Abstract
Leprosy in children under 15 years of age is a serious public health problem. In this retrospective case series conducted in a Brazilian reference center (2004-2012), we found 18 cases with a mean age of 10.0±3.6 years of age and 16.6% between 0-5 years of age. Almost 56% of the cases were female, with a median time between the first symptoms and diagnosis of 11 months (4-24); 77.8% reported household contact with leprosy patients. Upon hospital admission, 66.7% presented mostly skin symptoms, while 27.8% presented a degree 2 disability. Most were classified as multibacillary (66.7%). Half of the sample developed a reaction (predominantly type 1) during the follow-up period, while 22.2% developed a late disability.
Keywords: Child, Case Studies, Leprosy
Leprosy is an infectious and contagious disease characterized by insidious development, high infectivity, and low pathogenicity, whose human transmission occurs mainly through upper airways.1 The etiological agent (Mycobacterium leprae) presents tropism on the skin and peripheral nerves and, as it multiplies slowly, the incubation period can vary from three to five years.1,2 The later the disease is diagnosed, the greater the risk of developing deformities and disabilities.3
Although it mainly affects young adults, leprosy in children under 15 years of age is a strong indicator of the recent transmission index of still undiagnosed cases, suggesting a high transmissibility and early exposure to bacteria, in turn increasing the chances of secondary disabilities.3 Recognizing the profile of leprosy during childhood is important to finding the proper control strategies for this often neglected disease.
This research was a retrospective case series study, aimed at describing the profile of leprosy in children under 15 years of age at a reference center in the southeastern regions of Brazil. Patients were selected through the Services databank and the sample included all of the cases confirmed between 2004 and 2012. All of the cases suspected in the first consultation were submitted to the protocol, including: bacilloscopy, Mitsuda, skin biopsy, and, as of 2010, a serum dose of phenol glycopeptide-I (PGL-1). The definitions adopted in this study for the classification of the cases, disabilities, and reactions were published in a prior study.2 The data were analyzed by employing descriptive statistics and association tests (t-student, Wilcoxon, and χ2), considered significant if p<0.05.
In the period from 2004 to 2012, 206,837 outpatient appointments (new cases and return patients) were conducted at the Reference Center; of these, 10.8% (22,405) received medical care dedicated to patients with leprosy. In children of under 15 years of age, 18 new cases of leprosy were identified during the period, with an average of 10.0 ± 3.6 years (16.6% from 0-5 years), and 55.6% of the sample, corresponding to the female gender. The median time between the first symptoms and the diagnosis was of 11 months (4-24). Home contact with leprosy was confirmed in 77% of the cases.
Upon hospital admission, 66.7% of the children under 15 years of age presented mostly skin symptoms; 33.3%, of mostly neural symptoms; while 27.8% already presented disabilities (all degree 2). The majority were classified as multibacillary (66.7%). Half of the sample developed a reaction during the follow-up period, while 22.2% developed a later disability. Chart 1 summarizes the other clinical-laboratory characteristics.
Chart 1.
Description of the clinical and laboratory characteristics of 18 patients under 15 years of age diagnosed with leprosy and followed up in a reference center in the southeastern regions of Brazil (2004-2012)
| Case | Main symptoms upon hospital admission | Home contact (yes/no - who) | Bacilloscopy (+) | Mitsuda (mm) | PGL-1* | Sensory- motor test | EMG† | Type of reaction | Treatment of reaction | Type of later disability |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Neural | YES - FATHER and MOTHER | 2+ | 10.5 | NO | Loss of protective sensibility in hands and feet | NR‡ | Type 1 | Corticoid | Loss of protective sensibility in hands and feet |
| 2 | Neural | YES - FATHER and MOTHER | N§ | 4.5 | YES | Loss of protective sensibility in hands and feet | Normal | NA|| | NA | NA |
| 3 | Neural | NO | 4+ | 0.0 | NO | Loss of protective sensibility in hands | Left nail demyelination | Type 1 | Corticoid | Ulnar claw |
| 4 | Skin | NO | N | 10.0 | YES | NR | NR | NA | NA | NA |
| 5 | Neural | YES - FATHER | 1+ | 5.0 | NO | Normal | NR | Type 1 | Corticoid | NA |
| 6 | Neural | YES - FATHER | 1+ | 3.5 | YES | Loss of protective sensibility in hands and feet | Sensory-motor multiple mononeuropathy | Type 1 | Corticoid | Bilateral ulnar claw and bilateral tibial claw |
| 7 | Skin | NO | 1+ | 5.0 | YES | Normal | NR | NA | NA | NA |
| 8 | Skin | YES - FATHER | N | 3.0 | NO | NR | NR | Type 2 | Corticoid | NA |
| 9 | Skin | YES - FATHER | 5+ | 0.0 | YES | Normal | NR | Type 2 | Thalidomide + Corticoid | NA |
| 10 | Skin | NO | 4+ | 0.0 | YES | Normal | NR | Type 1 | Corticoid | NA |
| 11 | Skin | YES - TWO BROTHERS AND GRANDMOTHER | N | 6.0 | YES | Normal | NR | NA | NA | NA |
| 12 | Neural | NO | 3+ | 6.0 | YES | Normal | NR | NA | NA | NA |
| 13 | Skin | NO | N | 10.0 | YES | Normal | NR | Type 1 | Corticoid | Lagophthalmos |
| 14 | Skin | YES - MOTHER | 1+ | 5.0 | NO | NR | Flow change in the right ulnar nerve | Type 1 | Corticoid | NA |
| 15 | Skin | YES -FATHER | N | 0.0 | NO | NR | NR | NA | NA | NA |
| 16 | Skin | YES - MOTHER | N | 5.5 | NO | NR | NR | NA | NA | NA |
| 17 | Skin | NO | N | 0.0 | NO | NR | NR | NA | NA | NA |
| 18 | Skin | NO | N | 5.0 | YES | NR | NR | NA | NA | NA |
Legend:
PGL-1=phenol glycopeptide-I;
EMG=Eletroneuromiography;
NR=Not realized; N
=negative;
NA=Not applicable/Did not present
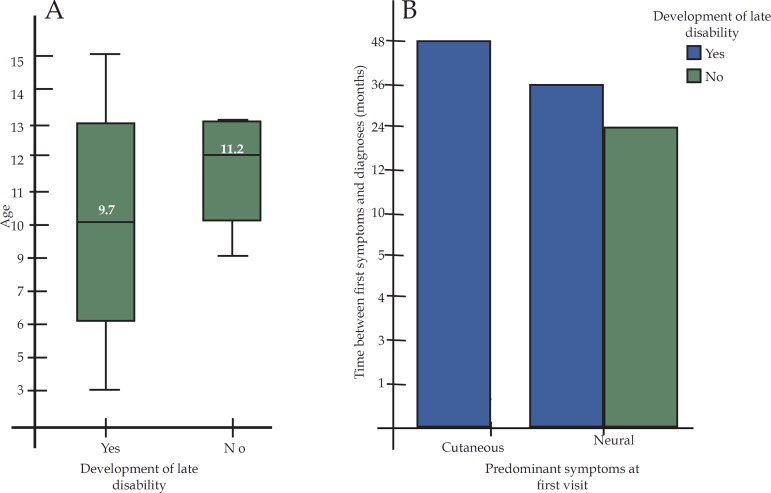
Graph 1A illustrates the age distribution according to the diagnosis of delayed disabilities (Student t, p=0.47). In figure 1B, although the medians of time between the first symptoms and the diagnosis were not different among the patients with predominant initial skin and neural symptoms, the greater proportion of patients with neural symptoms developed a later disability (χ2, p=0.04).
Graph 1.
A. Distribution of age characteristics according to the diagnosis of later disabilities in 18 patients under 15 years of age with leprosy in a reference center located in the southeastern regions of Brazil (2004-2012). B. Distribution of the medians of time between the first symptoms and the diagnosis of leprosy in 188 patients of under 15 years of age according to the type of symptoms most commonly found in the first doctor’s appointment, stratified according to the development of later disabilities.
In the same period analyzed for this study (2004-2012), the number of new cases in children under 15 years of age in Brazil fell from 4,000 new cases/year to a little over 2,300 new cases/year. As a result, the detection coefficient dropped from 7.68 to 4.88.4
The high proportion of disabilities within the diagnosis of these samples, when compared to previous studies, may well be due to the delay in diagnosis and to the tertiary feature of the location of this study. However, one study conducted with secondary data in Rio de Janeiro (2001-2009) also found a high proportion of disabilities within the diagnosis, with a discrete drop in the proportion of disabilities as of 2008.3,5,6,7
Although the majority of cases published in India, China, and Brazil were paucibacillary, the present study found a predominance of multibacillary cases in this sample, which is in accordance with two studies reviewed by Palit & Inamadar.2,3,5,6,7,8
Few studies evaluated the development of reactions in this age range, finding incidences of 1.36% to 29.7%, while 50% of this sample presented reactions, which can also justify the high prevalence of later disabilities found in this study.1,2,8,9 Unsatisfactory results pertaining to the degree of disability in the cure of the disease were also observed by Flach et al., suggesting that there is a significant proportion of patients who do not finish their leprosy treatment within the public health system in Brazil.7
Unlike other prior studies, nearly 80% of the investigated children confirmed home contact with leprosy.2,8,9 In recent years, heavily influenced by the results of the introduction of the Family Health Strategy in the majority of Brazilian municipalities, the averge percentage of home contact cases rose from 45.5% in 2004 to 74.5% in 2012.4
This study does contain limitations inherent to the methodology and profile of the location of the study, which do not, however, render these findings invalid.
The needs for community participation and the engagement of health services in tracking down suspected cases, especially in this vulnerable age range, have proven to be significant in combatting this disease, given that one does not expect children to actively seek out medical care.9 Health education activities in schools appear to be an important tool in the fight against this disease.7
Despite the efforts to reduce the incidence of leprosy in children, data suggest that, unfortunately, the targets will not be soon be met: leprosy still represents a public health problem in many countries, and reports such as this highlight the high prevalence of complications in this age range.1,2,10 Therefore, it is essential that public health policies intensify preventive measures and continue the active search for undiagnosed cases, especially at primary levels of medical care.
Footnotes
Conflict of interest: none.
Work was conducted at the Instituto Lauro de Souza Lima (ILSL) - Bauru (SP), Brazil.
Financial support: none.
REFERENCES
- 1.Oliveira MB, Diniz LM. Leprosy among children under 15 years of age: literature review. An Bras Dermatol. 2016;91:196–203. doi: 10.1590/abd1806-4841.20163661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santos VS, Santos LC, Lôbo LV, Lemos LM, Gurgel RQ, Cuevas LE. Leprosy and disability in children younger than 15 years in an endemic area of northeast Brazil. Pediatr Infect Dis J. 2015;34:e44–e47. doi: 10.1097/INF.0000000000000592. [DOI] [PubMed] [Google Scholar]
- 3.Lana FC, Fabri Ada C, Lopes FN, Carvalho AP, Lanza FM. Deformities due to Leprosy in Children under Fifteen Years Old as an Indicator of Quality of the Leprosy Control Programme in Brazilian Municipalities. J Trop Med. 2013;2013:812793–812793. doi: 10.1155/2013/812793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Portalsaude.saude.gov Brasil. Ministério da Saúde. Indicadores epidemiológicos e operacionais de hanseníase Brasil 2000-2014. [14 Set 2016]. Internet. Disponível em: http://portalsaude.saude.gov.br/images/pdf/2015/outubro/29/S--rie-Hist--rica-Hansen--ase-2000---2014.pdf.
- 5.Yan L, Shen J, Zhou M, Zhang G. Survey on child leprosy patients and problems resulted from the disease in China. Lepr Rev. 2015;86:75–79. [PubMed] [Google Scholar]
- 6.Costa IMC, Patrus OA. Incapacidades físicas em pacientes de hanseníase na faixa de zero a 14 anos, no Distrito Federal, no período de 1979 a 1989. An Bras Dermatol. 1992;67:245–249. [Google Scholar]
- 7.Flach DMAM, Andrade M, Valle CLP, Pimentel MIF, Mello KT. Análise da série histórica do período de 2001 a 2009 dos casos de hanseníase em menores de 15 anos, no estado do RJ. Hansen Int. 2010;35:13–20. [Google Scholar]
- 8.Palit A, Inamadar AC. Childhood leprosy in India over the past two decades. Lepr Rev. 2014;85:93–99. [PubMed] [Google Scholar]
- 9.Sethi M, Rao PS. Challenges in preventing disabilities among children affected by leprosy: findings from a referral hospital in north India. Lepr Rev. 2015;86:296–297. [PubMed] [Google Scholar]
- 10.Alberts CJ, Smith WC, Meima A, Wang L, Richardus JH. Potential effect of the World Health Organization's 2011-2015 global leprosy strategy on the prevalence of grade 2 disability: a trend analysis. Bull World Health Organ. 2011;89:487–495. doi: 10.2471/BLT.10.085662. [DOI] [PMC free article] [PubMed] [Google Scholar]