Overview
In the spirit of Dr. Haggerty’s teachings, we present an overview of our work to improve care for children with asthma in the context of 3 lessons learned:1 1) The importance of providing integrated services across disciplinary boundaries for children with chronic illness, 2) The need to move from a care model focused only on the individual child to a model focused on the child, family, and community, and 3) The need to expand beyond the local community and take a broad perspective on improving health on a national level. The goal of our program is to develop sustainable models to overcome the multiple obstacles to effective preventive care for urban children with asthma. The primary intervention for our original School Based Asthma Therapy (SBAT) program was directly observed administration of preventive asthma medications in school (with dose adjustments based on NHLBI guidelines).2 We found that children who received preventive medications in school through directly observed therapy had improved outcomes across multiple outcome measures.3 Our subsequent asthma programs have focused on dissemination and sustainability, with the incorporation of communication technology to enhance the system of care. We are currently testing the ‘School-Based Telemedicine Enhanced Asthma Management’ (SB-TEAM) program, including 400 children with persistent asthma from the Rochester City School District. This program includes directly observed administration of preventive asthma medication at school, and school-based telemedicine to assure appropriate evaluation, preventive medication prescription, and follow-up care. It is designed to implement and sustain guideline-based asthma care through existing community infrastructure, and could serve as a model for the integration of services in both rural and urban communities.
Introduction
Asthma is one of the most common chronic diseases of childhood, affecting 1 in 11 children in the US.4 Children of minority racial or ethnic backgrounds and children living in poverty suffer a disproportionate burden from the disease,5 with prevalence rates higher than 16% among Puerto Rican and non-Hispanic black children.6 Asthma accounts for numerous office and emergency room visits and hospitalizations as well as substantial health care cost.7 Importantly, the burden of asthma extends beyond morbidity from ongoing symptoms and exacerbations. Asthma is also the leading cause of missed school days in children8 and contributes to limitations in activity,9–11 missed work days for caregivers,12 and caregiver stress and depression.13–15
National guidelines for the management of asthma recommend effective daily preventive anti-inflammatory medications for all children with persistent asthma symptoms.16 Implementation of these guidelines, however, has been problematic. Many children in the US with persistent asthma symptoms do not receive effective preventive medications.17–19 In one multistate study, more than 1/3 of children with persistent asthma symptoms reported no use of preventive medication.20 In addition, even among children who are prescribed a preventive medication, many do not achieve optimal control.20 Consistent with other studies that have shown adherence rates to preventive medications of approximately 50%, we have found that adherence to daily medications is very low21 and appropriate follow-up occurs infrequently.22 Further, parents tend to underestimate the child’s overall disease severity23 causing communication barriers with providers and inadequate attention to asthma care.21 Importantly, poor children living in the inner-city are at greatest risk for under-use of preventive medications and lack of appropriate asthma care.24,25 Thus a significant amount of asthma morbidity could be prevented by improvements in the delivery of care.
Rochester School-Based Asthma Studies
School-based programs represent a promising strategy for asthma management because of the potential to reach large numbers of children in a community setting, where they regularly spend much of their day.2 Over more than a decade, we have had the privilege of working in partnership with the entire Rochester city school district in Rochester, NY to implement novel programs for urban, high risk children with asthma. The Rochester city school district serves approximately 17,000 elementary school students, the majority of whom identify as either African American (57%) or Hispanic (28%). More than 80% of the students live in poverty, and around 1 in 6 students have asthma.
Our initial studies tested directly observed administration of preventive asthma medications in school to improve outcomes for children with persistent asthma.3,26 By delivering daily preventive medications through schools, adherence can be assured on the days the child attends school, and most schools are already equipped to provide daily medications for other conditions such as attention deficit disorder. Thus the delivery of daily preventive asthma medications at school represents a conceptually simple and inexpensive system intervention to improve adherence. In one study including 530 children (ages 3–10 years) from more than 50 elementary schools,2,3 results demonstrated reduced morbidity, absenteeism, and exacerbations for children receiving DOT. We also found that the program was cost-effective in reducing asthma symptoms compared to other existing programs, with a cost of $10 per symptom-free day.12
Although caregivers, providers, and the school health team (nurses and health aides) have been very supportive of this work, several aspects of the original SBAT program limit its sustainability and potential for dissemination. In particular, in SBAT all initial and follow-up assessment data were obtained by the study team through in-home and telephone contacts with families, and recommendations for initial medications as well as adjustments in therapy were communicated to the child’s primary care provider (PCP). The PCP was asked to approve recommendations for preventive therapy so that they could be implemented by the study team. This made the initiation and tailoring of therapy burdensome due to difficulty communicating back and forth to primary care offices and lack of direct contact between the PCP and caregiver, and often resulted in delays in medication administration. With this key limitation in mind, we developed the SB-TEAM program as a new model of care within the school system, using telemedicine assessments to facilitate these steps in a potentially cost-effective and easily disseminable manner.
SB-TEAM Study
Theoretical Framework
Our school based interventions are based on the Chronic Care Model (CCM).27 This model is currently being implemented in a number of health care systems as an organizing framework for collaborative quality-improvement efforts that involve changes to the system of care for chronic disease. The goal of the model is to ensure access to services that are proven to improve outcomes.
The CCM components built into the SB-TEAM intervention include delivery system change (guideline-based preventive asthma medications delivered through school), decision support (telemedicine assessments with feedback to the PCP and family about the child’s symptoms and implementation of guideline-based care), and community resources (school-based care, pharmacy support). These components allow for coordination of care among parents, schools, and providers. Objectives are to improve communication, access to care, adherence to medications, and satisfaction with care. Ultimate goals are to improve clinical and functional outcomes and reduce costs. Importantly, in all of our school-based programs, the medical home remains unchanged and the PCP is informed of every step of the child’s asthma care.
Telemedicine Intervention
Telemedicine is a system that allows clinicians to provide assessment and consultation through remote audiovisual technology and enables children to be seen by a physician without making a trip to the doctor’s office or hospital.28,29 This rapidly expanding technology eliminates a significant barrier to care by making it possible for a healthcare visit to be accomplished while the child remains at school, the parent remains at work and the provider remains at their usual work place (or home). Telemedicine can be used to care for a large proportion of acute illness episodes that arise in children (e.g.; rashes, sore throats, colds, ear pain, pinkeye)30 as well as to monitor and address chronic conditions such as attention deficit disorder and asthma.31 Telemedicine is used in cities worldwide31 and has been used in Rochester, NY for more than 10 years,32 now serving all schools in the city school district with mobile telemedicine units and having performed >14,000 visits. Additionally, there is reimbursement for telemedicine visits by local payers, making it a sustainable system of care. Telemedicine is an efficient, cost-effective, and safe way of reaching patients and facilitating access to care.30,33–35
To overcome barriers to guideline-based preventive asthma care among minority, poor children residing in urban Rochester, NY, the School-Based Telemedicine Enhanced Asthma Management (SB-TEAM) program utilizes both: 1) school-based directly observed therapy with preventive asthma medications; and 2) telemedicine visits to overcome key barriers to guideline-based preventive asthma care.
Initial Telemedicine Assessment
Children enrolled in the SB-TEAM group are scheduled for a telemedicine visit in the school health office at the start of the school year to provide an initial assessment and to determine the initial medication to be used for directly observed therapy. Most children receive once daily dosing of their preventive medication because it is effective36 and allows for administration of medication during school hours. If more frequent dosing is needed, the additional dose is given at home. While many schools do not have a full-time nurse, all schools are prepared for medication administration as many children have daily medication needs (e.g. medications for attention deficit disorder). In our prior study, controller medications were administered >95% of the time the child was in school. While adherence is assured by the nurse on the days the child attends school, adherence is simply encouraged on days the child does not attend school.
The school site component of the telemedicine visit is completed by clinical telemedicine assistants (CTAs) who already work in the school district. The CTA brings the mobile telemedicine unit and meets with the child at school, typically in the school health office. The CTA obtains clinical history and physical examination data (including medical images, height/weight, and breath sounds), which are either securely stored in the telemedicine system’s “virtual waiting room”, or assessed by the PCP in real time, using videoconferencing to link the child and PCP. Using the scheduling system pre-established by the telemedicine program and coordinated with the medical practices that provide telemedicine visits, a provider is notified that a child’s visit is available. The visit is scheduled with the PCP in real time or performed within 48 hours using a ‘store-and-forward’ approach to information exchange. The PCP logs into the telemedicine system from their office or home, reviews the recorded symptom information, views the child’s images, and listens to the breath sounds. The PCP then completes the assessment and communicates with the child’s caregiver via videoconference or telephone to further discuss the child’s asthma and develop a treatment plan. The telemedicine provider delivers brief asthma education and referrals to community resources as needed, and sends a guideline-based preventive medication prescription electronically to a local pharmacy. The telemedicine assessment at school approximates care that would be delivered at an outpatient asthma visit and uses a standard asthma visit template. Reimbursement is submitted to the child’s health insurance.
Follow-Up Telemedicine Asthma Control Assessments
Follow-up telemedicine assessments occur twice during the study period. They are scheduled at school 4–6 weeks after initiating DOT, and again 4–6 weeks later. These visits focus on assessment of control, assessment of ongoing triggers or co-morbid conditions that might interfere with an optimal response to treatment, and brief asthma education. Guideline-based medication adjustments (or specialist referral, if warranted) are recommended for children who continue to have persistent symptoms despite DOT in school.
Outcome Assessment
We are testing this program in a randomized trial of the School-Based Telemedicine Enhanced Asthma Management (SB-TEAM) intervention versus an enhanced usual care (eUC) comparison group with 400 inner-city children with persistent asthma. The intervention continues until the end of the school year, which varies from 7–9 months depending on the timing of enrollment for each child. The preliminary effectiveness of the study is being assessed by blinded telephone interviews with the caregivers, medical record review, and review of school records. The primary outcome is symptom-free days over 2 weeks. Caregivers are asked to report the number of days their child experienced no symptoms of asthma (defined as a 24 hour period with no coughing, wheezing, chest tightness, or shortness of breath, and no need for rescue medications) over the prior 2 weeks. Figure 1 shows a summary of the SB-TEAM study design.
Figure 1. Summary of Study Design.
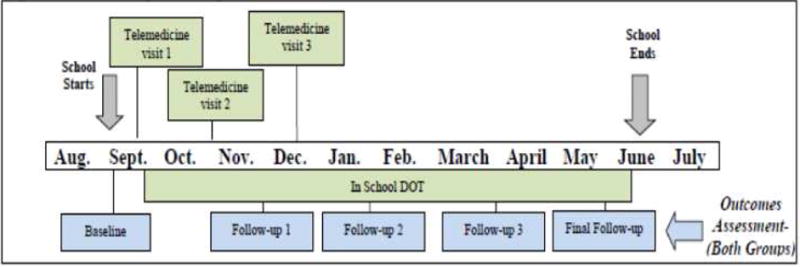
Figure 1 outlines the process of events for the SB-TEAM study. Children are identified through telephone screening at the start of the school year and a home visit is scheduled for the baseline assessment. Children assigned to the SB-TEAM group are then scheduled for an initial telemedicine visit to determine the appropriate treatment to be initiated as DOT at school. The subsequent 2 telemedicine visits are used to reassess symptoms and determine whether a step-up in therapy is needed. Any changes in treatment are implemented through school-based DOT. Both groups are followed over time by blinded interviewers, assessing a variety of outcomes until the end of the school year.
Summary and Lessons Learned
We have found that school-based care can substantially improve outcomes for urban children with asthma, and are now collaborating with more than 70 schools and preschools in the Rochester area as well as 13 primary care practices. We have enrolled, in total, more than 1,900 children in our programs. Our new SB-TEAM program focuses on an integrated system of preventive medication delivery and telemedicine assessment in schools. For the children in the SB-TEAM group, medication adherence is assured through directly observed therapy on the days in which the child attends school. The telemedicine assessments ensure access to the follow-up care recommended by the Expert Panel guidelines, and occur systematically and efficiently. Integration within the schools enhances the potential for program sustainability. Health plan reimbursement for telemedicine visits, an essential step towards sustainability, has also been achieved. Collaboration with schools allows high-risk children to be reached in the setting in which they spend much of their day. The key processes of telemedicine assessment and delivery of medications to the schools are facilitated through technology that is transferable into other systems and communities.
In addition to our work in Rochester, we have now consulted with several programs across the country that are in the process of implementing school-based preventive asthma treatment. Many of these sites are using specific resources available in their own local communities, such as school-based health clinics located on-site, and the Breath-mobile program which goes directly to schools, to facilitate asthma assessments and implementation of supervised medication delivery through schools. In fact, some programs are receiving financial support through local accountable care organizations.37 Thus, even without full-time health personnel in schools, the provision of daily asthma preventive medications in school is viewed as a relatively simple and sustainable system change to improve medication adherence.
Conclusion
In reflecting on Dr. Haggerty’s ‘lessons learned’, we come back to the need for integrated services for children with chronic illnesses. This work involves an interdisciplinary team of primary care providers, school nurses, medical assistants, and school administrative staff, all of whom serve a critical role in delivering optimal care to children. We recognize the power of moving from office-based care to care in the community (and specifically in schools), which allows us to enhance our reach to children, broaden the impact of our work, and gain trust from families and key stakeholders as we establish partnership outside academia, outside the medical center and outside the office. The daily involvement of school health personnel for chronic illness management not only can enhance medication adherence, but also allows for ongoing monitoring of symptoms, promotion of self-management and proper medication technique, and relationship building that can have ongoing positive effects on the child’s wellbeing. Lastly, we are optimistic about the power of community based work to make a difference for children broadly. We recognize that identifying key local resources, and incorporating technology into our programs, can help with national dissemination efforts. We are grateful for Dr. Haggerty and his colleagues for their leadership in extending the focus of academic medicine to the community and to those children and families who should be better served. We would like to consider our work towards improving preventive asthma care to be an extension of his. Our ultimate goal is to disseminate efficient models of chronic illness care through schools, ensure access to effective preventive treatments, and improve outcomes for underserved children across communities.
Acknowledgments
We thank Andrew MacGowan, MS, Flora McEntee, RN, Erin Graupman, MBA, BSN, RN, the Rochester City School District and their nurses for their ongoing partnership and support of our work. We thank the SB-TEAM study team for their limitless energy to help children with asthma, and the children, families, and primary care providers who participated in these studies. This work was funded by a grant from the National Heart, Lung and Blood Institute of the National Institutes of Health (R01 HL079954).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kendig JW. Robert J Haggerty, MD: Oral History Project. Elk Grove Village, IL: American Academy of Pediatrics: Pediatric History Center; 2003. [Google Scholar]
- 2.Halterman JS, Borrelli B, Fisher S, Szilagyi P, Yoos L. Improving care for urban children with asthma: design and methods of the School-Based Asthma Therapy (SBAT) trial. J Asthma. 2008;45(4):279–286. doi: 10.1080/02770900701854908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halterman J, Szilagyi P, Fisher S, et al. A randomized controlled trial to improve care for urban children with asthma: results of the School-Based Asthma Therapy trial. Archives of Pediatrics & Adolescent Medicine. 2011;165:262–268. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinbami LJ, Moorman JE, Bailey C, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS data brief. 2012;(94):1–8. [PubMed] [Google Scholar]
- 5.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. Journal of Allergy and Clinical Immunology. 2014;134(3):547–553. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health NCfE. National Asthma Prevalence (2014) 2016 https://www.cdc.gov/asthma/most_recent_data.htm. Accessed November, 2016.
- 7.Akinbami LJ, Sullivan SD, Campbell JD, et al. Asthma outcomes: healthcare utilization and costs. J Allergy Clin Immunol. 2012;129(3 Suppl):S49–64. doi: 10.1016/j.jaci.2011.12.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moonie SA, Sterling DA, Figgs L, Castro M. Asthma status and severity affects missed school days. J Sch Health. 2006;76(1):18–24. doi: 10.1111/j.1746-1561.2006.00062.x. [DOI] [PubMed] [Google Scholar]
- 9.Walker TJ, Reznik M. In-school asthma management and physical activity: children’s perspectives. J Asthma. 2014;51(8):808–813. doi: 10.3109/02770903.2014.920875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glazebrook C, McPherson AC, Macdonald IA, et al. Asthma as a barrier to children’s physical activity: implications for body mass index and mental health. Pediatrics. 2006;118(6):2443–2449. doi: 10.1542/peds.2006-1846. [DOI] [PubMed] [Google Scholar]
- 11.Lang DM, Butz AM, Duggan AK, Serwint JR. Physical activity in urban school-aged children with asthma. Pediatrics. 2004;113(4):e341–346. doi: 10.1542/peds.113.4.e341. [DOI] [PubMed] [Google Scholar]
- 12.Noyes K, Bajorska A, Fisher S, Sauer J, Fagnano M, Halterman JS. Cost-effectiveness of the School-Based Asthma Therapy (SBAT) program. Pediatrics. 2013;131(3):e709–717. doi: 10.1542/peds.2012-1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- 14.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104(6):1274–1280. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- 15.Silver EJ, Warman KL, Stein RE. The relationship of caretaker anxiety to children’s asthma morbidity and acute care utilization. J Asthma. 2005;42(5):379–383. doi: 10.1081/JAS-62999. [DOI] [PubMed] [Google Scholar]
- 16.National Asthma Education and Prevention Program (NAEPP) Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 17.Halterman JS, Aligne CA, Auinger P, McBride JT, Szilagyi PG. Inadequate therapy for asthma among children in the United States. Pediatrics. 2000;105(1 Pt 3):272–276. [PubMed] [Google Scholar]
- 18.Bauman LJ, Wright E, Leickly FE, et al. Relationship of adherence to pediatric asthma morbidity among inner-city children. Pediatrics. 2002;110(1 Pt 1):e6. doi: 10.1542/peds.110.1.e6. [DOI] [PubMed] [Google Scholar]
- 19.Desai M, Oppenheimer JJ. Medication adherence in the asthmatic child and adolescent. Current allergy and asthma reports. 2011;11(6):454–464. doi: 10.1007/s11882-011-0227-2. [DOI] [PubMed] [Google Scholar]
- 20.Halterman JS, Auinger P, Conn KM, Lynch K, Yoos HL, Szilagyi PG. Inadequate therapy and poor symptom control among children with asthma: findings from a multistate sample. Ambul Pediatr. 2007;7(2):153–159. doi: 10.1016/j.ambp.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Halterman JS, Yoos HL, Kaczorowski JM, et al. Providers underestimate symptom severity among urban children with asthma. Arch Pediatr Adolesc Med. 2002;156(2):141–146. doi: 10.1001/archpedi.156.2.141. [DOI] [PubMed] [Google Scholar]
- 22.Halterman JS, Yoos HL, Sidora K, Kitzman H, McMullen A. Medication use and health care contacts among symptomatic children with asthma. Ambul Pediatr. 2001;1(5):275–279. doi: 10.1367/1539-4409(2001)001<0275:muahcc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 23.Yoos HL, Kitzman H, McMullen A, Sidora K. Symptom perception in childhood asthma: how accurate are children and their parents? J Asthma. 2003;40(1):27–39. doi: 10.1081/jas-120017204. [DOI] [PubMed] [Google Scholar]
- 24.Akinbami LJ, LaFleur BJ, Schoendorf KC. Racial and income disparities in childhood asthma in the United States. Ambul Pediatr. 2002;2(5):382–387. doi: 10.1367/1539-4409(2002)002<0382:raidic>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Piecoro LT, Potoski M, Talbert JC, Doherty DE. Asthma prevalence, cost, and adherence with expert guidelines on the utilization of health care services and costs in a state Medicaid population. Health Serv Res. 2001;36(2):357–371. [PMC free article] [PubMed] [Google Scholar]
- 26.Halterman J, Riekert K, Bayer A, et al. A pilot study to enhance preventive asthma care among urban adolescents with asthma. Journal of Asthma. 2011;48(5):523–530. doi: 10.3109/02770903.2011.576741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 28.Miller E. Solving the disjuncture between research and practice: telehealth trends in the 21st century. Health Policy. 2007;82:133–141. doi: 10.1016/j.healthpol.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 29.McConnochie K. Potential of telemedicine in pediatric primary care. Pediatrics in Review. 2006;27(9):e58–e65. doi: 10.1542/pir.27-9-e58. [DOI] [PubMed] [Google Scholar]
- 30.McConnochie KM, Wood NE, Alarie C, Ronis S. Care Offered by an Information-Rich Pediatric Acute Illness Connected Care Model. Telemed J E Health. 2016;22(6):465–472. doi: 10.1089/tmj.2015.0161. [DOI] [PubMed] [Google Scholar]
- 31.McLean S, Chandler D, Nurmatov U, et al. Telehealthcare for asthma: a cochrane review. Cmaj. 2011;183(11):E733–E742. doi: 10.1503/cmaj.101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McConnochie K, Wood N, Kitzman H, et al. Telemedicine Reduces Absence Resulting From Illness in Urban Child Care: Evaluation of an Innovation. Pediatrics. 2005;115(5):1273 –1282. doi: 10.1542/peds.2004-0335. [DOI] [PubMed] [Google Scholar]
- 33.McConnochie K, Wood NE, Herendeen NE, et al. Acute illness care patterns change with use of telemedicine. Pediatrics. 2009;123:e989–e995. doi: 10.1542/peds.2008-2698. [DOI] [PubMed] [Google Scholar]
- 34.McConnochie KM, Tan J, Wood NE, et al. Acute illness utilization patterns before and after telemedicine in childcare for inner-city children: A cohort study. Telemedicine and e-Health. 2007;13:381–390. doi: 10.1089/tmj.2006.0070. [DOI] [PubMed] [Google Scholar]
- 35.McConnochie KM, Feng Qian J, Noyes K, Wood NE, Roghmann KJ. Potential to Reduce Healthcare Costs by Replacing Emergency Department with Telemedicine Visits. Paper presented at: Pediatric Academic Societies’ Annual Meeting; 2008; Honolulu. [Google Scholar]
- 36.LaForce CF, Pearlman DS, Ruff ME, et al. Efficacy and safety of dry powder fluticasone propionate in children with persistent asthma. Ann Allergy Asthma Immunol. 2000;85(5):407–415. doi: 10.1016/S1081-1206(10)62556-2. [DOI] [PubMed] [Google Scholar]
- 37.http://www.nationwidechildrens.org/asthma-therapy-program. Accessed 2/28/17.


