Figure 2. Microbiota controls hematopoiesis and systemic hematopoietic cell education.
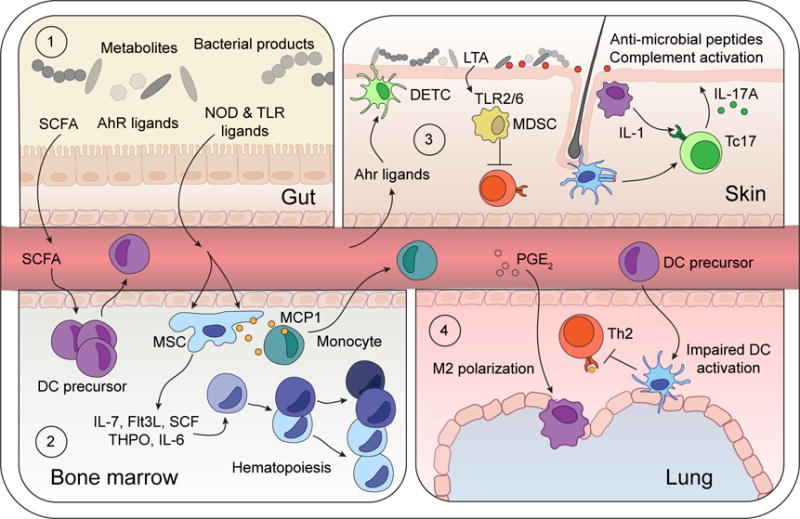
(1) Microbiota-derived TLR and NOD ligands and metabolites (SCFA and AhR ligands) can act directly on local intestinal tissue cells, but also penetrate beyond the mucosa, into circulation to tune immune cells in peripheral tissues.
(2) SCFA promote DC precursor activation and release into bloodstream. Microbiota-derived NOD1 ligands activate mesenchymal stem cells (MSC) to produce hematopoietic growth factors (IL-7, SCF, THPO, Flt3L, IL-6), and commensal-derived TLR ligands trigger MCP1 production by MSC and their progeny, thereby promoting monocyte exit into the bloodstream.
(3) Diet-derived AhR-ligands promote continued tissue residency of Dendritic Epidermal T cells (DETC) within the skin epidermis. Local skin commensals engage local immune responses. Lipoteichoic acid (LTA) derived from S. aureus limits T cell activation by TLR2/6-dependent generation of myeloid-derived suppressor cells (MDSC). Conversely, colonization with S. epidermidis promotes cognate CD8+ T cell seeding of the epidermis, licensing of cytokine production by myeloid-derived IL-1, and engagement of antimicrobial pathways by keratinocytes.
(4) SCFA-elicited DC precursors traffic to the lung and limit Th2 cell reactivation to dampen experimental asthma. Antibiotic-dependent dysbiosis elicits PGE2 production which promotes M2 polarization of alveolar macrophages.
