Abstract
Background
After a single slip, older adults rapidly make adaptive changes to avoid or eliminate further backward loss of balance or a fall. This rapid adaptation has been termed the “single trial effect”. The purpose of this study was to explore the relationship between the motor errors subjects experienced upon a novel slip and the selection and execution of corrective response by which they modified their ongoing gait pattern and turned it into a protective step.
Methods
A forward slip was induced in the laboratory among 145 community-living older (≥65 year old) adults who were protected by an overhead full body harness system. An eight-camera motion analysis system recorded subjects’ kinematics, which was used to compute their instability (motor error), recovery step placement (response selection), and stability gain (motor correction).
Findings
A linear relationship was found between the stability errors at recovery foot liftoff and the distance between the recovery foot and slipping foot at the time of its touchdown, reflecting an appropriate selection of response that was proportionate to the motor error. A linear relationship was also found between this step modification and resulting stability gain, indicating that greater step modification resulted in greater stability gain. This learning behavior was surprisingly consistent regardless whether the outcome was a recovery or a fall.
Interpretations
These results suggest that fallers and non-fallers all have an intact motor learning foundation that has enabled them to rapidly improve their stability in subsequent exposures.
Keywords: Perturbation, Motor learning, Stability, Protective stepping
1. Introduction
Falling is a common cause of hip fracture, traumatic head injury, and a major cause of death in older adults (Hayes et al., 1996; Morley, 2002). Further, 40% of falls among community-living adults is slip-related backward falls. These backward falls are particularly dangerous because they frequently cause hip fractures (Luukinen et al., 2000; Nevitt et al., 1993). Interventions (including strength training, dance mat or step pad exercises, and tai chi) aimed at increasing one’s strength, balance, and proactive control against postural disturbances have been shown effective to reduced fall risk in older adults (Lord et al., 1995; Schoene et al., 2011; Schoene et al., 2013; Wolf et al., 1996). Slip perturbation training (Pai et al., 2014; Parijat and Lockhart, 2012) has emerged as an alternative approach to conventional fall-reduction approaches by harnessing and improving a person’s natural responses to externally induced perturbations. Such processes are akin to the “learning from falling” observed among toddlers in early childhood (Joh and Adolph, 2006).
A remarkable “first-trial” effect has been observed in the adaptive control of stability demonstrated by subjects undergoing these perturbation protocols. This effect is characterized by immediate and often drastic postural changes following the initial exposure to a postural threat (Adkin et al, 2000; Beschorner et al., 2013; Marigold and Patla, 2002; Mcllroy and Maki, 1995; Pai et al., 2003). These findings shed light on the process that must take place in the very first trial. Because subjects who fall in a novel trial are often able to avoid a fall in the next or the following exposures to a slip perturbation (Pai et al., 2003), it is natural to postulate that the basis for this essential learning must exist during the very first exposure.
In this connection, sequence of events that constitute the basis of the motor learning must occur in the first perturbation trial: (1) perturbation-induced motor error must be identified by the central nervous system (CNS); (2) the CNS must select a strategy to respond to the error; and (3) the CNS must implement this strategy by means of motor corrections (Schmidt and Lee, 1999). Motor error (or movement error) represents error signal that leads to motor learning, which prompts update of the existing model for motor control during unskilled performance (Adams, 1971; Lee et al., 2016). To understand how the CNS resists loss of balance induced by the slip perturbation, the stability was defined as a quantification of balance loss from a stable human upright posture. Feasible stability region in the center of mass (COM) state space was established by empirical approach and mathematical modeling (Pai and Patton, 1997). Stability was calculated as the shortest distance from the instantaneous COM motion state to the dynamic feasible stability boundary. Instability specifically represents stability outside of the feasible stability region. The elevated risk of backward balance loss caused by higher instability (lower stability) can be reduced with an adaptive improvement in movement stability (Pai et al., 2003). Since modulation of foot placement is required for both translation of the body and balance of the motion (Maeda et al., 2017; Qiao and Jindrich, 2014), the first protective step after the slip-onset was selected in this study to represent the corrective strategy. The instability immediately before the protective stepping and stability gain from the stepping were taken as the motor error and correction, which could quantify the motor learning.
Individual variability in motor learning should exist, and it makes sense that the subjects who fall during a novel slip exposure (“fallers”) and the subjects who do not (“non-fallers”) would display the greatest between-group differences. It is also possible that fallers learn differently from non-fallers. In older adults, falls are thought to impede individuals’ mobility not only as a result of any injury sustained, but also because they may lead to overly cautious behaviors. If these cautious behaviors are also reflective of the central processes during the novel exposure, then we might expect a mismatch by fallers’ undercompensating (or overcompensating) the motor error with corrective action. Alternatively, because most of these individuals are able to reverse their fall outcomes so rapidly and stop falls in the following trial, they must have learned at least as well as those non-fall cohorts in that very same trial. In such scenario, we would expect that fallers are able to detect and attempt to select and execute similar corrective action as those who did not fall, although their initial attempts may be less effective due to other factors.
The purpose of this study was to explore the relationship between the motor errors subjects experienced upon a novel slip and the selection and execution of corrective response by which they modified their ongoing gait pattern and turned it into a protective step. We hypothesized that community-dwelling older adults would detect the motor error induced by the slip perturbation and select their strategy (measured by their recovery landing distance after the perturbation) according to the magnitude of the errors. Specifically, those with greater posterior instability by the time of the recovery foot liftoff (that is, displaying a greater motor error in the control of stability at the beginning of the action) would modify their regular gait stepping to a greater degree, so that they would land their recovery step further behind the slipping foot (Hypothesis 1a: a linear relationship between error detection and response selection). We further hypothesized that, as a result of the response selection, greater recovery landing distance modification would actually result in greater stability gain at recovery foot touchdown (Hypothesis 1b: a linear relationship between response selection and motor correction). In addition, we hypothesized those who fall during a novel slip symbolized a mismatch between the error detection and the corrective action they subsequently took, and we would therefore expect their motor error-and-correction relationship tested in Hypothesis 1 to be significantly different from those who recovered successfully (Hypothesis 2: mismatch or altered linear relationship in Hypothesis 1).
2. Methods
2.1. Subjects
The recruitment was conducted within a 50-mile radius from the laboratory in the city and the neighboring suburbs of the Greater Chicago Area. One hundred forty-five volunteers (≥ 65 years) came from different senior centers, community exercise centers (e.g., YMCA: Young Men’s Christian Association), independent senior living facilities, the Aging Research Registry of the Buehler Center on Aging at Northwestern University, or from affiliates of the Department on Aging, City of Chicago. They followed a standard protocol and standard criteria (Pai et al. 2014) to be screened for the current use of selected drugs that may alter their control of stability, cognitive impairment (Folstein Mini Mental Status Exam score < 25) (Folstein et al. 1975), or poor mobility (> 13.5 s on the Time-Up-and-Go test) (Podsiadlo and Richardson 1991). All participants had given written informed consent in this study approved by Institutional Review Board in the University of Illinois at Chicago.
2.2. Experimental Setup
Subjects were instructed to walk on a 7-meter walkway (Fig. 1) at their preferred speed and manner. Subjects were informed that they “may or may not be slipped” at any time and that, if a slip occurred, they should “try to recover” and “continue to walk.” None of them were told when, where, or how they might slip. To make the first unannounced slip completely novel, no rehearsal was provided. This trial took place only after ten trials of uninterrupted walking in order to increase the level of difficulty to predict when this novel slip would occur.
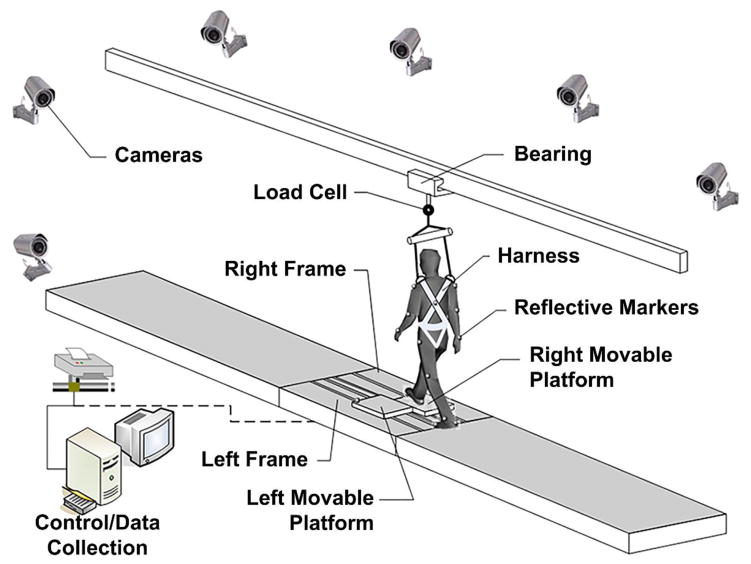
Fig. 1.
The overground walkway with embedded movable platforms. The simulated slip was triggered by the release of two side-by-side low-friction moveable platforms.
The slip was induced by releasing of a pair of side-by-side, low-friction, movable platforms (length = 65.0 cm; width = 30.5 cm) embedded near the middle of the walkway (Fig. 1). The platforms were firmly locked in those first ten walking trials. Each platform was mounted to an aluminum track along the anterior-posterior direction via ball bearings. During a slip trial, each released platform could slide smoothly in the anterior-posterior direction for up to 90 cm forward or 58 cm backward with constraint in medial-lateral movement (Fig. 2c). Upon detection of a subject’s step by force plates (AMTI, Newton, MA, United States) installed beneath the platforms, a computer controlled triggering mechanism would release the electronic mechanical lock that held the platform firmly in place.
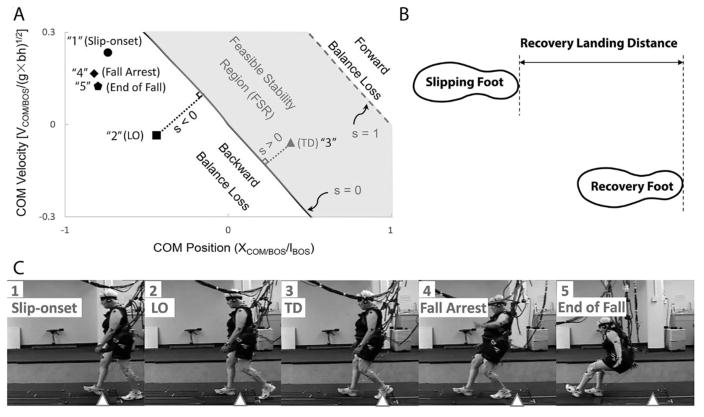
Fig. 2.
The diagrammatic time evolution of center of mass (COM) state stability corresponding video frames of a subject who fell upon a slip. (a) Schematic illustration of the feasible stability region (FSR, the shaded region), which is enclosed by two boundaries: the limits of stability against backward balance loss (the thick solid line, s = 0) and those against forward balance loss (the thick dashed line, s = 1). The COM state stability (s, the length of the thin dotted line) indicates the magnitude of the instantaneous stability of the COM against backward balance loss (refer to Experimental procedures for the calculation of this quantity). The slip trial consists of evolution of stability following the time sequence: slip-onset (solid circle); recovery foot lift off (LO, solid square); recovery foot touch down (TD, solid triangle); fall arrest (solid diamond); and the end of fall (solid pentagon). For the illustrated subject, the COM state moved into FSR because of support from the recovery step, but it moved back to backward balance loss region (stability at fall arrest below 0), which was attributed to a continuous forward travel of the movable platforms remaining with the progress of the fall. (b) The recovery landing distance was calculated as the distance between heel positions of recovery foot and slipping foot at recovery foot touchdown. (c) Still-frame video images (taken after the release of moveable platform) of the same subject. The five frames were taken near slip-onset (frame 1), LO (frame 2), TD (frame 3), fall arrest (frame 4) and the end of fall (frame 5). The triangle in each frame approximates the initial position of the slipping foot at slip-onset.
A full-body harness, connected with shock-absorbing ropes to a load cell (Transcell Technology Inc., Buffalo Grove, IL, United States) mounted an overhead trolley on a track over the walkway, enabled subjects to walk freely while providing protection against body impact with the floor surface (Fig. 2c). Kinematics were recorded by an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA, United States) and a full body marker set composed of 28 retro-reflective markers. Kinematics were sampled at 120 Hz and synchronized with the force plate and load cell data which were collected at 600 Hz (Fig. 1).
2.3. Outcome variables
Four variables were analyzed for each trial: (1) the perturbation-motor error; (2) the response selection; (3) the stability gain immediately after the stepping response; and (4) the outcome of recovery whether or not a fall occurred. The timing of recovery foot liftoff and recovery foot touchdown were identified from the synchronized vertical ground reaction force and motion analysis data. The perturbation induced motor error was characterized by the stability measured at recovery foot liftoff. The response selection was defined by the distance from the heel of the recovery step to the heel of the slipping foot at step touchdown normalized by body height (Fig. 2b). A backward balance loss is defined by the position of the recovery foot that lands posterior to the slipping foot. A longer between-heel distance then means a shorter forward displacement of the recovery foot and a greater modification of this person’s regular gait pattern. The stability gain was measured by the difference in the stability from recovery foot liftoff to its touchdown. A trial outcome was characterized as a fall when the peak force recorded by the load cell in the harness system exceeded 30% of body weight (Yang and Pai, 2011).
The control of stability is the control of the relationship between COM and BOS, which determines balance. Base of support (BOS) represents the area beneath a person encircled by the points of contact that the person’s foot or feet make(s) with the supporting surface. In order to maintain stability at low velocities, one must confine the vertical projection of his or her COM within the BOS. The COM state (position and velocity of the COM relative to the BOS) was used to measure a person’s instantaneous dynamic stability (Pai and Patton, 1997 Yang et al., 2007). First, body COM kinematics were calculated using a 13-segment rigid body model with gender-dependent segmental inertial parameters (de Leva, 1996). Using the motion state of the rear edge of BOS (the right heel) as reference, the relative position and velocity of COM/BOS were then calculated. Relative COM/BOS position was normalized by foot length (lBOS), such that negative values indicate distance behind the BOS. Relative velocity was normalized by the quantity , where g is gravitational acceleration and bh represents the body height. Finally, the COM state stability was computed from the shortest distance from the COM motion state to the dynamic feasible stability boundary against backward loss of balance under slip conditions (Fig. 2a), with the accuracy higher than adequate level of 10−2. When stability values are less than 0, a backward loss of balance must take place, whereas greater values indicate greater stability against backward loss of balance. Position and velocity of the COM relative to the BOS, as well as the stability of the COM state, are all dimensionless variables.
2.4. Statistical analysis
To test Hypothesis 1a, recovery landing distance was regressed on COM stability state at recovery foot liftoff; regressions were performed separately for fallers and non-fallers. Similarly, Hypothesis 1b was tested by regressing change in COM stability state between recovery foot liftoff and recovery foot touchdown on recovery landing distance. To test Hypothesis 2, ANCOVA (Analysis of covariance, a general linear model which blends ANOVA and regression) was used to compare the linear regression slopes between fallers and non-fallers in Hypothesis 1a and 1b, separately. A univariate general linear model was built with the predictor variable as covariate, the group dummy variable as fixed factor and the product of group dummy variable and predictor variable as interaction. All statistical analysis was performed using SPSS 22 (IBM Corp, Armonk, NY).
3. Results
As expected, every subject lost balance following the slip-onset, and took a recovery step that landed posterior to the slipping foot. Upon this novel slip, 72 fell, while the remaining 59 subjects did not fall. Of these 72 subjects, there were 25 “multiple-step fallers” who took more than one recovery steps following the slip onset and before the instant when the load cell force reaches 30% body weight. Notably, 14 fallers underwent maximum modification and aborted stepping altogether (without lifting the trailing foot from the ground) following the slip-onset before a fall was arrested by the protective harness. Because it is impossible to measure the stability gain in these subjects in the same manner as everyone else, they were excluded. Subsequently, the results of the remaining 131 subjects (gender: 93 females, 38 males; age: M = 71.8, SD = 5.2 years; height: M = 165.3, SD = 8.5 cm; mass: M = 73.1, SD = 12.9 kg) are presented here.
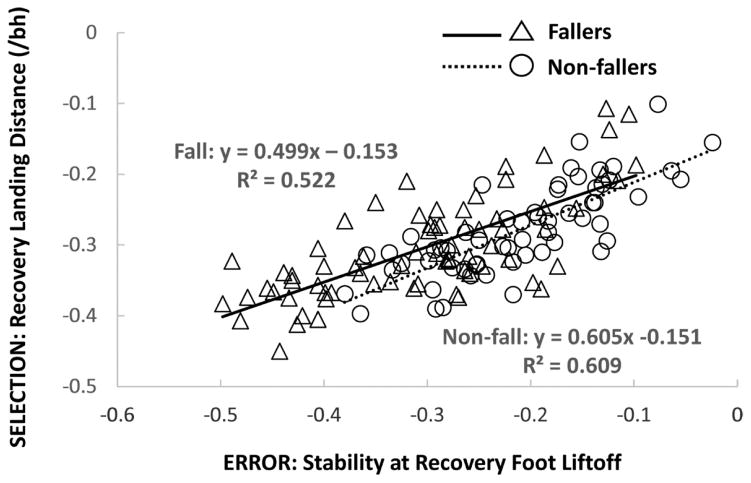
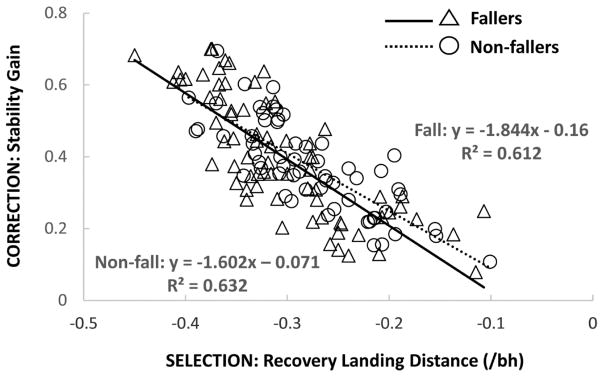
The subjects’ recovery step placement appeared to be dictated by their lack of stability at recovery foot liftoff, and a linear relationship was found between the two [R2 = 0.522, y = 0.499x - 0.153, F (1, 70) = 76.459, P < 0.001 for fallers; and R2 = 0.609, y = 0.605x - 0.151, F (1, 57) = 88.823, P < 0.001 for non-fallers, Fig. 3]. Consequently, the stability gain upon touchdown was also proportional to the step placement, and a linear relationship also existed between these two variables [R2 = 0.612, y = −1.844x - 0.16, F (1, 70) = 110.559, P < 0.001 for fallers; and R2 = 0.632, y = −1.602x - 0.071, F (1, 57) = 97.994, P < 0.001 for non-fallers, Fig. 4]. No significant interaction in the slopes of the linear regression was found between fallers and non-fallers for error-response (P = 0.239, Fig. 3) nor for response-correction relationship (P = 0.335, Fig. 4).
Fig. 3.
The relationship between recovery landing distance and stability at recovery foot liftoff in fallers (triangles; solid regression line) and non-fallers (circles; dashed regression line). The regression equations for fallers and non-fallers are y = 0.499x − 0.153 and y = 0.605x − 0.151, respectively.
Fig. 4.
The relationship between stability gain from recovery foot liftoff to recovery foot touchdown and recovery landing distance in fallers (triangles; solid regression line) and non-fallers (circles; dashed regression line). The regression equations for fallers and non-fallers are y = −1.844x − 0.16 and y = −1.602x − 0.071, respectively.
4. Discussion
The results presented here support both parts of our first but not the second hypothesis. First, proper learning process took place in the very first slip trial, in which a greater motor error and greater instability led to the selection of a more drastic modification of the ongoing motor programming as characterized by the placement of the recovery step further posterior with a longer distance to the forward slipping foot. A linear relationship between these two variables lent support to Hypothesis 1a. Subsequently, a greater modification of the gait pattern led to a greater gain in stability, as demonstrated by the linear relationship between these two variables that lent support to Hypothesis 1b. Finally, not entirely as expected and as stated in Hypothesis 2, the fallers had similar error-response and response-correction relationship regardless whether the outcome was a recovery or a fall.
While every fall resulting from a slip has the potential to be disastrous, the natural ability to learn from novel slips in a safe setting (like a laboratory or rehabilitation center) is a central tenant of perturbation motor learning paradigms. It has long been observed that, in response to postural perturbations with small-scale platform movement, people tend to respond in stereotyped ways which are not necessarily the most effective (Nashner, 1980). Through exposure to life-like slips, it is likely that the human body reshapes these reactions to be more efficacious. After experiencing an environment in which the motor error is more easily predictable, subsequent motor learning should become faster (Takiyama et al., 2015). Our previous paper (Figures 2 & 3 in Pai et al., 2010) showed that subjects’ stability increased significantly and thus the performance was improved drastically from the first to the second slip with rapid reduction in both rate of fall and rate of balance loss. The present study provided insights of what happened in the initial exposure before the remarkable performance improvement taken place in the second exposure to the same distance. A recent paper from our group indicates that this “first trial effect” can be retained for up to one year (Liu et al., 2017), which is strong evidence of the learning effect from only a single trial.
Though the “first trial effect” has been widely observed in motor training as rapid adaptation, the ways corrective responses match motor error resulting from a slip have not been fully examined nor understood. Challenges still remain to directly measure neurological input, output, and responsivity because techniques for studying complex psychological phenomena such as perception, decision making and response planning do not lend themselves to the short timescales required in single-trial motor learning. As such, an indirect approach is necessarily used as an effective alternative to explore the motor corrections to the errors.
To effectively respond to a slip perturbation, we expect that the CNS must first be able to detect the post-slip-onset error, which we analyzed in terms of the COM state instability at the following step liftoff. The COM state stability measures a person’s ability to simultaneously control both the position and velocity of the COM relative to its BOS (Fig. 2a), and reflects this person’s ability to maintain COM stability in upright posture without altering the ongoing gait pattern (Pai and Patton, 1997; Yang et al., 2007). While the limits of stability as such may not be directly computed by the human body in the same mathematical processes as we have derived, all of the information integrated in the evaluation of COM state stability is available in the form of vestibular, proprioceptive, and visual sensory inputs to reshape its future experience of such limits. The rapidness of the adaptive process could be explained only if the CNS merely needs to recalibrate and update an existing internal representation of the stability limits experienced in this first trial rather than to acquire an entirely new motor program (Pai et al., 2003). The proper response resulting from the modification of the ongoing gait pattern displayed in this first trial indeed provides another essential piece of evidence supporting this postulation.
The data presented here support the notion that recovery strategy is a measured response to the motor error detected and that it is enacted via modified foot placement. Foot placement is a major element of locomotion from walking to running, which is consisted of volitional cycles of falling-and-stabilizing (Pai, 2003). Once an unintended perturbation occurs, foot placement is even more critical in restoring stability. Vlutters et al. (2016) found that recovery from medial-lateral perturbations on treadmill walking involved medial-lateral foot placement adjustments proportional to the medial-lateral COM velocity. Hof (2008) reported that changes in foot placement were associated with stability after perturbations in walking. Using both kinematic and EMG data of young adults who experienced backward balance loss upon treadmill perturbation, Kagawa et al. (2011) suggested that the ongoing swing movement and rapid touchdown of the unperturbed swing leg were modulated according to the COM states at liftoff. Our results are consistent with those findings: the older adult’s landing distance of the recovery foot (i.e. foot placement) is linearly correlated with the instability at liftoff and the stability gain at the recovery touchdown after the first slip onset. In this first trial, the subjects exhibited different errors across a certain range (Fig. 3) because each subject’s baseline of balance control varied. After all, the control of stability is only a part of the reasons that lead to a fall. The other is the ability to provide sufficient limb support, which is not a part of the analysis of the present study.
We found that both fallers and non-fallers took shorter forward steps when they experienced a more severe loss of stability (choosing a recovery response appropriate to the error) and changed their COM state stability in proportion to the landing distance of recovery step they chose (effectively implemented the chosen strategies). The absence of a significant difference in these metrics between non-fallers and fallers indicates that both groups learn and implement at least partially effective strategies (that is, strategies which effectively increase the state stability of the COM) in response to a novel slip (Figs. 3 & 4). Elderly fallers and non-fallers were found in other studies to have similar capabilities to generate large amounts of joint moments (i.e., peak torque in hip, knee and ankle joints) (Bento et. al., 2010), similar levels of neuromuscular activation of the hip (although lower rate of torque development) (Morcelli et al., 2015), have shown similar selection of other (cross and side-stepping) recovery strategies upon a waist-pull balance perturbations (Sturnieks el al. 2013). The current study is consistent with these findings in that both fallers and non-fallers appear capable of taking rapid actions to set the recovery foot on the ground to avoid a fall, and both groups appear to use similar strategies. Again, true implication of the present study is NOT about why fallers fell upon the novel fist exposure. Rather, it provides insight to understand why BOTH fallers and non-fallers can successfully resist falls in the second trial: because they all have had intact ability to learn.
Notably, in the fallers, there were 25 multiple-step fallers. The onset of instability and limb collapse occurred much later among the multiple-step fallers than the single-step fallers. When the multiple-step fallers are excluded from analysis, the regressions of error-response and response-correction relationships among the homogeneous single step fallers would be much clearly fitted with higher R squared values (multiple-step fallers included: R2error-response = 0.522, R2response-correction = 0.612; vs. multi-step fallers excluded: R2error-response = 0.620, R2response-correction = 0.731). However, the multiple-step fallers were included to keep the diversity of recovery strategies in the faller group. With both multiple-step fallers and single-step fallers included, the R2 values for fallers were still higher than 50% with significant p values.
There are several limitations to our present study. One is that participants who fell without taking a step were excluded from the analysis. The development of methods and theories by which to compare different recovery strategies – including aborted stepping strategies – requires further exploration. We also note that only healthy older adults were included in this study. How the results may change with a different population (for example older adults with movement disorders) merits further study. Although the stability method we used is different from that proposed by Hof (2008), our methods should be robust to normalization methods.
5. Conclusions
Protective stepping is extremely important in helping people to recover from any unintended postural disturbance. The results of this study indicate that, even when a slip results in an actual fall, the human body still tends to make useful corrections. Greater motor error and greater COM state instability at recovery foot liftoff are likely to lead to greater modification of ongoing motor programming, resulting in greater correction (stability gain), in part, by selecting a shortened forward step placement as strategy. Regardless of recovery outcome, older community-dwelling adults appear to display the same modulation of corrective strategy and efficacy, indicating that simply giving the older adults implicit learning opportunity through slip-training (without instruction) can harness their potential to rapidly learn fall-avoidance strategies from a novel slip
Highlights.
Greater instability led to more posterior landing of the recovery foot following a novel slip.
More posterior landing distance resulted in greater stability gain.
The fallers’ error-response and response-correction relationship was quite consistent as the non-fallers.
Acknowledgments
Funding
This work was supported by the National Institutes of Health [grant numbers RO1-AG029616, RO1-AG044364].
Footnotes
Conflict of interest statement
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams JA. A closed-loop theory of motor learning. Journal of Motor Behavior. 1971;3:111–149. doi: 10.1080/00222895.1971.10734898. [DOI] [PubMed] [Google Scholar]
- Adkin AL, Frank JS, Carpenter MG, Peysar GW. Postural control is scaled to level of postural threat. Gait & Posture. 2000;12:87–93. doi: 10.1016/s0966-6362(00)00057-6. [DOI] [PubMed] [Google Scholar]
- Bento PC, Pereira G, Ugrinowitsch C, Rodacki AL. Peak torque and rate of torque development in elderly with and without fall history. Clinical Biomechanics (Bristol, Avon) 2010;25:450–454. doi: 10.1016/j.clinbiomech.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Beschorner KE, Redfern MS, Cham R. Earliest gait deviations during slips: implications for recovery. IIE Trans Occup. 2013;1:31–37. [Google Scholar]
- de Leva P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. Journal of Biomechanics. 1996;29:1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hayes WC, Myers ER, Robinovitch SN, Van Den Kroonenberg A, Courtney AC, McMahon TA. Etiology and prevention of age-related hip fractures. Bone. 1996;18:77S–86S. doi: 10.1016/8756-3282(95)00383-5. [DOI] [PubMed] [Google Scholar]
- Hof AL. The ‘extrapolated center of mass’ concept suggests a simple control of balance in walking. Human Movement Science. 2008;27:112–125. doi: 10.1016/j.humov.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Joh AS, Adolph KE. Learning from falling. Child Development. 2006;77:89–102. doi: 10.1111/j.1467-8624.2006.00858.x. [DOI] [PubMed] [Google Scholar]
- Kagawa T, Ohta Y, Uno Y. State-dependent corrective reactions for backward balance losses during human walking. Human Movement Science. 2011;30:1210–1224. doi: 10.1016/j.humov.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Lee TD, Eliasz KL, Gonzalez D, Alguire K, Ding K, Dhaliwal C. On the Role of Error in Motor Learning. Journal of Motor Behavior. 2016;48:99–115. doi: 10.1080/00222895.2015.1046545. [DOI] [PubMed] [Google Scholar]
- Liu X, Bhatt T, Wang S, Yang F, Pai YC. Retention of the “first-trial effect” in gait-slip among community-living older adults. GeroScience. 2017;39:93–102. doi: 10.1007/s11357-017-9963-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. Journal of the American Geriatrics Society. 1995;43:1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Herala M, Koski K, Honkanen R, Laippala P, Kivela SL. Fracture risk associated with a fall according to type of fall among the elderly. Osteoporosis International: A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2000;11:631–634. doi: 10.1007/s001980070086. [DOI] [PubMed] [Google Scholar]
- Maeda RS, O’Connor SM, Donelan JM, Marigold DS. Foot placement relies on state estimation during visually guided walking. Journal of Neurophysiology. 2017;117:480–491. doi: 10.1152/jn.00015.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marigold DS, Patla AE. Strategies for dynamic stability during locomotion on a slippery surface: effects of prior experience and knowledge. Journal of Neurophysiology. 2002;88:339–353. doi: 10.1152/jn.00691.2001. [DOI] [PubMed] [Google Scholar]
- Mcllroy W, Maki B. Adaptive changes to compensatory stepping responses. Gait & Posture. 1995;3:43–50. [Google Scholar]
- Morcelli MH, LaRoche DP, Crozara LF, Marques NR, Hallal CZ, Rossi DM, Goncalves M, Navega MT. Neuromuscular performance in the hip joint of elderly fallers and non-fallers. Aging Clinical and Experimental Research. 2015 doi: 10.1007/s40520-015-0448-7. [DOI] [PubMed] [Google Scholar]
- Morley JE. A fall is a major event in the life of an older person. Journal of Gerontology: Medical Sciences. 2002;57:M492–M495. doi: 10.1093/gerona/57.8.m492. [DOI] [PubMed] [Google Scholar]
- Nashner LM. Balance adjustments of humans perturbed while walking. Journal of Neurophysiology. 1980;44:650–664. doi: 10.1152/jn.1980.44.4.650. [DOI] [PubMed] [Google Scholar]
- Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. Journal of the American Geriatrics Society. 1994;42:909. doi: 10.1111/j.1532-5415.1994.tb06576.x. [DOI] [PubMed] [Google Scholar]
- Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. Journal of the American Geriatrics Society. 1993;41:1226–1234. doi: 10.1111/j.1532-5415.1993.tb07307.x. [DOI] [PubMed] [Google Scholar]
- Owings TM, Pavol MJ, Grabiner MD. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clinical Biomechanics (Bristol, Avon) 2001;16:813–819. doi: 10.1016/s0268-0033(01)00077-8. [DOI] [PubMed] [Google Scholar]
- Pai YC. Movement termination and stability in standing. Exercise and Sport Sciences Reviews. 2003;31:19–25. doi: 10.1097/00003677-200301000-00005. [DOI] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Archives of Physical Medicine and Rehabilitation. 2010;91:452–459. doi: 10.1016/j.apmr.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2014;69:1586–1594. doi: 10.1093/gerona/glu087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Patton J. Center of mass velocity-position predictions for balance control. Journal of Biomechanics. 1997;30:347–354. doi: 10.1016/s0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- Pai YC, Wening JD, Runtz EF, Iqbal K, Pavol MJ. Role of feedforward control of movement stability in reducing slip-related balance loss and falls among older adults. Journal of Neurophysiology. 2003;90:755–762. doi: 10.1152/jn.01118.2002. [DOI] [PubMed] [Google Scholar]
- Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Annals of Biomedical Engineering. 2012;40:1111–1121. doi: 10.1007/s10439-011-0477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Qiao M, Jindrich DL. Compensations during Unsteady Locomotion. Integrative and Comparative Biology. 2014;54:1109–1121. doi: 10.1093/icb/icu058. [DOI] [PubMed] [Google Scholar]
- Schmidt RA, Lee TD. Motor control and learning: a behavioral emphasis. Human Kinetics; Champaign, IL: 1999. p. 495. [Google Scholar]
- Schoene D, Lord SR, Verhoef P, Smith ST. A novel video game--based device for measuring stepping performance and fall risk in older people. Archives of Physical Medicine and Rehabilitation. 2011;92:947–953. doi: 10.1016/j.apmr.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Schoene D, Lord SR, Delbaere K, Severino C, Davies TA, Smith ST. A randomized controlled pilot study of home-based step training in older people using videogame technology. PloS One. 2013;8:e57734. doi: 10.1371/journal.pone.0057734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturnieks DL, Menant J, Delbaere K, Vanrenterghem J, Rogers MW, Fitzpatrick RC, Lord SR. Force-controlled balance perturbations associated with falls in older people: a prospective cohort study. PloS One. 2013;8:e70981. doi: 10.1371/journal.pone.0070981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takiyama K, Hirashima M, Nozaki D. Prospective errors determine motor learning. Nature Communications. 2015;6:5925. doi: 10.1038/ncomms6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlutters M, van Asseldonk EH, van der Kooij H. Center of mass velocity-based predictions in balance recovery following pelvis perturbations during human walking. The Journal of Experimental Biology. 2016;219:1514–1523. doi: 10.1242/jeb.129338. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- Yang F, Anderson FC, Pai YC. Predicted threshold against backward balance loss in gait. Journal of Biomechanics. 2007;40:804–811. doi: 10.1016/j.jbiomech.2006.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Pai YC. Automatic recognition of falls in gait-slip training: Harness load cell based criteria. Journal of Biomechanics. 2011;44:2243–2249. doi: 10.1016/j.jbiomech.2011.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]