Summary
Background
Extensive flooding occurred during the winter of 2013–14 in England. Previous studies have shown that flooding affects mental health. Using data from the 2013–14 Public Health England National Study of Flooding and Health, we compared the prevalence of symptoms of depression, anxiety, and post-traumatic stress disorder between participants displaced by flooding and those flooded, but not displaced, 1 year after flooding.
Methods
In this multivariable ordinal regression analysis, we collected data from a cross-sectional survey collected 1 year after the flooding event from flood-affected postcodes in five counties in England. The analysis was restricted to individuals whose homes were flooded (n=622) to analyse displacement due to flooding. The primary outcome measures were depression (measured by the PHQ-2 depression scale) and anxiety (measured by the two-item Generalised Anxiety Disorder [GAD]-2 anxiety scale), and post-traumatic stress disorder (measured by the Post-Traumatic Stress Disorder Checklist [PCL]-6 scale). We adjusted analyses for recorded potential confounders. We also analysed duration of displacement and amount of warning received.
Findings
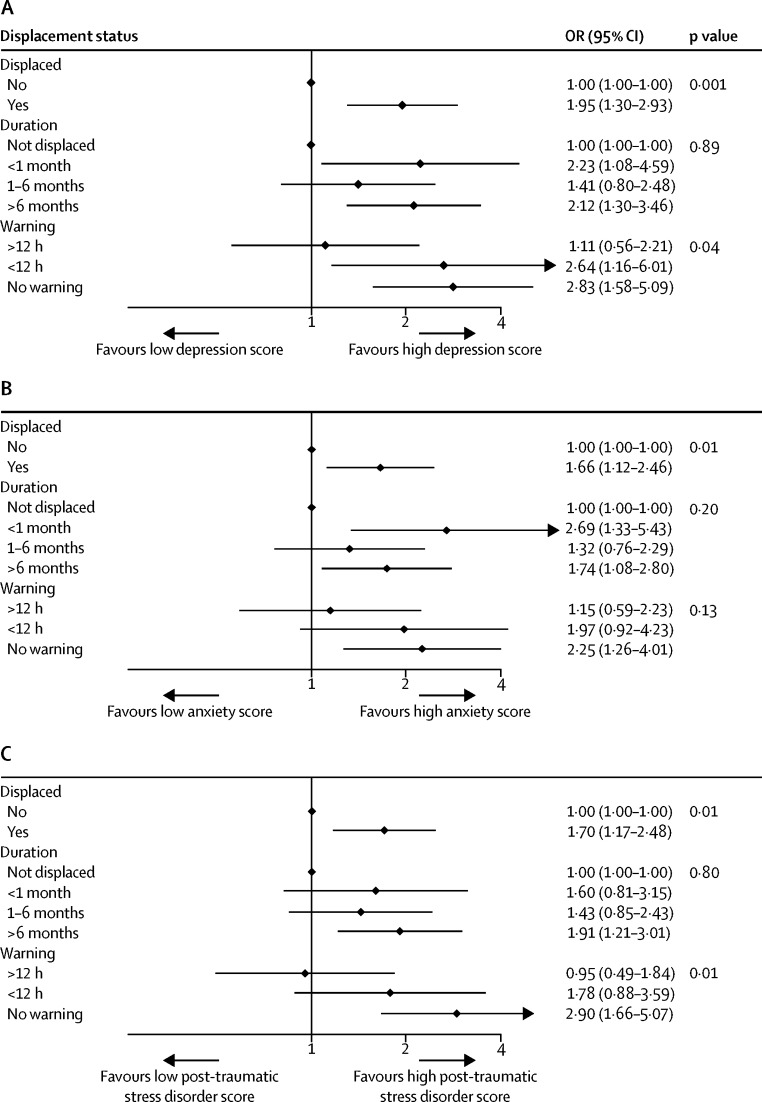
People who were displaced from their homes were significantly more likely to have higher scores on each scale; odds ratio (OR) for depression 1·95 (95% CI 1·30–2·93), for anxiety 1·66 (1·12–2·46), and for post-traumatic stress disorder 1·70 (1·17–2·48) than people who were not displaced. The increased risk of depression was significant even after adjustment for severity of flooding. Scores for depression and post-traumatic stress disorder were higher in people who were displaced and reported receiving no warning than those who had received a warning more than 12 h in advance of flooding (p=0·04 for depression, p=0·01 for post-traumatic stress disorder), although the difference in anxiety scores was not significant.
Interpretation
Displacement after flooding was associated with higher reported symptoms of depression, anxiety, and post-traumatic stress disorder 1 year after flooding. The amount of warning received showed evidence of being protective against symptoms of the three mental illnesses studied, and the severity of flooding might be the reason for some, but not all, of the differences between the groups.
Funding
National Institute for Health Research Health Protection Research Units (HPRU) in Emergency Preparedness and Response at King's College London, Environmental Change and Health at the London School of Hygiene and Tropical Medicine, and Evaluation of Interventions at the University of Bristol, Public Health England.
Introduction
Research suggests that climate change is likely to increase the risk of river, groundwater, and coastal flooding in the UK over the course of this century.1 Natural disasters, including floods, have been linked to increased prevalence of mental disorders such as post-traumatic stress disorder, anxiety, and depression in both industrialised and non-industrialised countries.1, 2, 3, 4, 5 Various risk factors mediate the effect of flooding on mental health and wellbeing. Among these factors, evacuation and displacement have been identified as secondary stressors associated with poorer mental health outcomes.3, 6, 7, 8
Since 2000, there have been eight major flooding events in England, including in the winter of 2015–16. In the winter of 2013–14, there was widespread river, coastal, and surface water flooding after a period of heavy rainfall, which resulted in total economic damages estimated at £1·3 billion. Roughly 25% of the cost was for the repair of damage to an estimated 10 465 residential properties. Most of the residents affected had not previously experienced household flooding. A best estimate of £50 million was spent on temporary accommodation for people who were evacuated or displaced.9
Estimations of future flood risks in the UK show that nearly 2 million properties in flood plains along rivers, estuaries, and coasts are potentially at risk, and river flooding is projected to affect 250 000–400 000 additional people per year by 2080.10
Research in context.
Evidence before this study
We searched PubMed and Embase using the search terms “flood*” and/or “natural disasters” AND “mental health” and/or “post-traumatic stress disorder” and/or “anxiety” and/or “depress*”, and/or “evacuat*” and/or “displace*”, published between Jan 1, 2000 and July 31, 2015. Reference lists of the most relevant studies and literature reviews were also searched for relevant articles. Studies of the effects of natural disasters on mental health in both high-income and low-income countries have found associations between displacement and poor mental health outcomes, including post-traumatic stress disorder, anxiety, depression and reduced wellbeing. The only quantitative studies that have investigated displacement as a primary exposure studied the aftermath of Hurricane Katrina in the USA. Findings from seven studies of people affected showed that severe mental health affects those displaced; however, these studies have limited generalisability to the UK. The most comparable UK survey found an association between evacuation after flooding and increased distress as measured by the General Health Questionnaire-12 (GHQ-12), but not with anxiety, depression, or post-traumatic stress disorder. Investigators of one other UK survey found higher GHQ-12 scores in people who were displaced, but other outcomes were not examined. A qualitative study of people who were displaced for more than 1 year is the only UK study to examine evacuation as a primary exposure. Findings from this study showed high symptoms of anxiety, depression, and post-traumatic stress disorder up to 4 years after flooding.
Added value of this study
We observed a strong association between displacement and symptoms of all three disorders one year after flooding. Among the displaced, those who reported no warning before flooding and displacement were significantly more likely to report more symptoms of depression (p=0·05) and post-traumatic stress disorder (p=0·01), but not anxiety. However, there was no evidence of any association of duration of displacement with these symptoms. Timely (at least 12 h) warning was the only factor associated with reducing the increase in probable mental health disorders seen in people who were subsequently displaced. This is the first quantitative study to examine displacement as a primary exposure after flooding in the UK. As flood events are expected to increase in frequency and severity over the course of this century, these findings contribute to evidence needed to project the likely health impacts of flooding in the UK.
Implications of all the available evidence
These findings suggest that the burden on primary care and mental health services could increase as a consequence of flood related displacement. This burden of increased health needs could affect those areas to which people relocate. Local authorities should consider prioritising identification of people who might have mental health problems after flooding among those displaced. Other priority areas could be early warning systems for evacuation and services to enable flooded residents to remain at home where possible.
In high-income countries such as the UK, flood events usually cause few immediate deaths, and the greatest burden on health is the increase in mental illnesses.11 One study estimated that 80% of all the disability adjusted life-years attributable to floods in the UK were due to mental health.12 A systematic review3 concluded that there is a shortage of research into the mental health effects of fluvial (river) flooding, as opposed to coastal, tsunami, or hurricane-related flooding. This finding is of potential significance in the UK, because fluvial flooding is the most common form of flooding, and many houses are, and continue to be, built on flood plains, whose occupants might have no experience of natural disasters. A previous UK survey of flooded households found a higher prevalence of psychological distress in people who were evacuated compared with those who were able to remain at home, although no significant differences were reported for symptoms of anxiety, depression, or post-traumatic stress disorder.6 Warning time for impending disasters has previously been identified as a key variable in psychological and physical preparation and floods in the UK have been known to progress rapidly and with little warning.13, 14
The National Study of Flooding and Health was established by Public Health England (PHE) and academic partners to investigate the long-term impact of flooding and related disruption on mental health and wellbeing, to help direct preventive and follow-up actions and reduce harm from future flooding. The first finding of the PHE study relates to the cross-sectional data collected in the first year of the survey, 12 months after the period of severe flooding in 2013–14. The main study reported excesses of adverse mental health in flooded compared with unaffected persons, with adjusted odds ratios (ORs) of 5·91 (3·17–10·99) for depression, 6·50 (3·77–11·24) for anxiety, and 7·19 (4·33–11·93) for post-traumatic stress disorder.8 In this Article, we examine the effects of evacuation and displacement due to floods in England on depression, anxiety, and post-traumatic stress disorder indicators. We use a subset of the PHE dataset and only consider people whose homes were flooded to investigate whether evacuation and displacement were associated with poorer mental health than flooding that did not result in evacuation or displacement.
Methods
Study design and participants
In this cross-sectional analysis, we analysed data from the National Study of Flooding and Health, a survey of people living in neighbourhoods affected by flooding during the winter of 2013/14 in the counties of Gloucestershire, Wiltshire, Surrey, Somerset, and Kent in England. A recruitment pack including a questionnaire was sent to each residential address in the postcode areas identified as flooded in January, 2015, 1 year after the event. All adults aged 18 years and older residing at addresses to which recruitment packs were sent were invited to participate, and to return the questionnaire by post or online. Recruitment packs were sent to 8761 households. Details of sampling and data collection methods have been published previously.15
Ethical approval for the study was granted by the Psychiatry, Nursing and Midwifery Research Ethics Subcommittee at King's College London (reference PNM 1314 152). All participants provided written, informed consent to participate in the study, and to the use of their aggregated data for publication in a journal article.
Procedures
The questionnaire contained 36 questions including a bespoke 19-item exposure assessment, based on which respondents were allocated to one of three categories: unaffected, disrupted (eg, by loss of communications, interruption of access or utilities, or flooding of non-liveable rooms) and flooded, defined as floodwater in at least one liveable room in their home. We collected demographic data on sex, date of birth, ethnicity, marital status, household composition and tenure, education, employment, and the presence of any limiting long-term illness. This analysis was restricted to 622 of 2126 respondents who were flooded. The survey included questions on displacement including duration of displacement, whether or not participants were evacuated, and whether a warning was received and when.
We measured outcomes with three validated tools used in clinical practice to screen for symptoms suggestive of probable mental disorders. Each tool is designed to be self-administered. The four-item Patient Health Questionnaire for Depression and Anxiety (PHQ)-4 consists of the two-item PHQ-2 depression scale and the two-item Generalised Anxiety Disorder (GAD)-2 anxiety scale.16, 17 Post-traumatic stress disorder is measured with the four-item Post-Traumatic Stress Disorder Checklist (PCL)-6.18 Each of these scales has a validated cutoff score indicating a probable diagnosis of the condition, the prevalence of which is described for each exposure category.
Statistical analysis
The primary exposure classification was the division between participants who were able to remain at home and those who were evacuated or displaced. Evacuation and displacement were combined in this analysis because reported evacuation was largely concomitant with reported displacement, and to generate sufficient statistical power for the analysis. In the analyses, the term displaced refers to respondents who reported evacuation, displacement, or both.
To investigate the association between mental health and displacement, we ran ordinal (proportional odds) logistic regression analyses on the PHQ-2 (score range 0–6), GAD-2 (score range 0–6), and PCL-6 scores (score range 6–30). The outcome variables can be analysed as dichotomous outcomes creating those with or without a probable diagnosis, as in the previously published main analysis.8 However, in this analysis, ordinal logistic regression was chosen because of its greater statistical power to detect differences in a smaller sample. Because of the large range of post-traumatic stress disorder scores, we grouped the scores into intervals of 5 points, with cutpoints chosen to retain one used for the conventional high dichotomy (eg, 6–8, 9–13, 14–18).
To explore contributory factors, we also created ordered subgroups of duration of displacement (not displaced, <1 month, 1–6 months, >6 months) and amount of warning received (none, <12 h, >12 h). For warning, we calculated ORs for displacement in each warning group compared with the non-displaced participants in the same warning group using an interaction term. We tested for trend over both sets of ORs.
All ORs were adjusted for recorded variables regarded as potential confounders: age group, sex, local authority, previous illness or disability, marital status, education level, housing tenure, employment, and area deprivation score. In a sensitivity analysis, we recalculated standard errors using the Huber-White sandwich estimator, to ensure robustness to clustering in small areas (lower layer super output areas, of which there were 136). We excluded participants who did not complete an outcome questionnaire from analysis of that measure only.
Statistical analyses were done in Stata 14. The core analysis code used for our analysis is in the appendix.
Data sharing
The datasets used and analysed in this study are available from Public Health England Field Epidemiology Service on reasonable request.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Responses to the recruitment packs were received from 2014 (23%) of 8761 unique households. The total number of responses was 2126 (112 houses returned more than one response), of which 622 contributed to this analysis of participants who had flooding in liveable rooms. 366 (59%) of 622 respondents were women, 562 (90%) lived in homes owned by themselves or their family, and 471 (76%) were from the highest two quintiles based on index of multiple-deprivation scores (table 1).
Table 1.
Characteristics of flooded survey population by exposure category
| Flooded, not displaced (n=173) | Flooded and displaced (n=449) | |
|---|---|---|
| Sex | ||
| Male | 74 (43%) | 170 (38%) |
| Female | 90 (52%) | 276 (61%) |
| Age group, years | ||
| 18–35 | 2 (1%) | 37 (8%) |
| 36–64 | 86 (50%) | 252 (56%) |
| 65–79 | 60 (35%) | 119 (27%) |
| 80+ | 14 (8%) | 37 (8%) |
| Marital status | ||
| Single | 12 (7%) | 38 (8%) |
| Married, civil partnership, or cohabiting | 115 (66%) | 316 (70%) |
| Separated or divorced | 18 (10%) | 37 (8%) |
| Other | 20 (12%) | 52 (12%) |
| Housing tenure | ||
| Owner or family-owned | 155 (90%) | 407 (92%) |
| Private rented | 4 (2%) | 19 (4%) |
| Council or housing associated rented | 4 (2%) | 15 (3%) |
| Other | 3 (2%) | 2 (<1%) |
| Employment | ||
| Full-time employed | 55 (32%) | 160 (36%) |
| Part-time employed | 23 (13%) | 72 (16%) |
| Carer | 8 (5%) | 20 (4%) |
| Retired | 5 (3%) | 19 (4%) |
| Other | 72 (42%) | 169 (38%) |
| Education | ||
| Degree or above | 79 (46%) | 151 (34%) |
| Below degree level | 56 (32%) | 188 (42%) |
| Other | 21 (12%) | 43 (10%) |
| No formal qualifications | 10 (6%) | 59 (13%) |
| Pre-existing illness or disability | ||
| Yes | 28 (16%) | 109 (24%) |
| No | 138 (80%) | 335 (75%) |
| English LSOA Quintile (low to high) | ||
| 1 and 2 | 8 (5%) | 8 (2%) |
| 3 | 31 (18%) | 92 (20%) |
| 4 | 64 (37%) | 244 (54%) |
| 5 | 67 (39%) | 96 (21%) |
| Local or district authority | ||
| Sedgmoor | 2 (1%) | 61 (14%) |
| South Somerset | 11 (6%) | 6 (1%) |
| Wiltshire | 8 (5%) | 5 (1%) |
| Gloucestershire | 37 (21%) | 20 (4%) |
| Surrey | 90 (52%) | 294 (65%) |
| Tonbridge and Malling | 25 (14%) | 63 (14%) |
Data are n (%). Not all categories sum to total for the exposure category; missing data ranged from 0·7–5·2% in each of the above categories. These were treated as additional categories in the regression analysis. LSOA=lower layer super output areas.
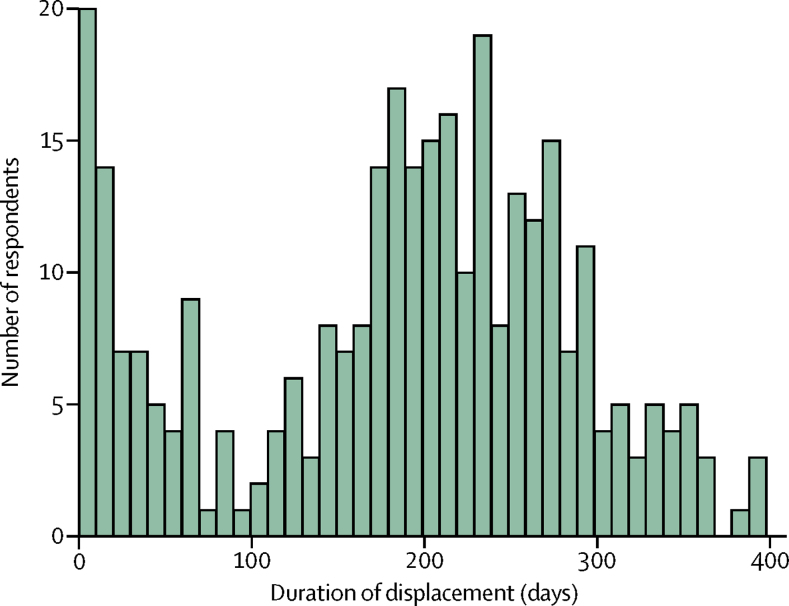
449 (72%) of 622 people whose houses were flooded were also displaced from their homes. Of 449 participants who were flooded and displaced, evacuated, or both, 372 (83%) reported both flooding and displacement, and a further 52 (12%) reported displacement without evacuation. The duration of displacement was calculated based on dates provided by respondents. There were 135 (8%) missing values among respondents who were flooded and displaced, for whom duration of displacement is unknown. There were two peaks of people returning home after displacement (figure 1), and most people were displaced from their homes for 6–9 months.
Figure 1.
Number of days displaced for participants who were flooded and displaced
Crude prevalence of probable depression, anxiety, and post-traumatic stress disorder was higher in participants who were displaced by flooding than in those flooded, but not displaced (table 2). The prevalence of disorders as dichotomous outcomes by displacement status is in table 2. The distribution of depression, anxiety, and post-traumatic stress disorder ordinal scores are in the appendix.
Table 2.
Proportion of participants with probable diagnosis of each outcome
| Participants* | Anxiety (GAD-2 score ≥3) | Depression (PHQ-2 score ≥3) | PTSD (PCL-6 score ≥14) | |
|---|---|---|---|---|
| Exposure group | ||||
| Flooded, not displaced | 164 | 36 (22%) | 28 (17%) | 42 (26%) |
| Flooded and displaced | 441 | 133 (30%) | 97 (22%) | 172 (40%) |
| Duration of displacement | ||||
| <1 month | 41 | 17 (41%) | 10 (25%) | 17 (42%) |
| 1 to 6 months | 86 | 22 (26%) | 13 (16%) | 30 (36%) |
| >6 months | 187 | 56 (30%) | 39 (21%) | 80 (43%) |
| Length of warning | ||||
| No warning | 138 | 50 (36%) | 35 (26%) | 65 (48%) |
| Warning <12 h before flood | 138 | 40 (29%) | 33 (24%) | 49 (37%) |
| Warning >12 h before flood | 156 | 41 (26%) | 28 (18%) | 56 (36%) |
Data are n or n (%). PHQ-2=Patient Health Questionnaire 2 depression scale. GAD-2=Generalised Anxiety Disorder 2 scale. PCL-6=Post-Traumatic Stress Disorder Checklist 6.
Number of participants with non-missing scores for at least one of the outcomes: the actual denominator varied slightly for the three outcomes measured due to missing values; not all exposure measures were completed by participants (duration of displacement and warning received), therefore the number of participants in these categories do not sum to the total flooded and displaced exposure group.
The adjusted ordinal regression analyses of each outcome revealed a similar pattern: people who had been displaced were significantly more likely to report symptoms of depression, anxiety, and post-traumatic stress disorder than people who had not been displaced (figure 2). Among the displaced, the scores for depression and post-traumatic stress disorder were significantly higher when there was no or only short warning than when there was a warning of 12 h or longer (p=0·04 for depression, and p=0·01 for post-traumatic stress disorder from a test for trend; figure 2). Long duration of displacement was not, however, associated with high scores (figure 2). The ORs for people who were displaced for less than 1 month were no lower than those displaced for longer than 6 months (figure 2).
Figure 2.
Adjusted ordinal regression analysis of depression, anxiety, post-traumatic stress disorder by displacement status
(A) Depression assessed by PHQ-2 score. (B) Anxiety assessed by GAD-2 score. (C) Post-traumatic stress disorder assessed by PCL-6 score. ORs are adjusted for age group, sex, local authority, ethnicity, marital status, education level, employment, and deprivation score. OR=odds ratio. PHQ-2=Patient Health Questionnaire 2 depression scale. GAD-2=Generalised Anxiety Disorder 2 scale. PCL-6=Post-Traumatic Stress Disorder Checklist 6. p values for the displaced category are ORs for people who were displaced. For duration and warning, ORs are for tests of trend across the displaced groups.
There was no evidence against proportional odds, which is the key assumption of the ordinal regression model used (appendix). We tested whether the excess prevalence found in people who were displaced by flooding was modified by (or interacted with) any of the measured sociodemographic variables (eg, sex, age, education), and found that one of 27 tests was significant (post-traumatic stress disorder with housing tenure; p=0·04; for details see appendix). In view of the fact that many tests were post-hoc findings, we felt it inappropriate to analyse this further. We also undertook a secondary analysis in which ordinal regression was replaced by standard logistic regression using the conventional cutpoints to define high scores (appendix). Patterns of symptom prevalence were essentially the same as those found with ordinal regression, but the ORs were less precise and in some cases lower. For depression and anxiety the raised odds among people who were displaced compared with those who were not displaced was no longer statistically significant; however, the increase for post-traumatic stress disorder by duration of displacement and the trend in post-traumatic stress disorder and depression by amount of warning remained significant.
The sensitivity analysis was robust to possible geographic clustering of outcome and made little difference (appendix), and unexpectedly reduced the standard errors. Finally, we investigated whether the associations of displacement with adverse mental health symptoms could be explained by displacement being associated with more severe flooding by adjusting additionally for flood depth (three groups: <30 cm, 30–100 cm, and >100 cm), flood duration (four groups: <24 h, 24 to 7 days, 8 days to 2 weeks, >20 weeks), and whether rooms remained unusable at time of the questionnaire, as previously classified.8 With this adjustment, ORs decreased, but remained elevated above those not displaced; OR 1·72 (95% CI 1·12–2·65) for depression, 1·45 (0·96–2·20) for anxiety, and 1·30 (0·86–1·97) for post-traumatic stress disorder (appendix).
Discussion
In this population in England, there was a significant association between displacement as a consequence of flooding and symptoms of depression, anxiety, and post-traumatic stress disorder 1 year after flooding. Among those who were displaced, people who reported having received no warning before flooding and displacement were significantly more likely to report symptoms of depression (p=0·05) and post-traumatic stress disorder (p=0·01), but not anxiety, than those who were warned. However, there was no evidence of any association of duration of displacement with these symptoms. Additionally, the ORs for anxiety and post-traumatic stress disorder were no longer significantly different after adjustment for severity, suggesting that the effect of displacement could partly be explained by the severity of flooding that led to displacement. More complete information on the severity of flooding might help to explain more of the effect, although severity of flooding is not likely to be the only explanation.
Depression and anxiety are common mental disorders that have previously been associated with household flooding.4, 6, 13 In high-income countries, displacement of flooded individuals is usually studied as a secondary stressor.4, 6, 13, 19, 20, 21, 22 The only studies investigating displacement as a primary exposure relate to the aftermath of Hurricane Katrina in the USA because of the exceptionally high (roughly 600 000) number of residents who were displaced for over 1 month.23, 24, 25, 26, 27, 28 The results from these studies are less generalisable to the effects of flooding in the UK because of the substantial differences in the scale, response, and the demographics of the affected population. None of the US studies examined the three mental health outcomes of depression, anxiety, and post-traumatic stress disorder as in this study.
Our findings are not consistent with one of the most directly comparable studies in the UK. In an analysis6 of evacuation as an incident management variable after the 2007 UK floods, being asked to evacuate and evacuating households were associated with higher General Health Questionnaire 12 (GHQ-12) scores, a measure of increased psychological distress, but not with probable depression, anxiety, or post-traumatic stress disorder. However, this analysis was based on a logistic analysis of the outcome variables rather than ordinal regression as used in our study, and the exposure variable of evacuation does not directly compare with our creation of a homogenised displaced, evacuated, or both variable.
The outcomes measured in this survey reflected the mental health outcomes that have been most studies in flooded populations, both in the UK and internationally, but our study has some limitations.1, 2, 6, 7, 20 The ability to compare outcomes between studies is limited by the fact that no established definitions of exposure to flooding for epidemiological studies exist.4
A further limitation is the representativeness of respondents and therefore generalisability of the findings. The characteristics of the population studied distinguish it from similar studies of this type. The areas surveyed in the south of England include some of the most affluent parts of the country and very few participants from the most deprived areas and who were not white. However, data on age, sex, pre-existing illness, deprivation, local authority, ethnicity, marital, education, and employment status were collected as potential confounders, and adjusted for in the analysis.
Also potentially missing from this survey are responses from people displaced for over a year. If similar to the 2007 floods, up to 20% of those displaced in the 2013–14 flood might not have returned home 1 year later.29 However, as there is no register of individuals displaced, this group were not surveyed, which might have caused bias. For example, if long-term displacement is more associated with adverse mental health outcomes, this would underestimate the excess among the displaced because this group might not have been assessed by this survey.
The overall response rate of 23%, although not unusual in these types of surveys, suggests susceptibility to bias. However, we believe that our main conclusions, which are about associations within the sample, are more robust to non-response than comparisons of prevalence with those reported elsewhere. To cause bias in the comparison of mental health outcomes in the displaced and non-displaced would require that non-responders were different to responders for those measures. For example, if people with depression were more likely to respond, that would only cause a bias in the odds ratio of interest if it occurred unequally in the displaced and non-displaced. Also, if people who were displaced were more likely to respond, there would only be bias if the association occurred unequally in people with and without depression. Whether or not the doubly-differential non-response abrogates this assumption is not known, and we acknowledge that this fact adds uncertainty to the results.
Moreover, the findings have only captured point-prevalence at one timepoint, and the act of completing the survey encourages recollection of stressful experiences in respondents, which might lead to overreporting of symptoms. Thus, the overall high prevalence we found could in part reflect overreporting or selective response. However, all participants included in this study had flooding in their homes, so bias in odds ratios of comparisons would only occur if symptom overreporting or selective responding differed between those displaced and not displaced.
We cannot infer from these findings the duration of symptoms after disasters such as flooding, nor whether the total prevalence had peaked at the time the survey was done. The English National Study for Flooding and Health will continue to collect annual outcome data from participants, which will allow future comparisons with our findings over a longer timeperiod than 1 year.
Residual confounding from unmeasured or imperfectly measured risk factors is possible in this study as with all observational studies. We controlled for many potential confounders, but mention some gaps: previous adverse mental health might make displacement more likely and be associated with high outcome scores. We had no information specifically on previous mental health, but did control for pre-existing illness generally, which should have gone some way to minimise bias caused by pre-existing depression. Somewhat similarly, there is potential confounding in this study if past exposure to trauma is independently associated with both displacement and pre-existing symptoms of post-traumatic stress disorder. A study of New York residents affected by Hurricane Sandy in 2012 found that those who had experienced previous trauma related to the attacks on the World Trade Centre were significantly more likely to evacuate and become displaced.30 As noted above, our control for confounding by reported pre-existing illness would have controlled for this to some extent.
In this study, we found that people who were displaced because of flooding had worse mental health outcomes compared with those who remained at home. However, once severity of flooding is adjusted for, we found that only depression in people who were displaced remain statistically significant. Amount of warning received was the only factor studied that showed evidence of being protective in people who were subsequently displaced. These results suggest that local authorities might want to consider that the identification of people with possible mental health problems after flooding should be prioritised among those displaced. The findings from this study also support the case for enhanced early warning systems, and for services to enable residents whose homes are flooded to remain at home.
Displacement due to flooding in the UK is expected to increase over the coming years and these findings contribute to evidence needed to help project the likely health impacts of climate change in the UK. Although we did not study demand for health services, there is indirect evidence that implications of common mental health disorders, such as those we studied, for health services are significant. In the English adult psychiatric morbidity survey, 37·3% of participants with a common mental disorder (as measured by the Clinical Interview Schedule) were receiving treatment for mental illness in 2014.31 Therefore, these findings suggest that the burden on primary care and mental health services could rise as a consequence of flood-related displacement, and that the burden of increased health needs will not only be felt in flooded areas, but also in areas to which people relocate, which can be geographically spread and are not defined by flood risk
In this analysis, we report evidence of an association between flood-related displacement in the UK, especially without warning, and reported symptoms of anxiety, depression, and post-traumatic stress disorder 1 year after flooding. Further research is needed into risk factors for displacement-related poor mental health in high-income country settings, which characteristics determine why some severely flooded residents remain at home while others are displaced, and how the reported symptoms translate into health needs.
Acknowledgments
Acknowledgments
The research was funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response at King's College London in partnership with Public Health England (PHE). RSK and BA's time was funded by the NIHR Health Protection Research Unit in Environmental Change and Health at the London School of Hygiene and Tropical Medicine, London, UK. GJR's time was funded by King's College London NIHR Health Protection Research Unit in Emergency Preparedness and Response, London, UK. We thank respondents to the English National Study for Flooding and Health for providing data analysed used in our study and members of the English National Study for Flooding and Health for supporting this study and providing advice. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, the Department of Health or PHE.
Contributors
AM, RSK, TDW, and BA designed the study. AM, TDW, and GJR did the literature review. TDW collected and processed the data. AM, RSK, and BA analysed the data. AM, RSK, TDW, AB, GJR, and BA interpreted the data. AM, RSK, TDW, AB, GJR, and BA drafted the manuscript and contributed to intellectual content.
National Study of Flooding and Health study group members
Thomas David Waite, Charles R Beck, Angie Bone, Richard Amlôt, R Sari Kovats, Ben Armstrong, Giovanni Leonardi, G James Rubin, and Isabel Oliver.
Declaration of interests
We declare no competing interests.
Contributor Information
Ben Armstrong, Email: ben.armstrong@lshtm.ac.uk.
English National Study of Flooding and Health Study Group:
Thomas David Waite, Charles R Beck, Angie Bone, Richard Amlôt, R Sari Kovats, Ben Armstrong, Giovanni Leonardi, G James Rubin, and Isabel Oliver
Supplementary Material
References
- 1.Hajat S, Ebi KL, Kovats RS, Menne B, Edwards S, Haines A. The human health consequences of flooding in Europe: a review. In: Kirch W, Menne B, Bertollini R, editors. Extreme weather events and public health responses. Springer-Verlag; New York, NY: 2005. pp. 185–197. [Google Scholar]
- 2.Alderman K, Turner LR, Tong S. Floods and human health: a systematic review. Environ Int. 2012;47:37–47. doi: 10.1016/j.envint.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez A, Black J, Jones M. Flooding and mental health: a systematic mapping review. PLoS One. 2015;10:e0119929. doi: 10.1371/journal.pone.0119929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray V CH, Amlôt R, Stanke C, Lock S, Rowlatt H, Williams R. The effects of flooding on mental health. Health Protection Agency; London: 2011. [Google Scholar]
- 5.Uscher-Pines L. Health effects of relocation following disaster: a systematic review of the literature. Disasters. 2009;33:1–22. doi: 10.1111/j.1467-7717.2008.01059.x. [DOI] [PubMed] [Google Scholar]
- 6.Paranjothy S, Gallacher J, Amlot R. Psychosocial impact of the summer 2007 floods in England. BMC Public Health. 2011;11:145. doi: 10.1186/1471-2458-11-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norris FH, Murphy AD, Baker CK, Perilla JL. Post-disaster PTSD over four waves of a panel study of Mexico's 1999 flood. J Trauma Stress. 2004;17:283–292. doi: 10.1023/B:JOTS.0000038476.87634.9b. [DOI] [PubMed] [Google Scholar]
- 8.Waite TD, Chaintarli K, Beck RC. The English National Cohort Study of Flooding and Health: cross-sectional analysis of mental health outcomes at year one. BMC Public Health. 2017;17:129. doi: 10.1186/s12889-016-4000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Environment Agency The costs and impacts of the winter 2013 to 2014 floods. 2015. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/501783/The_costs_and_impacts_of_the_winter_2013_to_2014_floods_-_summary.pdf (accessed June 12, 2017).
- 10.Foresight, Government Office for Science . Future flooding: mid-term review. Foresight project: flood and coastal defence. Government Office for Science; London: 2011. [Google Scholar]
- 11.Menne B, Murray V. Floods in the WHO European region: health effects and their prevention. World Health Organisation, Public Health England; Geneva, London: 2013. http://www.euro.who.int/__data/assets/pdf_file/0020/189020/e96853.pdf (accessed June 12, 2017). [Google Scholar]
- 12.Fewtrell L, Kay D. An attempt to quantify the health impacts of flooding in the UK using an urban case study. Public Health. 2008;122:446–451. doi: 10.1016/j.puhe.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Penning-Rowsell E, Tapsell S, Wilson T. Key policy implications of the health effects of floods. In: Kirch W, Bertollini R, Menne B, editors. Extreme weather events and public health responses. Springer Berlin Heidelberg; Berlin, Heidelberg: 2005. pp. 207–223. [Google Scholar]
- 14.Pitt M. The Pitt Review: learning lessons from the 2007 floods. London: UK, 2008.
- 15.Du W, FitzGerald GJ, Clark M, Hou XY. Health impacts of floods. Prehosp Disaster Med. 2010;25:265–272. doi: 10.1017/s1049023x00008141. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 17.Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43:585–594. doi: 10.1016/j.brat.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer R, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 19.Mason V, Andrews H, Upton D. The psychological impact of exposure to floods. Psychol Health Med. 2010;15:61–73. doi: 10.1080/13548500903483478. [DOI] [PubMed] [Google Scholar]
- 20.Reacher M, McKenzie K, Lane C. Health impacts of flooding in Lewes: a comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Commun Dis Public Health. 2004;7:39–46. [PubMed] [Google Scholar]
- 21.Tunstall S, Tapsell S, Green C, Floyd P, George C. The health effects of flooding: social research results from England and Wales. J Water Health. 2006;4:365–380. doi: 10.2166/wh.2006.031. [DOI] [PubMed] [Google Scholar]
- 22.Hoffpauir SA, Woodruff LA. Effective mental health response to catastrophic events: lessons learned from Hurricane Katrina. Fam Community Health. 2008;31:17–22. doi: 10.1097/01.FCH.0000304064.02454.e8. [DOI] [PubMed] [Google Scholar]
- 23.Fussell E, Lowe SR. The impact of housing displacement on the mental health of low-income parents after Hurricane Katrina. Soc Sci Med. 2014;113:137–144. doi: 10.1016/j.socscimed.2014.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LaJoie AS, Sprang G, McKinney WP. Long-term effects of Hurricane Katrina on the psychological well-being of evacuees. Disasters. 2010;34:1031–1044. doi: 10.1111/j.1467-7717.2010.01181.x. [DOI] [PubMed] [Google Scholar]
- 25.Merdjanoff AA. There's no place like home: Examining the emotional consequences of Hurricane Katrina on the displaced residents of New Orleans. Soc Sci Res. 2013;42:1222–1235. doi: 10.1016/j.ssresearch.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Kloos B, Flory K, Hankin BL, Cheely CA, Segal M. Investigating the roles of neighborhood environments and housing-based social support in the relocation of persons made homeless by hurricane Katrina. J Prev Interv Community. 2009;37:143–154. doi: 10.1080/10852350902735742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Legerski JP, Vernberg EM, Noland BJ. A qualitative analysis of barriers, challenges, and successes in meeting the needs of Hurricane Katrina evacuee families. Community Ment Health J. 2012;48:729–740. doi: 10.1007/s10597-011-9446-1. [DOI] [PubMed] [Google Scholar]
- 28.Tucker P, Jeon-Slaughter H, Pfefferbaum B, Khan Q, Davis NJ. Emotional and biological stress measures in Katrina survivors relocated to Oklahoma. Am J Disaster Med. 2010;5:113–125. doi: 10.5055/ajdm.2010.0013. [DOI] [PubMed] [Google Scholar]
- 29.Milojevic A, Kovats S, Leonardi G, Murray V, Nye M, Wilkinson P. Population displacement after the 2007 floods in Kingston upon Hull, England. J Flood Risk Manag. 2014;9:99–104. [Google Scholar]
- 30.Gargano L, Caramanica K, Sisco S, Brackbill R, Stellman S. Exposure to the World Trade Center disaster and 9/11-related post-traumatic stress disorder and household disaster preparedness. Disaster Med Public Health Prep. 2015;9:625–633. doi: 10.1017/dmp.2015.71. [DOI] [PubMed] [Google Scholar]
- 31.Lubian K, Weich S, Stansfeld S. Adult Psychiatric Morbidity Survey: survey of mental health and wellbeing, England, 2014, Chapter 3: mental health treatment and service use. 2014. http://content.digital.nhs.uk/catalogue/PUB21748/apms-2014-treatment.pdf (accessed June 12, 2017).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.