Abstract
The purpose of this systematic review is to report current preoperative assessment for femoroacetabular impingement (FAI) including physical examination and imaging modalities prior to hip arthroscopy, and report current imaging measures used in the diagnosis of FAI. The electronic databases MEDLINE, EMBASE and PubMed were searched and screened in duplicate for relevant studies. Data regarding patient demographics, non-operative treatment, preoperative assessment including physical examination and imaging prior to hip arthroscopy were abstracted. Study quality was assessed in duplicate using the Methodological Index for Non-Randomized Studies criteria. Sixty-eight studies of fair quality evidence that involved a total of 5125 patients (5400 hips) were included. In total, 56% of all patients were male and mean age was 36 years (SD ± 10.0). Within physical examination, FADIR impingement testing was reported in 57% of patients. All included studies reported plain radiographic imaging as a component of preoperative assessment with anterior–posterior pelvis view being the most commonly reported view, followed by the cross-table lateral and Dunn views. Magnetic resonance imaging was obtained for 52% of included patients and computed tomography for 26% of patients. The most commonly reported measure within imaging for the diagnosis of cam type impingement was alpha angle (66%), whereas for pincer type impingement, the cross-over sign (48%) was most reported. Preoperative assessment is underreported in the FAI literature. Improved reporting is warranted to develop a more consistent and validated diagnostic algorithm for FAI to enhance patient selection.
Level of evidence: Level IV, Systematic Review of Level I–IV Studies.
INTRODUCTION
Hip arthroscopy has numerous indications with femoroacetabular impingement (FAI) being one of the most common [1–3]. FAI is often classified as either cam or pincer type; though combinations of both types exist in clinical practice [4]. Cam type impingement is the result of abnormal femur morphology typically defined by a decrease in anterior femoral head neck offset or an aspheric femoral head. Comparatively, pincer impingement arises due to morphologic variation on the acetabular side with focal or global over-coverage of the femoral head [5]. Arthroscopic treatment is a surgical treatment option for cam, pincer and mixed type FAI [4]. It is, however a demanding procedure due to anatomic and mechanical constraints and thus is associated with a significant learning curve [6–8].
The success of demanding surgical procedures like hip arthroscopy depends in part on appropriate patient selection during preoperative assessment [9]. Preoperative assessment allows the surgeon to confirm the suspected diagnosis and determine whether the patient is an appropriate candidate for the procedure [9]. Further, it is at this stage that the surgeon is able to plan for the procedure, anticipate issues that may arise during surgery and take appropriate measures to minimize risk for failure and/or future revision surgery [9]. Amongst the existing literature, the main indication for revision in FAI treated arthroscopically is residual cam or pincer deformity [8]. Appropriate and standardized preoperative assessment may better characterize impingement lesions; however, how this may mitigate residual deformity as a cause for revision remains unknown.
Preoperative assessment typically consists of a thorough history, physical exam and diagnostics such as imaging in the case of FAI. With regard to FAI, several physical examinations are used in clinical practice and can include the: FADIR (flexion, adduction, internal rotation) test, FABER (flexion, abduction, external rotation) test, log roll test, gait assessment and maximal squat test [4, 10–12]. FADIR is considered one of the most sensitive tests with a sensitivity of 0.99 [13, 14]. It is also recommended that provisional diagnoses of FAI be confirmed by imaging wherein several different imaging modalities as well as views within these modalities are used in routine practice [3, 4]. Magnetic resonance imaging (MRI) protocols for FAI have also been developed with Magnetic Resonance Arthrography (MRA) known to be of particular use for the assessment of intra articular pathology such as labral tears [15, 16]. Computed tomography (CT) is also used and has long been considered the best imaging modality to assess bony abnormalities, though is less helpful in assessing soft tissue injuries of the hip [17]. Further, several measurements can be made on imaging to assist in the diagnosis of FAI and distinguish between the different types of FAI [4, 5]. Cam type impingement is often defined by the alpha angle, and head-neck offset, and femoral asphericity on imaging. Features suggestive of pincer type impingement include the: cross-over sign, coxa profunda or protrusion, high center-edge angle (CEA) and signs of global or segmental acetabular retroversion or anteversion [4, 5]. Additionally, both types of impingement are associated with osteoarthritis often measured on imaging by Tönnis grade and Kellgren-Lawrence classification [18].
Currently, neither there is gold standard physical examination, imaging modality or measures on imaging to support the diagnosis of FAI nor is there a consensus on what should be included in preoperative assessment prior to hip arthroscopy [4, 6]. The purpose of this review paper is to report the current preoperative assessment used in patients with FAI including physical examination and imaging modalities prior to hip arthroscopy and specific imaging measures used in the diagnosis of FAI.
MATERIALS AND METHODS
Search strategy
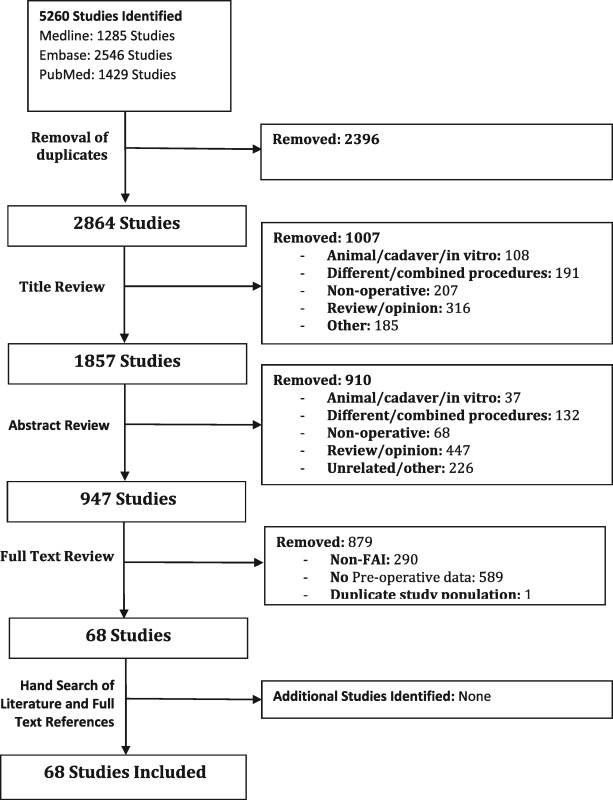
A systematic search strategy previously described by the authors was employed [19]. Two reviewers searched three online databases (EMBASE, MEDLINE and PubMed) for literature related to hip arthroscopy. The following MeSH terms were used in the search; ‘hip’ and ‘arthroscopy’. A table outlining the search strategy is presented in Appendix 1. The PRISMA guidelines were followed in the development of this study. The search was conducted 16 March 2016 and retrieved articles from database inception (EMBASE: 1980, MEDLINE: 1966, PubMed: 1950) to the search date (16 March 2016). The research question and individual study eligibility criteria were established a priori. Inclusion criteria were: (1) all levels of evidence; (2) male and female patients of all ages; (3) studies published in English; (4) human studies; (5) studies reporting on surgical technique (including: approach, use of anesthesia, number of portals, traction, use of intraoperative imaging); (6) studies reporting details regarding preoperative assessment (imaging and/or physical examination) of FAI prior to arthroscopy and (7) studies reporting on patients with suspected or confirmed FAI. Exclusion criteria were: (1) non-surgical treatment studies; and (2) studies where the outcomes for the exact same patient population were reported in multiple articles (most recent article included).
Study screening
Two reviewers independently screened the titles, abstracts and full texts of retrieved studies. Data abstraction was performed between 11 April 2016 and 18 May 2016. Discrepancies at the title and abstract stages were resolved by automatic inclusion to ensure thoroughness; discrepancies at the full text stage were resolved by consensus between the reviewers. If a consensus could not be reached a third, more senior reviewer helped to resolve the discrepancy. The references of included studies were screened to capture any articles that may have been missed.
Quality assessment of included studies
A quality assessment of included studies was completed using the Methodological Index for Non-Randomized Studies (MINORS) Criteria [20]. The MINORS score represents a validated tool for non-randomized studies (e.g. case reports, case series, cohort studies etc.). Each of the 12 items in the MINORS criteria is given a score of 0, 1 or 2—with maximum scores of 16 and 24 for non-comparative and comparative studies, respectively.
Data abstraction
Two reviewers independently abstracted relevant data from included articles and recorded this data in a Microsoft Excel (2013) spreadsheet designed a priori. Demographic information included author, year of publication, sample size, study design, level of evidence and patient demographics (sex and age). In addition, information regarding non-operative treatment prior to surgery, physical examination, imaging modalities used (including views) and radiograph, MRI or CT measurements were also documented.
Statistical analysis
A kappa (κ) value was calculated for each stage of article screening to evaluate inter-reviewer agreement. Agreement was categorized a priori as follows: κ > 0.60 to indicate substantial agreement, 0.21 ≤ κ ≤ 0.60 to indicate moderate agreement and κ < 0.21 to indicate slight agreement [21]. An intra-class correlation coefficient (ICC) was used to evaluate inter-reviewer agreement MINOR scores [20–22]. Descriptive statistics, such as means, ranges and measures of variance (e.g. standard deviations) are presented where applicable. No meta-analysis was performed, due to considerable heterogeneity amongst studies in terms of clinical features such as imaging modalities used, non-operative management and history items and physical examination techniques used.
RESULTS
Study characteristics and quality
From an initial search of 5260 studies, 68 studies, all published between 2007 and 2016, satisfied the inclusion criteria for this systematic review (Appendix 1). Among the 68 included studies: 51 were assessed as Level 4, 7 as Level 3, 9 as Level 2 and 1 as Level 1 (Appendix 2). Most studies were based in North America (N = 35), followed by Europe (N = 20); the remainder were from Asia (N = 5), Australia (N = 5) and South America (N = 3). There was substantial agreement amongst reviewers for all aspects of the study: (i) screening at title (κ = 0.73; 95% CI: 0.70–0.75), abstract (κ = 0.79; 95% CI: 0.76–0.82) and full-text screening (κ = 0.97; 95% CI: 0.95–0.999), as well as (ii) MINORS assessment (ICC 0.90, 95% CI 0.84–0.94). The included studies had an overall mean MINORS score of 11.68 ± 3.81 (fair quality) with comparative studies having a mean score of 21.29 ± 1.68 and non-comparative studies with a mean score of 10.60 ± 2.05.
Patient demographics
A total of 5125 patients (5400 hips) were available at final follow-up. Fifty-six percent of all patients were male (2106 of 3785 patients across 55 studies) and 61.8% of procedures were performed on the right side (620 out of 1002 patients across 30 studies). The combined mean age of patients was 36 years (range = 11–82 years, SD ± 10.0).
Prior non-surgical treatment
Prior non-surgical treatment was reported in 25% of patients (1264 patients). With respect to duration of non-surgical treatment, the mean duration of non-operative treatment was 10.1 months (SD ± 10.1) with a range of 1.5–24 months (in 886 patients). Non-surgical treatment when specified, included activity modification (564 patients), non-steroidal anti-inflammatory or other analgesic (534 patients), physical therapy (377 patients) and intra-articular injection (102 patients).
Patient history and physical examination
Patient symptoms of FAI were reported in 36% (1848 patients) of included patients. Hip and/or groin pain reported in 65% of these patients. Pain that was aggravated by activity and/or sport was reported in 50% and pain with sitting was reported in 5% of patients. Mechanical symptoms (locking, catching) were reported in 10% of these patients.
Preoperative physical examination was reported on in 2992 patients (58%) (Table I). Preoperative physical examination reported in the included studies included range of motion, impingement tests and assessment of gait. Impingement testing was used in the vast majority of patients at 87.0%. Within studies that used impingement testing, 57% of patients were tested for anterior impingement with FADIR testing, 41% were tested with FABER testing and 27% with impingement sign. Few studies reported on the range of motion tested, however those that did reported assessment of restriction of flexion, and internal rotation and external rotation (measured at 90° of hip flexion). Strength testing was examined in a single case report where no strength deficits were detected. Intra-articular diagnostic injection was performed in 7.0% of patients. The type of anesthetic was specified in a single study of 36 patients where lidocaine was used.
Table I.
Physical examination
| Physical examination | Number of patients (%) |
|---|---|
| Any impingement testing | 2590/2992 (87%) |
| • FADIR/Anterior Impingement Testing | 1477/2590 (57%) |
| • FABER Impingement Testing | 1072/2590 (41%) |
| • Unspecified Impingement Testing | 706/2590 (27%) |
| • FADIR and FABER Testing | 665/2590 (26%) |
| • Lateral Impingement Testing | 47/2590 (2%) |
| • Posterior Impingement Testing | 47/2590 (2%) |
| Restricted range of motion testing | 1336/2992 (45%) |
| • Range of Motion and Impingement Testing | 1321/2992 (44%) |
| Log Roll | 377/2992 (13%) |
| Observation of Gait | 367/2992 (12%) |
| Hip Dial | 85/2992 (3%) |
Preoperative imaging
All included studies reported plain radiographic imaging as a component of preoperative assessment (Table II), with the most commonly reported view was being the anterior–posterior (AP) pelvis (97%), followed by cross-table lateral (40%) and Dunn view (40%), false-profile (27%), lateral (15%), extended neck lateral (6%), frog leg lateral (6%) and axial (3.5%).
Table II.
Imaging modalities and view/sequences used
| Imaging modality | Studies using (patients) | Studies reporting views (patients) | Number of views reported: percentage (patients) | Views used: percentage (patients) |
|---|---|---|---|---|
| Radiograph | 68 (5125) | 51 (4066) |
|
|
| Imaging modality | Studies using (patients) | Type (patients): | ||
| Computed tomography (CT) | 19 (1352) | 3D CT: 7 studies (629) | ||
| Magnetic resonance imaging (MRI) | 48 (2652) |
|
||
MRI use was reported in 52% of patients. Type of MRI was reported in 14% of patients that underwent MRI where MRA was the most commonly used. The most commonly used sequence was T1-weighted followed by use of both T1 and T2-weighted MRI (Table II).
CT use was reported in 26% of patients. It was further specified in seven studies that 47% of these patients underwent a 3 D-CT. Fourteen studies used CT for all patients (1007 patients, 65%), and five studies (544 patients, 35%) used it on some patients (Table II).
In terms of combinations of imaging used, the most common combination used was plain radiographic imaging with MRI, which was used in 37% of patients. This was followed by plain radiographic imaging used in isolation, plain radiographic imaging with CT and MRI and lastly, plain radiographic imaging with CT (Table III).
Table III.
Imaging modality combinations used
| Imaging used | Percentage (patients) | Used along with impingement testing percentage (patients) |
|---|---|---|
| Radiograph only | 37% (1880) | 38% (980/2590) |
| Radiograph and MRI | 37% (1893) | 33% (850/2590) |
| Radiograph and CT and MRI | 15% (759) | 10% (269/2590) |
| Radiograph and CT | 12% (593) | 19% (491/2590) |
Radiographic, CT and MRI measures of FAI
Seventy-five percent of patients (3863 patients) had specific radiographs, MRI and CT measurements reported that assisted in diagnosis (Table IV). For cam impingement, these included the alpha angle (55° cut off, range 45°–60°) loss of femoral head sphericity and loss of femoral head neck offset. For pincer impingement, the cross-over, center edge angle (CEA), acetabular retroversion and other measures of retroversion (ischial spine sign, posterior wall sign) were used.
Table IV.
Measures of femoroacetabular impingement on imaging
| Measures of FAI on Imaging: | Studies with measures on imaging: 51 (3863) | Studies that did not distinguish between type of FAI (852) | Studies that distinguished between cam, pincer or reported mixed type (3004) |
|---|---|---|---|
| Cam impingement | Number of patients (%): | ||
| Alpha Angle | 2419 (66%) | 590 (69%) | 1829 (61%) |
| Loss of head sphericity | 1066 (29%) | 243 (29%) | 823 (27%) |
| Femoral head neck offset | 567 (15%) | 246 (29%) | 321 (11%) |
| Pistol Grip Deformity | 148 (4%) | 77 (9%) | 71 (2%) |
| Pincer impingement | Number of patients (%): | ||
| Cross over sign | 1762 (48%) | 277 (33%) | 1485 (49%) |
| Coxa profunda | 1496 (41%) | 212 (25%) | 1284 (43%) |
| Acetabular Retroversion | 845 (23%) | 278 (33%) | 567 (19%) |
| Acetabular protrusion | 1445 (39%) | 180 (21%) | 1265 (42%) |
| Center edge angle | 1537 (42%) | 462 (54%) | 1075 (36%) |
| Posterior wall sign | 277 (7%) | 0 | 277 (9%) |
| Ischial spine sign | 223 (6%) | 0 | 223 (7%) |
| Osteoarthritis | Number of patients (%): | ||
| Tönnis Grade of OA | 1747 (47%) | 521 (61%) | 1226 (41%) |
Within studies reporting on FAI measures, 21 studies (823 patients) did not distinguish between cam and pincer types of FAI within imaging measures and within patients. The remaining studies distinguished between cam, pincer and/or combined types. In studies that reported on FAI in general, alpha angle, Tönnis Grade and CEA were the measures that were most often reported. In studies that did distinguish, alpha angle was the measure most often used in cam type impingement and cross-over sign was the measure most often used in pincer type impingement. Studies that reported solely on cam or pincer impingement tended to assess for features of both impingement types to support study exclusions.
DISCUSSION
A key finding of this review is the limited reporting of preoperative assessment and imaging practices in the diagnosis of FAI prior to hip arthroscopy in the literature.
Non-operative treatment prior to hip arthroscopy was highly underreported in the included studies with a mean reported duration of 10 months. Current literature is supportive of non-operative therapy prior to surgical intervention; however, the efficacy of these treatments and their suggested duration is largely unknown [23]. Further, there have been theoretical propositions that early surgical intervention may in fact be more efficacious and prevent the development of future arthritis [23]. Research is currently underway to determine the type and duration of non-operative treatment that is most beneficial [24, 25].
With respect to diagnosis of FAI, FADIR testing was the most reported clinical examination which is known to be highly sensitive (0.99) for FAI/labral pathology though less specific [13, 14]. FABER and impingement sign were used less often which may reflect a relatively decreased sensitivity and specificity [14, 25]. Interestingly, diagnostic injection was a highly underreported component of preoperative assessment (used in 7% of patients) despite a positive response being reported as 90% accurate for detecting intra-articular pathology [24]. Further, response to diagnostic injection has also been shown to be positively associated with surgical outcome and thus, informative to treatment [24]. Within imaging, MRI and CT were reportedly used less often compared to plain radiographic imaging. This pattern in the use of imaging may reflect the increased time required for MRI and increased radiation dose with CT imaging [26, 27]. Within this systematic review, alpha angle >55° was the most reported measure of cam impingement. Current literature, however has suggested an alpha angle cut-off of 57° to maximize sensitivity and specificity for cam impingement [28]. Comparatively, no measure has been found to not be sensitive or specific enough to use in isolation in pincer impingement [29]. Thus, cross-over sign should be considered alongside other measures of pincer impingement [29].
Despite the underreporting of preoperative assessment practices and imaging, some commonalities emerged in the included literature suggestive of not only current practice but also what should be included in the work-up of a patient with suspected FAI. Physical examination should include impingement testing, where FADIR is a highly reported (used in 57% of patients in this study), sensitive and specific measure for intra-articular pathology [13, 14]. Clinical suspicion based on history and physical examination should be corroborated by radiographic imaging where an AP pelvis and Dunn view (45°) should be used to assess for features characteristic of cam and/or pincer impingement [30]. While alpha angle >55° may be used to assess for cam impingement, morphological parameters such as cross-over sign in addition to other features such as coxa profunda and CEA should be used to assess for pincer type [5]. If FAI cannot be appropriately characterized by radiograph and/or if there is suspicion of labral pathology, MRI imaging, preferably MRA, should be considered [31]. Current research suggests that the radial plane should be considered in the MRI investigation of FAI [32]. Additionally, CT, particularly 3 D-CT, should be considered in patients who are not candidates for MRI to recognize subtle femoral deformities and in preoperative planning for the management of complex deformities [17].
Currently, FAI is a diagnostic challenge that relies on patient history, physical examination and imaging findings. However, improved refinement of tools in diagnosis and the potential for concurrent evaluation with biomarkers of cartilage may lead to further diagnostic improvements combined with current modalities [33].
Strengths
This review has several strengths. First, the broad search strategy and inclusion criteria used allowed for the inclusion of many studies and a large sample of patients. Further, review of articles in duplicate at the title, abstract and full text stages was aimed to minimize reviewer bias. In addition, the review captured preoperative assessment for over 5000 patients.
Limitations
This study was limited by the low-quality evidence on this topic as well a lack of gold standard in the literature for use as a comparator to the included studies. This study included English only papers which may also lead to publication bias. Additionally, few included studies reported on the use of both preoperative examination and imaging with several studies not reporting on preoperative examination. Exact imaging measures and how both preoperative physical examination and imaging influenced diagnosis and subsequent clinical decision making was also limited. This study was also not registered with PROSPERO.
Future directions
Future studies on hip arthroscopy should better report preoperative physical examination details/findings and the imaging used including the justification for their use and expected findings. Documentation as to how the diagnosis changed based on preoperative findings and imaging would also help to identify how findings on physical examination and imaging can inform diagnosis. Greater reporting would also assist in improving the current understanding of findings used in the preoperative assessment for hip arthroscopy and what may be most relevant. Improvements in this area may lead to the development of a more consistent validated diagnostic algorithm that would ensure patients are receiving the appropriate diagnosis and subsequent treatment.
CONCLUSIONS
Preoperative assessment prior to FAI arthroscopic surgery was inconsistently reported in the FAI literature and improved reporting is warranted to develop a more consistent validated diagnostic algorithm of FAI.
FUNDING
The authors received no funding for this work.
CONFLICTS OF INTEREST STATEMENT
None declared.
Appendix 1. Outline of systematic search strategy used
Appendix 2.
Characteristics of included studies
| First author, year | Journal | Study design | Level of evidence | Sample size- patients (hips) | % Male | Mean age- years ± SD (range) | % Lost to Follow-up/ excluded post hoc |
|---|---|---|---|---|---|---|---|
| Ayeni, 2011 | J Bone Joint Surg Am | Case Report | 4 | 42 | 100% | 51 | None |
| Bardakos, 2008 | J Bone Joint Surg | Cohort Study | 2 | 71 (71) | 52% | 33 (27–41) | None |
| Basheer, 2016 | Bone Joint J | Case Series | 4 | 18 (19) | 50% | 19 (13–42) | None |
| Berkes, 2012 | Am J Orthop (Belle Mead, NJ) | Case Report | 4 | 3 (3) | 100% | 21 (17–27) | None |
| Boden, 2014 | Acta Orthop Belg | Observational | 4 | 120 (120) | Not reported | Median: 39 (14–67) | None |
| Boykin, 2013 | Knee Surg Sports Traumatol Arthrosc | Case Report | 5 | 1 (1) | 100% | 25 | None |
| Büchler, 2013 | Arthroscopy | Retrospective Comparative | 3 | 201 (201) | 54% | 32.5 | 18% |
| Byrd, 2011 | Arthroscopy | Case Series | 4 | 100 (100) | 67% | 34 (13–67) | None |
| Centinkaya, 2014 | Orthopedics | Case Series | 4 | 2 (2) | 0% | 39.5 (37–42) | None |
| Chahal, 2015 | Am J Sports Med | Cohort Study | 2 | 130 (130) | 42.3% | 35.6 ± 11.7 | None |
| Cloisy, 2010 | J Bone Joint Surg | Case Series | 4 | 35 (35) | 80% | 34 (16–48) | None |
| Dippmann, 2014 | Knee Surg Sports Traumatol Arthrosc | Case Series | 4 | 87 | 37% | 38 (15–63) | 16% |
| Domb, 2013 | Arthroscopy | Matched Comparative Study | 2 | 30 (30) | 20% | Not reported | None |
| Domb, 2014 | Arthroscopy | Case Series | 4 | 43 (47) | 49% | 37 (16–70) | None |
| Fabricant, 2012 | J Bone Joint Surg Am | Case Series | 4 | 21 (27) | 57% | 17.6 (14.5–19.9) | None |
| Fabricant, 2015 | Clin Orthop Relat Res | Prognostic Study | 2 | 243 (243) | 49 % | 29.2 | None |
| Ferro, 2015 | Arthroscopy | Case Series | 4 | 180 (180) | Not reported | 34 | None |
| Frank, 2014 | Am J Sports Med | Cohort Study | 3 | 64 (64) | 38% | 33 | None |
| Fritz, 2010 | Arthroscopy | Case Report | 4 | 2 (2) | 50% | 35 (18–52) | None |
| Fowler, 2010 | Arthroscopy | Case Report | 4 | 1 (1) | 100% | 42 | None |
| Fukui, 2016 | Int J Surg Case Rep | Case Report | 4 | 1 (1) | 100% | 53 | None |
| Gedouin, 2010 | Orthop Traumatol Surg Res | Case Series | 4 | 110 (111) | 71% | 31 (16–49) | None |
| Gupta, 2014 | Am J Sports Med | Case Series | 4 | 47 (47) | 60% | 37.2 (32–47) | None |
| Hammoud, 2012 | Arthroscopy | Case Series | 4 | 38 (38) | 100% | 31 (19–35) | None |
| Hartmann, 2009 | Arch Orthop Trauma Surg | Case Series | 4 | 32 (33) | Not reported | 31.1 (15–47) | 3% |
| Haviv, 2010 | J Bone Joint Surg Br | Case Series | 4 | 166 (170) | 80% | 37 (14–68) | None |
| Haviv, 2010 | Orthopedics | Case Series | 4 | 82 (164) | 82% | 29 (14–63) | None |
| Horisbeger, 2010 | Clin Orthop Relat Res | Case Series | 4 | 19 (19) | 53% | 47.3 (22–65) | 5% |
| Horisberger, 2010 | Arthroscopy | Case Series | 4 | 88 (105) | 70% | 40.9 (17–66) | None |
| Ilizaliturri, 2007 | J Bone Joint Surg Br | Case Series | 4 | 13 (14) | 46% | 30.6 (24–39) | None |
| Ilizaliturri, 2008 | J Arthroplasty | Case Series | 4 | 18 (18) | 56% | 34 (27–43) | None |
| Javed, 2011 | J Bone Joint Surg. | Cohort Study | 3 | 40 (40) | 65% | 65 (60–82) | None |
| Kaya, 2014 | Arthroscopy | Case Series | 4 | 77 (77) | 42% | 47.5 (18–78) | None |
| Kemp, 2014 | Br J Sports Med | Case Series | 4 | 100 | 51% | 36 | None |
| Krekel, 2011 | J Med Case Rep | Case Report | 4 | 1 (1) | 100% | 50 | None |
| Krych, 2013 | Arthroscopy | Randomized Controlled Study | 1 | 36 | 0% | 39 (19–59) | None |
| Larson, 2008 | Arthroscopy | Case Series | 4 | 96 (100) | 56% | 34.7 (16–64) | None |
| Larson, 2011 | Clin Orthop Relat Res | Case Series | 4 | 210 (227) | 59% | 31.8 (14–61) | 29% |
| Larson, 2012 | Am J Sports Med | Cohort | 2 | 90 (94) | 62% | 34 | 7% |
| Laude, 2009 | Clin Orthop Relat Res | Therapeutic Study | 2 | 91 (94) | 52% | 33.4 (16–56) | 6% |
| Leunig, 2012 | Arthroscopy | Case Series | 4 | 141 (152) | Not reported | 77 | None |
| Lincoln, 2009 | Arthroscopy | Case Series | 4 | 14 (16) | 71% | Not reported | 18% |
| Más Martínez, 2015 | Arthroscopy | Case Report | 4 | 1 (1) | 0% | 58 | None |
| Malviya, 2012 | Br J Sports Med | Case Series | 4 | 122 (122) | 61% | 35.4 (16–64) | None |
| Malviya, 2013 | Orthop Relat Res | Case Series | 4 | 80 (80) | 62.5% | 36 (16–59) | None |
| Matsuda, 2013 | Am J Sports Med | Cohort | 3 | 54 | 59% | 34.6 + 37.5 | None |
| Matsuda, 2014 | Arthrosc Tech. | Case Report | 4 | 1 (2) | 100% | 26 | None |
| Mei-Dan, 2014 | Arthroscopy | Retrospective Comparative Study | 3 | 73 (116) | 55% | 33 (18–35) | 4% |
| Nepple, 2009 | J Arthroplasty | Cohort | 2 | 48 (48) | 60% | 37.4 | None |
| Nossa, 2014 | Curr Orthop Pract | Cohort Study | 2 | 362 (362) | 40.6% | 40.4 (15–79) | None |
| Ozturk, 2013 | Arch of Orthop Trauma Surg | Case Report | 4 | 1 (1) | 100% | 45 | None |
| Palmer, 2012 | Arthroscopy | Case Series | 4 | 185 (201) | 53.5% | 40.2 | 4.2% |
| Park, 2013 | Arthrosc Tech | Case Report | 4 | 1 (1) | 100.0% | 45 | None |
| Park, 2014 | Arthrosc Tech | Case Series | 4 | 197 (200) | 49% | 44.64 (19–70) | None |
| Philippon, 2007 | Knee Surg Sports Traumatol Arthrosc | Case Series | 4 | 45 (45) | 93% | 31 (17–61) | None |
| Philippon, 2007 | Knee Surg Sports Traumatol Arthrosc | Case Series | 4 | 301 (301) | 51% | 40 (11–72) | None |
| Philippon, 2008 | J Pediatr Orthop | Case Series | 4 | 16 (16) | 88% | 15 (11–16) | None |
| Philippon, 2012 | Arthroscopy | Case Series | 4 | 107 (107) | Not reported | 57 (50–77) | 30% |
| Philippon, 2014 | J Pediatr Orthop | Case series | 4 | 7 (7) | 57% | 42 ± 8 (28–50) | None |
| Polat, 2013 | Acta Orthop Traumatol Turc | Case Series | 4 | 42 (42) | 60% | 35.1 (16–52) | None |
| Randelli, 2010 | J Orthop Traumatol | Retrospective comparative study | 3 | 300 | 60% | 37.6 | 5% |
| Redmond, 2015 | Am J Sports Med | Cohort | 3 | 174 (190) | 33 | None | |
| Sansone, 2013 | Knee Surg Sports Traumatol Arthrosc | Case Report | 4 | 2 (2) | 50% | 26 | None |
| Sansone, 2015 | Orthop J Sports Med | Case Series | 4 | 85 (115) | 80% | 25 ± 5 | None |
| Sekiya, 2009 | Orthopedics | Case Report | 4 | 1 (2) | 100% | 17 | None |
| Stähelin, 2008 | Arthroscopy | Case Series | 4 | 22 (22) | 68% | 45 (18–67) | None |
| Tran, 2013 | ANZ J Surg | Case Series | 4 | 34 (41) | 85% | 15.7 (11–18) | None |
| Whiting, 2015 | Orthopedics | Case Report | 4 | 1 (1) | 0% | 48 | None |
REFERENCES
- 1. Reich MS, Shannon C, Tsai E. et al. Hip arthroscopy for extra-articular hip disease. Curr Rev Musculoskelet Med 2013; 6: 250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Enseki KR, Martin RL, Draovitch P. et al. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther 2006; 36: 516–25. [DOI] [PubMed] [Google Scholar]
- 3. Bredella MA, Ulbrich EJ, Stoller DW. et al. Femoroacetabular Impingement. Magn Reson Imaging Clin N Am 2013; 21: 45–64. [DOI] [PubMed] [Google Scholar]
- 4. Banerjee P, McLean CR.. Femoroacetabular impingement: a review of diagnosis and management. Curr Rev Musculoskelet Med 2011; 4: 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tannast M, Siebenrock KA, Anderson SE. et al. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AMJ AM J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 6. McCarthy JC, Lee J.. Hip arthroscopy: indications, outcomes, and complications. Instructional Course Lectures 2006; 55: 301. [PubMed] [Google Scholar]
- 7. Boden RA, Wall AP, Fehily MJ.. Results of the learning curve for interventional hip arthroscopy: a prospective study. Acta Orthop Belg 2014; 80: 39–44. [PubMed] [Google Scholar]
- 8. Bogunovic L, Gottlieb M, Pashos G. et al. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res 2013; 471: 2523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tanzer M, Makhdom AM.. Preoperative planning in primary total knee arthroplasty. J Am Acad Orthop Surg 2016; 24: 220–30. [DOI] [PubMed] [Google Scholar]
- 10. Maslowski E, Sullivan W, Forster Harwood J. et al. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. PM R 2010; 2: 174–81. [DOI] [PubMed] [Google Scholar]
- 11. Pacheco-Carrillo A, Medina-Porqueres I.. Physical examination tests for the diagnosis of femoroacetabular impingement: a systematic review. Phys Ther Sport 2016; 21: 87–93. [DOI] [PubMed] [Google Scholar]
- 12. Kuhlman G, Domb B.. Hip impingement: identifying and treating a common cause of hip pain. Am Fam Physician 2009; 80: 1429–34. [PubMed] [Google Scholar]
- 13. Martin RL, Irrgang JJ, Sekiya JK.. The diagnostic accuracy of a clinical examination in determining intra-articular hip pain for potential hip arthroscopy candidates. Arthroscopy 2008; 24: 1013–8. [DOI] [PubMed] [Google Scholar]
- 14. Reiman MP, Goode AP, Cook CE. et al. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: a systematic review with meta-analysis. Br J Sports Med 2015; 49: 811.. [DOI] [PubMed] [Google Scholar]
- 15. Li AE, Jawetz ST, Greditzer HG. et al. MRI for the preoperative evaluation of femoroacetabular impingement. Insights Imaging 2016; 7: 187–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mintz DN, Hooper T, Connell D. et al. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy 2005; 21: 385–93. [DOI] [PubMed] [Google Scholar]
- 17. Heyworth BE, Dolan MM, Nguyen JT. et al. Preoperative three-dimensional CT predicts intraoperative findings in hip arthroscopy. Clin Orthop Relat Res 2012; 470: 1950–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Philippon MJ, Briggs KK, Carlisle JC. et al. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res 2013; 471: 2492–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horner N, de SA D, Heaven S. et al. Indications and outcomes of shoulder arthroscopy after shoulder arthroplasty. J Shoulder Elbow Surg 2016; 25: 510–8. [DOI] [PubMed] [Google Scholar]
- 20. Slim K, Nini E, Forestier D. et al. Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 2003; 73: 712–6. [DOI] [PubMed] [Google Scholar]
- 21. Landis JR, Koch GG.. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. [PubMed] [Google Scholar]
- 22. McGinn T, Wyer PC, Newman TB. et al. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ 2004; 171: 1369–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wall P, Fernandez M, Griffin DR. et al. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R 2013; 5: 418–26. [DOI] [PubMed] [Google Scholar]
- 24. Khan W, Khan M, Alradwan H. et al. Utility of intra-articular hip injections for femoroacetabular impingment: a systematic review. Orthop J Sports Med 2015; 3:23–32.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Palmer AJ, Ayyar-Gupta V, Dutton SJ. et al. Protocol for the Femoroacetabular Impingement Trail (FAIT): a multicentre randomised controlled trial comparing surgical and non-surgical management of femoroacetabular impingement. Bone Joint Res 2014; 3: 321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nepple JJ, Prather H, Trousdale RT. et al. Clinical diagnosis of femoroacetabular impingement. J Am Acad Orthop Surg 2013; 21S: 16–9. [DOI] [PubMed] [Google Scholar]
- 27. Rakhra KS. MRI/CT in FAI In: Marín-Peña Ó. (ed), Femoroacetabular Impingment. Berlin: Spinger, 2012, 41–55. [Google Scholar]
- 28. Barrientos C, Barahoma M, Diax K. et al. Is there a pathological alpha angle for hip impingement? A diagnostic test study. J Hip Preserv Surg 2016; 3: 223–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zaltz I, Kelly BT, Hetsroni I, Bedi A.. The crossover sign overestimates acetabular retroversion. Clin Orthop Related Res 2013; 471: 2463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meyer DC, Beck M, Ellis T. et al. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 2006; 445: 181–5. [DOI] [PubMed] [Google Scholar]
- 31. Toomayan GA, Holman WR, Major NM. et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR AMJ Roentgenol 2006; 186: 449–53. [DOI] [PubMed] [Google Scholar]
- 32. Rakhra KS, Sheikh AM, Allen D, Beaulé PE.. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res 2009; 467: 660–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bedi A, Lynch EB, Sibilski Enselman ER. et al. Elevation in circulating biomarkers of cartilage damage and inflammation in athletes with femoroacetabular impingement. Am J Sports Med 2013; 41: 2585–90. [DOI] [PMC free article] [PubMed] [Google Scholar]


