practice which may explain why they reported that their personal experiences were the first source in making clinical judgements.
This study indicated a positive attitude towards the use of EBP, with most participants responding ‘agree’ or ‘strongly agree’ (81–95%) with regards to the importance of research in practice. Approximately, 95% of the participants believed that reading relevant articles was essential for their practice and 81.4% of physiotherapists agreed that interventions should be supported by evidence. The findings are in alignment with the literature,30,32–36 for example, Swedish healthcare professionals, including physiotherapists, occupational therapists and dieticians, had positive attitudes towards EBP implementation.33 Similar results were also found among American Physical Therapy Association members.30 In a Colombian study, 71.6% of physiotherapists agreed that EBP is essential and 61.3% believed that literature was useful for practice,35 whereas a Brazilian study reported that 92.2% of physiotherapists agreed or strongly agreed that EBP was essential for their practice, also, 89% believed that EBP improves patient care.32 Furthermore, a Canadian study reported that 78% of physiotherapists agreed that there were benefits to using research findings in their practice.36
Although there is no study in Saudi Arabia that assessing the use of EBP among physiotherapists, there have been two Saudi studies investigating the use of EBM among primary healthcare physicians in the regions of Riyadh37 and Asir.38 Both studies reported similar results and found that most physicians in Saudi Arabia had positive attitudes towards the use of EBM. In addition, the majority of physicians (93%) agreed that there were benefits to the use of EBM for improving patient care and 92% of them found that research findings were useful in practice.38
This study found a significant association between physiotherapists’ attitude scores and their education level (P < 0.001), PhD and MSc degree holders were more likely to have positive attitudes towards EBP implementation as compared with BSc and diploma holders. Some studies found that there were association between demographics and physiotherapists attitudes.30,36 Salbach et al.36 reported that there were associations between physiotherapists’ attitudes and physiotherapists’ characteristics that includes age, sex, highest degree, work hours per week, working in a multidisciplinary team, supervision of physiotherapist students and participation in research. They reported that participants who held a bachelor's degree were more likely to agree or strongly agree that EBP improves patient care, as compared with diploma holders.
A systematic review found a positive association between attitudes and increased research utilization, which may indicate that having a positive attitude is one of the most crucial factors for EBP application.39 Furthermore, Nelson and Steele40 reported that the practitioner's attitude is a significant predictor of self-reported EBP use, and the association between clinical setting and EBP use was mediated by practitioners’ attitudes towards the use of research. Therefore, for increasing the EBP implementation, the attitude of each individual should be considered.
Awareness and knowledge of evidence-based practice
The current study distinguished between awareness and knowledge. Considering awareness, physiotherapists had good awareness levels of some research terms since they reported that they completely or very well understood terms such as ‘systematic reviews’ (64.9%), ‘randomized controlled trial’ (60.6%) and ‘quality of evidence’ (56.1%). The three terms that physiotherapists least understood were ‘forest plot’ (16.7%), followed by ‘likelihood ratio’ (25.6%) and ‘PICO’ (32.7%). However, some physiotherapists were unfamiliar even with basic terms such as EBP (32.9%) and EBP cycle/steps (44.5%). Regarding knowledge, most physiotherapists had poor understanding in terms of basic knowledge of EBP as 89.9% were not aware of the definition of EBP while 80.6% did not understand the aim of EBP. These findings were inconsistent with most of the previous studies.30,32–35 Silva et al.32 reported that most physiotherapists had a good level of knowledge; 77.3% partially or strongly agreed that they had a clear understanding of the use of research findings in practice and 71.1% were confident that they could implement EBP. Moreover, Australian physiotherapists also had a good level of knowledge; 98.4% understood the term ‘randomized controlled trials’ and 92.7% the term ‘systematic review’.34 In addition, more than 50% understood some complex research terms such as ‘relative and absolute risk’, ‘meta-analysis’, ‘effect size’ and ‘intention to treat’. Although the findings of the current study were somewhat similar to the study conducted by Heiwe et al.33 that showed that participants’ understanding of EBP terms was varied and based on the level of complexity in EBP terminologies, the main findings regarding physiotherapists’ awareness and knowledge vary considerably from previous studies. This may be due to many factors, such as the lack of discussion about EBP concept in the literature of Saudi Arabia, and its limited introduction into the Saudi Arabia's healthcare education system. In addition, there is a gap between academic and clinical physiotherapists which may result in misconceptions regarding the importance of EBP in a clinical setting among the latter group.
In this study, the median score of physiotherapists’ awareness towards the use of EBP was 28/56 (50%) and the median score of physiotherapists’ knowledge was 2/12 (16.7%). Also, there were significant associations between physiotherapists’ awareness and knowledge and their demographics including age, highest degree, work setting, job title and participants who had EBP training. Similar results were found by Salbach et al.36 who noted that there was an association between research skills (EBP self-efficacy) and participants’ characteristics, including age, sex, highest degree, and years of experiences in EBP. For example, the researchers found that participants with a higher degree, such as an MSc, were more likely to have a higher self-efficacy above 63% (63% is the median score of self-efficacy in percentage) as compared with participants with a BSc degree. Also, Jette et al.30 described similar results wherein they reported that physiotherapists’ knowledge was associated with age, years since licensure and highest degree held. In addition, Iles and Davidson34 found that physiotherapists with higher levels of training were more likely to search databases and understand EBP terms as compared with physiotherapists with lower levels of training.
In the current study, it was found that most physiotherapists had no formal EBP training (70.2%). This contrasts with previous studies such as Jette et al.,30 who reported that 67% of their respondents had formal training in the critical appraisal of research literature, and Ramírez-Vélez et al.35 who found that 88% had been exposed to basic knowledge about EBP. Thus, there is a significant issue regarding EBP training in Saudi Arabia, which needs to be addressed.
Perceived barriers to the use of evidence-based practice
The identification of barriers is important and should be considered the first step towards determining the issues surrounding the limited use of EBP.41 In the present study, insufficient teaching in previous educational contexts was the primary barrier to EBP use, while lack of time was the least important barrier for physiotherapists. This finding differed from most of previous studies as many studies have identified lack of time as the major barrier for physiotherapists in relation to EBP use,30,33,34,36 followed by lack of generalizability of the research findings to their specific patient population and also their lack of research knowledge. Furthermore, other healthcare professionals, such as nurses42,43 and occupational therapists44 also identified insufficient time to be the most important barrier to the application of EBP to their practice. One of the possible explanations of why our participants did not rate ‘lack of time’ as their most important barrier to the use of EBP is that most participants may be not aware about the amount of time and effort which has been put into EBP use worldwide. In addition, based on our findings, most physiotherapists had no formal training in EBP. Therefore, their level of knowledge about EBP implementation may be insufficient and may have impacted on their understanding about the barriers of EBP. On the other hand, it seems possible that the workload of some hospitals in Saudi Arabia may not be overwhelming, which might explain why physiotherapists reported that lack of time was not the most important barrier to EBP use. However, the workload in Saudi hospitals may be varied based on the following factors: large cities compared with towns; MOH hospitals compared with private or other government hospitals; rehabilitation centres compared with small physiotherapy departments.
Recently, a systematic review investigated physiotherapists’ knowledge, skills, behaviour, opinions and barriers regarding EBP.45 This review looked at 12 studies and found that the major three barriers reported in these studies were lack of time, difficulties in understanding statistics and absence of support. However, Ramírez-Vélez et al.35 reported that a lack of research skills was the primary barrier for Colombian physiotherapists, in terms of EBP implementation, whereas difficulty in accessing full-text articles was the most frequent barrier for Brazilian physiotherapists.32 In Saudi Arabia, two studies reported that the primary barrier to the use of EBM among physicians was patient overload.37,38 Both studies also reported that lack of library was one of the top three barriers curbing EBP implementation. However, physicians’ barriers may not be on the same lines as that of physiotherapists’ barriers. Therefore, these two studies’ results cannot be generalized to physiotherapy context.
Generally, the results of the current study could be explained by the fact that the teaching of physiotherapy courses in Saudi Arabia was started late in comparison to other countries, such as the United States and United Kingdom, which may have impacted on the quality of education provided. Also, other factors may well be involved such as culture, the university policy system, misunderstandings concerning EBP, and a lack of interest on the part of some universities’ staff members. Therefore, these issues need to be addressed when implementing EBPs courses in Saudi physiotherapy programmes.
LIMITATIONS
Although the needed sample size was calculated, and the reliability of the survey used was acceptable, there were certain limitations. First, a convenience sampling type was used as we did not have access to all physiotherapists in Saudi Arabia which might have underpowered the generalizability of the study results. However, an attempt was made to send the survey for both clinical and academic physiotherapists in all main five geographical regions in Saudi Arabia to ensure the distribution of the survey and minimize the bias. Second, even though the overall reliability of the survey was acceptable, the reliability of one of the survey sections was poor. Third, the completion rate was 64% and the response rate was not possible to calculate because this study did not use a specific list group for contact. Fourth, there is a possibility of a response bias arising from the knowledge section due to the answer options. Fifth, the accuracy of the data is uncertain as the data were collected via a self-report survey. Therefore, self-perceptions of awareness/knowledge may not align with actual awareness/knowledge. In addition, Lanyon and Goodstein46 reported that there are potential biases that may exist in self-report surveys such as acquiescence response styles, social desirability bias, negative affectivity bias, extreme response styles. Thus, these possible biases must be taken into consideration. It has been shown that self-report surveys are the most valid method to assess beliefs, attitudes, and opinions, thus, it should be considered while conducting social research.47 Furthermore, it has a fundamental role in contributing to the higher education research and evaluation.48 Therefore, self-report survey was used to answer the research question of this study. Sixth, there are no recent adequate statistics regarding the number of physiotherapists in Saudi Arabia, which may also affect the generalizability of the findings. Finally, the survey structure did not include in-depth data, particularly on attitudes (only four items) and knowledge sections (only six items). Thus, these sections may not have indicated the exact level of attitudes and knowledge of the participants.
CONCLUSION
Physiotherapists’ awareness and knowledge towards EBP implementation were relatively low, indicating an evident gap in terms of their understanding and application of EBP in Saudi Arabia. Given that the majority of practicing physiotherapists reported no formal training in EBP (70.2%), there is a need to integrate concepts related to EBP into the undergraduate and graduate curricula. In addition, strategies must be developed and implemented to encourage practicing among physiotherapists for gaining the relevant knowledge and proficiency in EBP.
RECOMMENDATION
Physiotherapists, in particular those who are working in a clinical setting must increase their awareness and knowledge of research and EBP terms to understand and adequately apply research findings in practice. In addition, physiotherapy technicians and specialists need more training in EBP and its implementation. Therefore, hospitals and healthcare organizations in Saudi Arabia should provide regular workshops to develop their skills in EBP implementation. Cooperation and communication between academic physiotherapists and clinical physiotherapists is recommended to create a better understanding of EBP implementation. Furthermore, lack of funding and resources is the third barrier to EBP use among physiotherapists. Thus, it is important to develop a proper environment in hospitals and universities, especially those which do not provide the required resources for facilitating the use of EBP.
Acknowledgements
We wish to express our sincere thanks to Professor Maureen Dobbins [Scientific Director for the National Collaborating Centre for Methods and Tools (NCCMT) and Professor at School of Nursing, McMaster University, Canada] for her valuable advice as well as her assistance in reviewing our paper. We also take this opportunity to record our sincere thanks to all participants who took part in this study.
References
- 1.Dawes MG. On the need for evidence-based general and family practice. EBM 1996; 1:68–69. [Google Scholar]
- 2.Geddes JR. On the need for evidence-based psychiatry. EBM 1996; 1:199–200. [Google Scholar]
- 3.Richards D, Lawrence A, Sackett DL. Bringing an evidence-base to dentistry. Community Dent Health 1997; 14:63–65. [PubMed] [Google Scholar]
- 4.Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: a guide to best practice. 2nd ed.Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 5.Stetler CB, Brunell M, Giuliano KK, et al. Evidence-based practice and the role of nursing leadership. J Nurs Adm 1998; 28:45–53. [DOI] [PubMed] [Google Scholar]
- 6.Ateef M. Evidence-based learning and practice in physical therapy: a need for novice physical therapists. Saudi J Sports Med 2015; 15:106. [Google Scholar]
- 7.Culham E. Evidence based practice and professional credibility. Physiother Theory Pract 1998; 14:65–67. [Google Scholar]
- 8.Gibbs L, Gambrill E. Evidence-based practice: counterarguments to objections. Res Soc Work Pract 2002; 12:452–476. [Google Scholar]
- 9.Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn’t. BMJ 1996; 312:71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dawes M, Summerskill W, Glasziou P, et al. Sicily statement on evidence-based practice. BMC Med Educ 2005; 5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Booth A. EBLIP five-point-zero: towards a collaborative model of evidence-based practice. Health Info Libr J 2009; 26:341–344. [DOI] [PubMed] [Google Scholar]
- 12.Johnson C. Evidence-based practice in 5 simple steps. J Manipulative Physiol Ther 2008; 31:169–170. [DOI] [PubMed] [Google Scholar]
- 13.Sackett DL, Straus SE, Richardson WS, et al. Evidence based medicine. How to practice and teach EBM. 2nd ed.Edinburgh: Churchill Livingstone; 2000. [Google Scholar]
- 14.Booth A, Brice A. Evidence based practice for information professionals: a handbook. London: Facet Publishing; 2004. [Google Scholar]
- 15.Ciliska D, Thomas H, Buffett C. An introduction to evidence-informed public health and a compendium of critical appraisal tools for public health practice. Canada 2008. Available from: http://www.nccmt.ca/uploads/media/media/0001/01/b331668f85bc6357f262944f0aca38c14c89c5a4.pdf. [Accessed 13 September 2016]. [Google Scholar]
- 16.Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: step by step: the seven steps of evidence-based practice. AJN 2010; 110:51–53. [DOI] [PubMed] [Google Scholar]
- 17.Bury T. Evidence based practice: an overview. WCPT Keynotes 2003. 1–2. [Google Scholar]
- 18.Ministry of Health. Health statistical year book, Saudi Arabia, 2012. Available from: http://www.moh.gov.sa/en/ministry/statistics/book/documents/1433.pdf. [Accessed 21 February 2017]. [Google Scholar]
- 19.Alghadir A, Zafar H, Iqbal ZA, et al. Physical therapy education in Saudi Arabia. J Phys Ther Sci 2015; 27:1621–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Abbad HM, Al-Haidary HM. The perception of physical therapy leaders in Saudi Arabia regarding physical therapy scope of practice in primary health care. J Phys Ther Sci 2016; 28:112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.King Saudi University. Postgraduate programs, College of Applied Medical Sciences. Available from: https://cams.ksu.edu.sa/ar/SanitaryEntitlingSciences/Plan. [Accessed 20 October 2016]. [Google Scholar]
- 22.University of Dammam. Postgraduate programs, College of Applied Medical Sciences. Available from: https://www.uod.edu.sa/ar/colleges/college-of-applied-medical-sciences/programs/masters-of-science-in-physical-therapy-0. [Accessed 20 October 2016]. [Google Scholar]
- 23.Bindawas SM. Physical therapy entry-level education and post-professional training in Saudi Arabia: a comparison of perceptions of physical therapists from five regions. J Phys Ther Sci 2014; 26:1377–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amin TT, Kaliyadan F, Al Qattan EA, et al. Knowledge, attitudes and barriers related to participation of medical students in research in three Arab Universities. Educ Med J 2012; 4:43–56. [Google Scholar]
- 25.Al Mutair. Quality of nursing care in Saudi Arabia: needs for improvement. J Nurs Care 2015;4:309. Available from: http://www.omicsgroup.org/journals/quality-of-nursing-care-in-saudi-arabia-needs-for-improvement-2167-1168-1000309.php?aid=64995. [Accessed 13 September 2016]. [Google Scholar]
- 26.Hanan AA, Roland M. Quality of primary health care in Saudi Arabia: a comprehensive review. Int J Qual Health Care 2005; 17:331–346. [DOI] [PubMed] [Google Scholar]
- 27.Perraton L, Machotka Z, Grimmer K, et al. Embedding evidence-based practice education into a post-graduate physiotherapy program: eight years of pre-post course evaluations. Physiother Res Int 2016. Available from: http://onlinelibrary.wiley.com/doi/10.1002/pri.1659/full. [Accessed 7 October 2016]. [DOI] [PubMed] [Google Scholar]
- 28.Condon C, McGrane N, Mockler D, et al. Ability of physiotherapists to undertake evidence-based practice steps: a scoping review. Physiotherapy 2016; 102:10–19. [DOI] [PubMed] [Google Scholar]
- 29.University of South Australia. Evidence-based practice profile questionnaire. Available from: http://www.biomedcentral.com/content/supplementary/1472-6920-11-100-S1.PDF. [Accessed 29 September 2016]. [Google Scholar]
- 30.Jette DU, Bacon K, Batty C, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther 2003; 83:786–805. [PubMed] [Google Scholar]
- 31.Upton D, Upton P. Knowledge and use of evidence-based practice by allied health and health science professionals in the United Kingdom. J Allied Health 2006; 35:127–133. [PubMed] [Google Scholar]
- 32.Silva TM, Costa L, Costa LO. Evidence-Based Practice: a survey regarding behavior, knowledge, skills, resources, opinions and perceived barriers of Brazilian physical therapists from São Paulo state. Braz J Phys Ther 2015; 19:294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heiwe S, Kajermo KN, Tyni-Lenné R, et al. Evidence-based practice: attitudes, knowledge and behaviour among allied health care professionals. Int J Qual Health Care, 2011. Available from: http://intqhc.oxfordjournals.org/content/early/2011/01/16/intqhc.mzq083.short. [Accessed 18 October 2016]. [DOI] [PubMed] [Google Scholar]
- 34.Iles R, Davidson M. Evidence based practice: a survey of physiotherapists’ current practice. Physiother Res Int 2006; 11:93–103. [DOI] [PubMed] [Google Scholar]
- 35.Ramírez-Vélez R, Correa-Bautista JE, Muñoz-Rodríguez DI, et al. Evidence-based practice: beliefs, attitudes, knowledge, and skills among Colombian physical therapists. Colomb Med 2015; 46:33–40. [PMC free article] [PubMed] [Google Scholar]
- 36.Salbach NM, Jaglal SB, Korner-Bitensky N, et al. Practitioner and organizational barriers to evidence-based practice of physical therapists for people with stroke. Phys Ther 2007; 87:1284–1303. [DOI] [PubMed] [Google Scholar]
- 37.Al-Ansary LA, Khoja TA. The place of evidence-based medicine among primary health care physicians in Riyadh region, Saudi Arabia. Fam Pract 2002; 19:537–542. [DOI] [PubMed] [Google Scholar]
- 38.Khoja TA, Al Ansary LA. Attitudes to evidence-based medicine of primary care physicians in Asia region, Saudi Arabia. East Mediterr Health J 2007; 13:408–419. [PubMed] [Google Scholar]
- 39.Estabrooks CA, Floyd JA, Scott-Findlay S, et al. Individual determinants of research utilization: a systematic review. J Adv Nurs 2003; 43:506–520. [DOI] [PubMed] [Google Scholar]
- 40.Nelson TD, Steele RG. Predictors of practitioner self-reported use of evidence-based practices: practitioner training, clinical setting, and attitudes toward research. Adm Policy Ment Health 2007; 34:319–330. [DOI] [PubMed] [Google Scholar]
- 41.McKenna HP, Ashton S, Keeney S. Barriers to evidence-based practice in primary care. J Adv Nurs 2004; 45:178–189. [DOI] [PubMed] [Google Scholar]
- 42.Brown CE, Wickline MA, Ecoff L, et al. Nursing practice, knowledge, attitudes and perceived barriers to evidence-based practice at an academic medical center. J Adv Nurs 2009; 65:371–381. [DOI] [PubMed] [Google Scholar]
- 43.Majid S, Foo S, Luyt B, et al. Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers (EC). J Med Libr Assoc 2011; 99:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCluskey A. Occupational therapists report a low level of knowledge, skill and involvement in evidence-based practice. Aust Occup Ther J 2003; 50:3–12. [Google Scholar]
- 45.Da Silva TM, Costa C, Garcia AN, et al. What do physical therapists think about evidence-based practice? A systematic review. Man Ther 2015; 20:388–401. [DOI] [PubMed] [Google Scholar]
- 46.Lanyon RI, Goodstein LD. Personality assessment. 3rd ed.New York: Wiley; 1997. [Google Scholar]
- 47.Korb KA. Self-report questionnaires: can they collect accurate information? J Educ Found 2011; 1:5–12. [Google Scholar]
- 48.Gonyea RM. Self-reported data in institutional research: Review and recommendations. New Dir Inst Res 2005; 127:73. [Google Scholar]


