Abstract
Purpose
The purpose of this study was to study outcomes after using perfluorocarbon liquid (PFCL) as a short-term postoperative vitreous substitute in eyes with retinal detachment from giant retinal tears (GRTs).
Patients and methods
A retrospective consecutive case series of patients with retinal detachment from GRT, who underwent vitrectomy using PFCL as short-term postoperative retinal tamponade. PFCL was left in the eye for a mean of 6.7 days (range 7–8 days) and then replaced with gas or silicone oil (SO). The anatomical and functional outcomes and postoperative complications are reported.
Results
A total of 30 eyes of 29 patients with a follow-up of 26.8 months (range 9–55 months) were included. GRTs had a mean size of 150° (range 90°–270°) with 46.6% of eyes with a tear of >180°. Intraoperative retinal re-attachment was achieved in all cases. No cases of retinal slippage were recorded. Four eyes (13.3%) had re-detachment and further surgery required. At final review, 27 eyes (90.9%) had attached retinas, while the remaining 9.1% had SO in situ. The visual acuity improved in 70% of eyes with 41% improving at least 2 Snellen lines and 35% with visual acuity of 6/12 or better. Mild anterior uveitis developed in six eyes (20%), which resolved on topical steroids. Glaucoma developed in one eye and was controlled medically.
Conclusion
Our study supports the safety and efficacy of PFCL as a short-term postoperative tamponade in cases of GRTs. As it reduces retinal slippage, the use of SO as a primary tamponade decreased in significant proportion of cases.
Introduction
Giant retinal tears (GRTs) are full-thickness retinal tears extending circumferentially for three clock hours (90°) or more.1 Management of GRT-related retinal detachment presents unique challenge to vitreoretinal surgeons because of the high risk of proliferative vitreoretinopathy (PVR), an increased risk of retinal slippage, and re-detachment.
The major problem of GRT surgery is the mobility of the posterior flap, which was solved by the use of intraoperative perfluorocarbon liquid (PFCL). However, avoiding slippage of the posterior flap can be a serious technical challenge when the PFCL is removed, especially when a GRT circumference is >180°.2, 3 To overcome this problem, few studies reported a two-stage surgical procedure to treat GRT where PFCLs were used as a short-term vitreous tamponade with good safety profile and low re-detachment rate.4, 5, 6 It reduces the risk of posterior retinal slippage by allowing extra time for chorioretinal adhesion to take place. An alternative technique to prevent retinal slippage is direct PFCL/silicone oil (SO) exchange with having SO as a primary tamponade in the eye, which can be avoided in the eyes with good visual potential as in macula-on GRT with no PVR. In the United Kingdom, the British Giant Retinal Tear Epidemiology Eye Study (BGEES)7 showed that PFCL was used only intraoperatively and nearly 80% of cases had SO as a primary tamponade, whereas 54.8% were a fovea-on detachment and 69.4% had no PVR.
The two-stage technique is not popular among vitreoretinal surgeons, as it results in at least two consecutive surgeries for each patient as compared with a mean of 1.19 surgeries as reported by Lee et al8 and another factor is the risk of PFCL-related complications, eg, raised intraocular pressure (IOP), cataract progression, and intraocular inflammation.
We adopted this technique for managing GRT-related retinal detachment 10 years ago and here we report our long-term follow-up results, including primary and final anatomical success rate, functional outcome, and complications.
Patients and methods
This is a retrospective case series of 30 eyes of 29 consecutive patients with a mean age of 43.7 years (range 10–82), who had GRT-related retinal detachment repair between May 2008 and August 2016 at The Royal Victoria Hospital in Belfast, a tertiary referral centre in Northern Ireland with six vitreoretinal surgeons. All patient charts were reviewed and the following data recorded: age, sex, presenting complaints, size and position of GRT, presence or absence of PVR, macular status, pre-and post operative vision, duration of PFCL tamponade, and follow-up in months. Cases having retinal slippage or re-detachment rate were noted.
The authors confirm that data collection conformed to all local policy at Belfast Health and Social Care Trust, and this study is registered with the audit department (number 4973).
Surgical technique
Conventional three-port pars plana 20 or 23G vitrectomy (PPV) was performed with non-contact wide-field viewing system. After completing core and peripheral vitrectomy, the edges of the tear (s) were marked with endo-diathermy, then perfluoro-n-octane (PFO, FCI S.A.S, Paris, France), which is a perfectly pure PFCL with non-volatile residues, non-detectable fluorides, and non-detectable ion hydrogen C–H link injected slowly over the optic nerve head to unroll the folded retina and continued until a single bubble fully filled the vitreous cavity. Cryotherapy is applied to the edges of the tear, followed by three to four rows of endophotocoagulation applied around the tear and to the vitreous base 360° in all eyes. The sclerotomies were closed with 7–0 vicryl sutures.
PFO was left in the eye and patients were asked to position according to the location of their GRT—usually lying on the ipsilateral side or sitting upright for inferior GRT.
Patients were advised to alternate this posturing position with lying supine every 10–20 min, to avoid prolonged tamponade in one particular position. A second-stage surgery to remove the PFO was performed after a week with PFO/BSS fluid exchange followed by internal search by indentation, to examine retinal periphery.
Following this, air–fluid exchange was performed with subsequent air/gas (either SF6, C2F6, or C3F8) or SO (1,000-CS) exchange. During the second stage, cryotherapy and/or endolaser photocoagulation was used for further re-enforcement of the retina if deemed necessary.
Outcome measures
The main outcome measures were as follows: (1) primary anatomical success, retinal reattachment, and no residual tamponade after 3 months after PFCL removal; (2) final anatomical success, retinal reattachment with more than one operation after PFCL removal, and no residual tamponade; (3) failure, persistent retinal detachment anywhere, or retinal reattachment with long-term SO tamponade; (4) visual acuity outcome; and (5) complications related to PFCL use.
Results
Thirty eyes of 29 patients with retinal detachment associated with GRT were included in the study. Of these, 23 patients were male and 6 patients were female, with 16 right eyes and 14 left eyes affected. The mean age was 43.7 years (range10–72). In all, 27 patients were Caucasian, 1 Asian and 1 African with known sickle cell retinopathy. Postoperative follow-up period ranged from 9 to 55 months with mean 26.8 months.
The 30 eyes included 20 idiopathic GRTs, 3 presumed traumatic GRTs, and 3 iatrogenic post PPV GRTs. Seven eyes were highly myopic. One patient had features of Stickler’s syndrome. Twenty-one eyes were phakic, 8 were pseudophakic, and 1 eye was aphakic.
Patient’s demographics are shown in Table 1. Mean pre-operative BCVA was 1.1 LogMAR (range 0–3.5). Fourteen eyes had macula-on RRD and 16 eyes were macula-off. The mean size of the GRTs was 150° (range 90–270) with 54% were <180°, 46% from 180 to 270°, and no GRT >270°. The tears were wholly or partially located inferiorly in five of the cases. One patient had two GRTs measuring 150° each. Four eyes had PVR grade C pre-operatively (Retina Society classification). Simultaneous scleral buckling procedure or lens surgery was not performed at the time of planned two-stage surgery.
Table 1. Patient demographics.
| Preoperative characteristics | No of eyes (total=30) | % |
|---|---|---|
| Eye | ||
| Right eye | 16 | 54% |
| Left eye | 14 | 46% |
| Gender | ||
| Male | 23 | 76.6% |
| Female | 7 | 23.4% |
| Mean age | 43.7 | |
| Predisposing factors | ||
| High myopia >−6D | 7 | 23.3% |
| Blunt trauma | 3 | 10% |
| Previous vitrectomy | 3 | 10% |
| Stickler’s syndrome | 1 | 3.3% |
| PVR grade | ||
| None | 26 | 86.7% |
| PVR-C | 4 | 13.3% |
| Lens status | ||
| Phakic | 21 | 70% |
| Pseudophakic | 8 | 26.7% |
| Aphakic | 1 | 3.3% |
| Macular status | ||
| Macula-ON | 14 | 46% |
| Macula-OFF | 16 | 54% |
| Size of GRT | ||
| 90–180° | 16 | 54% |
| 180–270° | 14 | 46% |
| >270° | 0 | 0% |
Intraoperative findings included intraoperative retinal reattachment in all 30 eyes. SF6 20% was used in 13.3% (4) of eyes, C2F6 12% in 3.3% of eyes (1), C3F8 14% was used in 56.6% (17) eyes, and 23.3% (7) eyes had SO. The mean follow-up period was 24.9 months (range 2–48). Re-detachment occurred in four eyes in the first 3 months; three had PVR and one eye had new tears. A total of four eyes underwent further surgery, three with repeated vitrectomy and one with combined SB and PPV.
At final follow-up, the anatomic success rate was 27 of 30 eyes (90%) had flat retina with no tamponade and the remainder 3 eyes have SO in situ. In terms of visual function, 70% had an overall improvement in vision, 42 improved by 2 lines, and 35% had 6/12 vision or better. The comparison of pre-operative and final postoperative visual acuity is shown in Figure 1. Cataract developed in 50% of eyes during follow-up. Raised IOP developed in two eyes; one patient had PFO in the anterior chamber, and six eyes had anterior uveitis that settled on topical steroids. There were no patients that required long-term management with steroids.
Figure 1.
Scatter plot of presenting visual acuity and the postoperative visual acuity (Snellen acuities were converted to logMAR).
Discussion
This case series of 30 eyes from the only tertiary referral centre in Northern Ireland is comparable to the nation-wide survey of GRT in the United Kingdom (BGEES) study7 in terms of patient demographics with the usual male predominance and >50% of idiopathic/spontaneous etiology. The current study showed that a high anatomic success can be obtained using PFO as a short-term tamponade. Our success rate is comparable to other published results that did not use similar technique. In the BGEES study7, primary and final success rates of 88 and 95%, respectively, were achieved. Similar results were reported from Asia8 where surgical success rate was reported at 84.8% after a mean of 1.19 surgeries.
Failure of retinal detachment surgery in eyes with a GRT can be related to the inadequate tamponade to the retina by gas or SO, which can allow fluid to seep under the edge of the tear before firm chorioretinal adhesion takes place. This can lead to retinal slippage, and/or reopening of the GRT.9 Retinal slippage is not uncommon but far under-reported and can lead to various complications such as hypotony, retinal folds, and may exacerbate PVR formation. Slippage typically occurs during PFO/air exchange due to the presence of a wedge of aqueous in the interface between the air and the PFO, and as the exchange progresses this wedge of fluid with the posterior edge of the GRT can be pushed posteriorly causing curvilinear fold of the retina. A traditional advice is to tilt the eye using a non-contact wide field viewing system and aim to achieve complete drying of the posterior edge of the GRT during the exchange of PFO and air. However, complete dryness of fluid is very difficult because visualization and access is very difficult especially in phakic patients when lens surgery has not been performed simultaneously. Therefore, some retinal surgeons would advocate direct PFO/SO exchange that is associated with less risk of retinal slippage. However, it is desirable to avoid SO in eyes with no PVR and good visual potential such as macula on detachments. In our series of 30 eyes, there were no cases of retinal slippage and only 23% had SO as a primary tamponade.
Intraoperative PFCLs are a useful tool in the management of GRTs, because it can act like a ‘third hand’ during surgery to unfold the inverted tear flap and to displace the subretinal fluid so laser and cryotherapy can be applied. Most case series using PFCL as an intraoperative tool have shown an increase in the success rate. Chang et al2 reported a final success rate of 94% however, 52.9% of eyes needed further surgical procedure for re-attachment of the retina and some eyes developed posterior retinal slippage during A/F exchange and patients had to be turned to prone position. This current study reports using PFO as an intraoperative tool and as a short-term postoperative tamponade.
The presence of a GRT on its own is a significant risk factor for PVR. Reasons for high rate PVR formation in GRTs are unclear possibly because of to the exposure of a large area of bare retinal pigment epithelium to the vitreous cavity.10 Other factors predisposing to PVR formation include younger age and a large amount of cryotherapy or photocoagulation intraoperatively resulting in increased blood–retinal barrier breakdown. Our two-stage technique might theoretically reduce postoperative inferior PVR formation because PFCLs displace inflammatory cells and mediators off the inferior retinal surface. Nine percent of eyes in this study developed postoperative PVR that led to failure and re-detachment.
Several studies have confirmed that postoperative PFO tamponade is safe and superior to other PFCLs including perfluorodecalin.11, 12 Outer retinal thinning and a mild inflammatory changes were found in PFO-retaining rabbit eyes; these changes seem to have occurred after 1 or 2 months of internal tamponade. Bottoni et al13 used PFCLs as a short-term tamponade in 11 eyes and 4 of 11 eyes had an electroretinogram (ERG), which showed a mild nonspecific reduction in b-wave amplitude following PFCL removal, and this remained stable throughout the follow-up period. In our study, we did not find any change in BCVA when compared macula-on GRT detachment preoperatively and postoperatively, suggesting that in the short-term PFO tamponade appears safe.
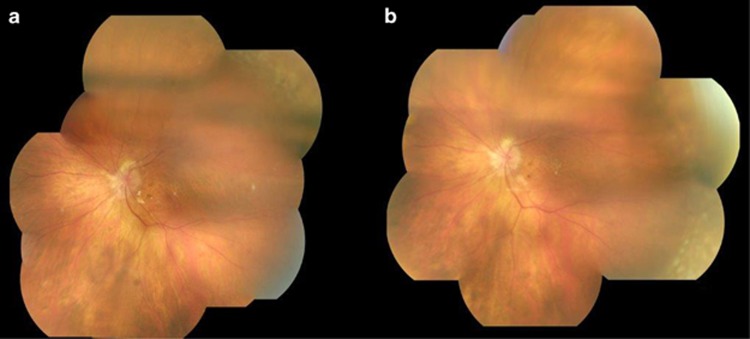
Table 2 shows a summary of the few studies that used a similar technique.4, 5, 6, 13, 14 Our reported postoperative complications were similar to previously published reports using PFO as a short-term postoperative tamponade.4, 5, 6, 13, 14 No patients in our series developed long-lasting complications affecting final visual outcome that could be attributable to PFO. In our series, 54.1% of phakic patients developed cataract during the follow-up period, which is similar to what has been reported by Rofail and Lee.5 Epiretinal membrane formation was recorded at 4.1% compared with 25% recorded by Rofail and Lee.5 A mild postoperative anterior segment inflammation was found in 25% of eyes, managed with topical steroids only, compared with 30.4% in the study by Randolph et al.14 One patient had persistent PFCL droplets in the AC but this was not associated with increased inflammation or raised IOP but was troublesome to the patient as they were aware of it. Two patients developed steroid response raised IOP, one of whom developed secondary open angle glaucoma. Figure 2 demonstrates fundus pictures taken at day 1 post vitrectomy and tamponade with PFO and day 7 before PFO removal (A and B, respectively) and showing the absence of inflammatory changes.
Table 2. Summary of studies that used PFCL as a short-term tamponade in management of giant retinal tear.
| Bottoni et al.13 | Rofail and Lee5 | Sirimahraj et al.6 | Rush et al.4 | Randolph et al.14 | |
|---|---|---|---|---|---|
| Year | 1994 | 2005 | 2005 | 2012 | 2016 |
| No of eyes | 11 | 16 | 62 | 10 | 23 |
| PFCL used | Decaline | Octane | Octane | Octane | Octane |
| PVR | 100% Grade B | 18.8% Grade C | 29% | NA | 21% Grade A or B |
| GRT>180° | 34% | 43.8% | 27.4% | NA | |
| Duration of short-term tamponade (Range) | 5 Days | Mean 16.4 days (6–50 days) | Mean 7.5 days (5–14 days) | 7–17 Days | Mean 18.78 days (7–31 days) |
| Intraoperative attachment | 100% | 100% | 100% | 100% | 100% |
| Primary success rate (after one operation) | 82% | 93.7% | 78.4% | NA | 91.3% |
| Final success at last visit | 94% | NA | 93.5% | 90% | NA |
| Visual acuity at last visit (6/12 or better) | 69% | 68% Improved overall | 46.5% | NA | NA |
Figure 2.
Fundus pictures taken at day 1 post vitrectomy and tamponade with PFO and day 7 before PFO removal (a and b, respectively), and showing the absence of inflammatory changes.
In our series, we achieved a final success rate of 90.9% (27 of 30 eyes), similar to the BGEES study but with a significantly lower percentage of eyes that had SO as a vitreoretinal tamponade; 23 and 80%, respectively. SO has its own profile of side effects and disadvantages including unexplained visual loss after its removal, which can be catastrophic in macula-on GRT-related detachment. Moya et al15 reported 26 cases of macula-on retinal detachment secondary to GRT, 10 cases developed visual loss after removal of SO, giving a rate of visual loss (2 or more Snellen line) of nearly 50% in this subgroup. One of seven patients in our series developed unexplained visual loss after removal of SO which shows the potential risks of SO as the routine tamponade agent, which is a particular concern in eyes that were macula-on at presentation (14 eyes out of 30 in our series).
To conclude, this case series offers an alternative technique in the management of GRT, which appears safe and effective. In the experience of the authors, this technique has a shorter learning curve and is technically easier to perform compared to other surgical techniques. In addition, the need for SO as a primary tamponade in some eyes is reduced. Potential drawbacks are the multiple surgeries in every patient and PFO-related complications including raised IOP, progression of cataract, and intraocular inflammation.
Footnotes
This paper was presented as an eposter at the European Society of Retinal specialists (Euretina) in September 2016 and as an oral presentation in British and Eire association of vitreoretinal surgeons in November 2016.
The authors declare no conflict of interest.
References
- Schepens CL, Dobbie JG, McMeel JW. Retinal detachments with giant retinal breaks: preliminary report. Trans Am Acad Ophthalmol Otolaryngol 1962; 66: 471–478. [PubMed] [Google Scholar]
- Chang S, Lincoff H, Zimmerman NJ, Fuchs W. Giant retinal tears. Surgical techniques and results using perfluorocarbon liquids. Arch Ophthalmol 1989; 107(5): 761–766. [DOI] [PubMed] [Google Scholar]
- Scott IU, Murray TG, Flynn HW, Feuer WJ, Schiffman JC. Outcomes and complications associated with giant retinal tear management using perfluoron-octane. Ophthalmology 2002; 109(10): 1828–1833. [DOI] [PubMed] [Google Scholar]
- Rush R, Sheth S, Surka S, Gregory-Roberts J. Postoperative perfluoro-Noctane tamponade for primary retinal detachment repair. Retina 2012; 32: 1114–1120. [DOI] [PubMed] [Google Scholar]
- Rofail M, Lee LR. Perfluoro-octane as a postoperative tamponade in giant retinal tears. Retina 2005; 19: 675–679. [DOI] [PubMed] [Google Scholar]
- Sirimahraj M, Balachandran C, Chan WC, Hunyor AP, Chang AA, GreogryRoberts J et al. Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol 2005; 89(1176): 1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang GS, Townend J, Lois N. Epidemiology of giant retinal tears in the United Kingdom: the British Giant Retinal Tear Epidemiology Eye Study (BGEES). Invest Ophthalmol Vis Sci 2010; 51(9): 4781–4787. [DOI] [PubMed] [Google Scholar]
- Lee SY, Ong SG, Wong DKW, Ang CL. Giant retinal tear management: an Asian experience. Eye 2009; 23: 601–605. [DOI] [PubMed] [Google Scholar]
- Krieger AE, Lewis H. Management of giant retinal tears without scleral buckling. Use of radical dissection of the vitreous base and perfluoro-n-octane and intraocular tamponade. Ophthalmology 1992; 99: 491–497. [DOI] [PubMed] [Google Scholar]
- Mathis A, Pagot V, Gazagne C, Malecaze F. Giant retinal tears: surgical techniques and results using perfluorodecaline and silicone oil tamponade. Retina 1992; 12: 7–10. [DOI] [PubMed] [Google Scholar]
- Chang S, Sparrow J, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina 1991; 11: 367–374. [PubMed] [Google Scholar]
- Singh J, Ramesh K, Wharton SB, Cormack G, Chawla HB. Perfluorodecalininduced intravitreal inflammation. Retina 2001; 21: 247–251. [DOI] [PubMed] [Google Scholar]
- Bottoni F, Bailo G, Arpa P, Prussiani A, Monticelli M, de Molfetta V. Management of giant retinal tears using perfluorodecalin as a postoperative short term vitreo-retinal tamponade: a long term follow-up study. Ophthalmic Surg 1994; 25: 365 373. [PubMed] [Google Scholar]
- Randolph JC, Diaz RI, Sigler EJ, Calzada JI, Charles S. 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for the repair of giant retinal tears. Graefes Arch Clin Exp Ophthalmol 2016; 254: 253–257. [DOI] [PubMed] [Google Scholar]
- Moya R, Chandra A, Banerjee PJ, Tsouris D, Ahmad N, Charteris DG. The incidence of unexplained visual loss following removal of silicone oil. Eye 2015; 29: 1477–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]