Abstract
The PREdiction of DELIRium for Intensive Care (PRE-DELIRIC) model reliably predicts at 24 h the development of delirium during intensive care admission. However, the model does not take account of alcohol misuse, which has a high prevalence in Scottish intensive care patients. We used the PRE-DELIRIC model to calculate the risk of delirium for patients in our ICU from May to July 2013. These patients were screened for delirium on each day of their ICU stay using the Confusion Assessment Method for ICU (CAM-ICU). Outcomes were ascertained from the national ICU database. In the 39 patients screened daily, the risk of delirium given by the PRE-DELIRIC model was positively associated with prevalence of delirium, length of ICU stay and mortality. The PRE-DELIRIC model can therefore be usefully applied to a Scottish cohort with a high prevalence of substance misuse, allowing preventive measures to be targeted.
Keywords: Delirium, alcohol abuse, decision support techniques, prophylaxis
Introduction
Delirium is a clinical syndrome characterised by acute disturbance in awareness, inattention and cognitive dysfunction. It is prevalent in critical care, affecting up to 80% of ventilated patients,1 and independently predicts mortality, longer stays and higher costs.2,3 It has also been associated with persistent cognitive impairment in intensive care unit (ICU) survivors.4
Identifying and treating ICU delirium is imperative as a means of alleviating patient distress in the short term and potentially mitigating adverse outcomes in the longer term. Of the tools available for detecting delirium in intensive care patients, the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) has the highest sensitivity and specificity.5
More recently, models have been developed to predict the likelihood of a patient developing delirium. Such models enable targeted assessment of high risk patients, but also create opportunity for preventing delirium, which has been shown possible outwith the ICU.6,7 The PREdiction of DELIRium for Intensive Care (PRE-DELIRIC) model8 was the first model validated in unselected general intensive care patients. It reliably predicts the development of delirium on the basis of 10 readily available risk factors within 24 h of intensive care admission. These risk factors (in order of greatest weighting) are coma, admission category (surgical, medical, trauma or neurosurgical), sedative use, infection, morphine use, unplanned ICU admission, metabolic acidosis, APACHE-II score, age and urea.
However, the PRE-DELIRIC model does not take account of substance misuse, which strongly predisposes delirium.9 The model’s proponents excluded alcohol abuse as a risk factor on account of its low prevalence in the initial study population.8 They have subsequently defended this approach by stating that the incidence of ICU delirium in alcohol abusers is so high as to render a prediction tool redundant. We therefore sought to determine whether the PRE-DELIRIC model retained its utility in a west of Scotland cohort with prevalent alcohol abuse.
Methods
This was a prospective cohort study of patients admitted to the general intensive care unit of Monklands District General Hospital in the west of Scotland between May and July 2013.
The risk of each patient developing delirium was calculated using the PRE-DELIRIC model (Radboud University Nijmegen Medical Centre). All data needed to use this model were harvested from patient records by the first and second authors. Where alfentanil was used for anlagosedation, this was converted to an equipotent dose of morphine.
To diagnose delirium, intensive care nurses (without knowledge of PRE-DELIRIC findings) assessed patients using the CAM-ICU at least once daily. This frequency of screening reflects standard practice in our unit, where the staff undergo multifaceted training and regular monitoring in the performance of the CAM-ICU. Patients were defined as having delirium if they had at least one positive CAM-ICU result during their intensive care stay. They were excluded from analyses if they were CAM-ICU positive within 24 h or not assessed for delirium on a daily basis.
ICU length of stay and mortality were ascertained from WardWatcher (the Scottish intensive care episode database) and the data analysed with Microsoft Excel software. Ethics approval was not required as delirium assessment is routinely performed and all other data routinely collected in our unit.
Results
Forty-four patients were admitted to our ICU during the study period. The characteristics of the cohort are shown in Table 1.
Table 1.
Patient characteristics.
| Median (IQR) age in years | 60 (43–67) |
| Male sex | 30 (68.2%) |
| Alcohol and/or drug misuse | 14 (31.8%) |
| Median (IQR) APACHE-II score | 17.5 (13–26) |
| Urgent admission | 41 (93.2%) |
| Admission category: | |
| Surgery | 21 (47.8%) |
| Medical | 18 (40.9%) |
| Trauma | 4 (9.1%) |
| Neurosurgery | 1 (2.3%) |
| Mechanical ventilation | 37 (84.1%) |
| Median (IQR) ICU length of stay in days | 2 (1–4) |
| ICU mortality | 9 (20.5%) |
Note: Values are number (percentage) of patients unless otherwise specified. IQR, interquartile range.
Fourteen patients were known to abuse alcohol or drugs. Eleven (78.6%) of these patients were males and all had unplanned admissions to ICU with a median APACHE-II score of 15 (IQR 11–23). Twelve (85.7%) were ventilated and 13 (92.9%) were discharged alive from ICU at a median of three (IQR 1–7) days.
Five patients (11.3%) were not assessed for delirium on a daily basis and seven (15.9%) could not be screened due to persistent coma (Richmond Agitation-Sedation Scale10 −4 or −5 throughout the ICU admission). Of the remaining 32 patients, 15 (46.9%) were delirious during their ICU stay. There were 13 substance misusers with complete delirium screening, of whom seven (53.8%) were CAM-ICU positive.
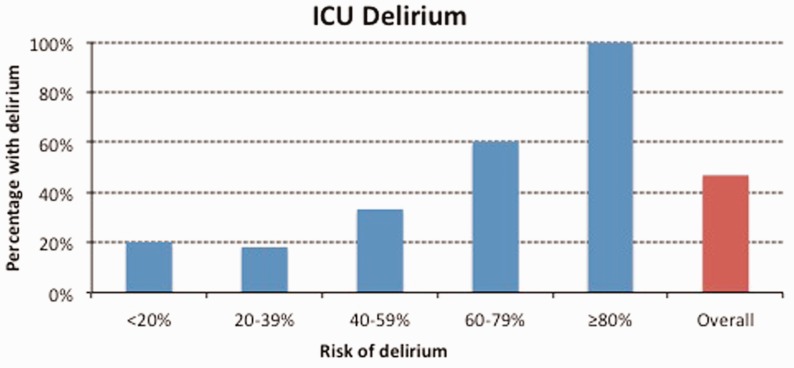
In keeping with the original description of the model,8 we divided our patients into five risk strata, based on PRE-DELIRIC scores of <20%, 20–39%, 40–59%, 60–79% and ≥80%. The incidence of delirium by risk strata is shown in Figure 1.
Figure 1.
Relationship between PRE-DELIRIC score for risk of ICU delirium and actual incidence of ICU delirium.
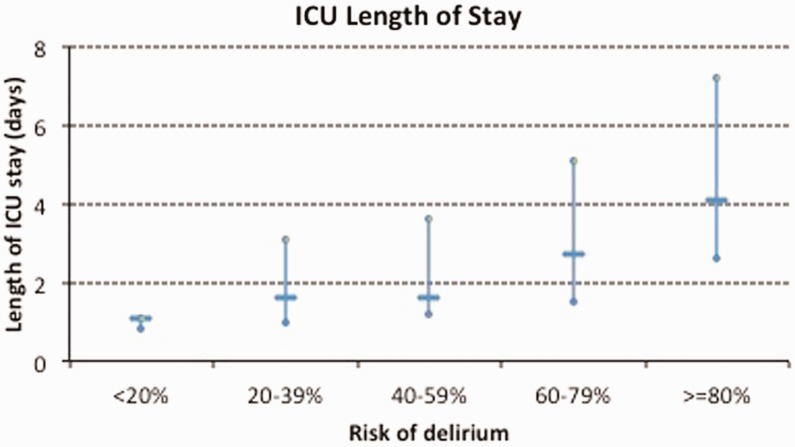
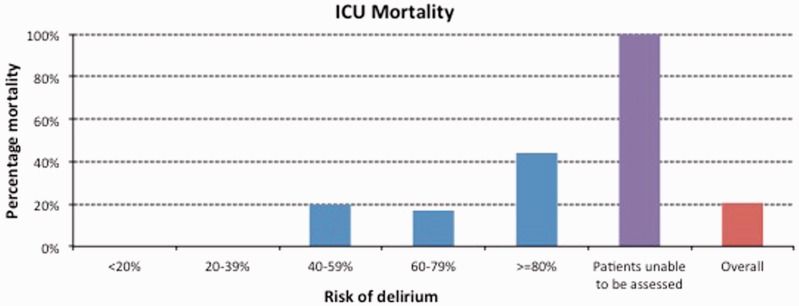
The risk of delirium given by the PRE-DELIRIC model was also positively associated with length of ICU stay (Figure 2) and mortality (Figure 3).
Figure 2.
Relationship between PRE-DELIRIC score for risk of ICU delirium and length of ICU stay. Horizontal bars reflect medians and vertical bars interquartile ranges.
Figure 3.
Relationship between PRE-DELIRIC score for risk of ICU delirium and ICU mortality.
Patients unable to be screened for delirium due to persistent coma had a mortality of 100%.
Discussion
The PRE-DELIRIC model reliably predicts the development of ICU delirium based on ten risk factors assessed in the first 24 h of admission to intensive care.8 It was originally derived and validated in the Netherlands, where it was shown to outperform prediction of delirium by caregivers. A subsequent multinational study11 showed that the model had similar discriminative power when applied to ICU cohorts across Europe and Australia.
One criticism of the PRE-DELIRIC model12 is that it does not account for alcohol misuse as a recognised risk factor for ICU delirium, which potentially impacts its generalisability. Van den Boogaard et al.8 justified the omission of alcohol misuse from the initial multivariate regression analysis by citing its ‘low prevalence rate’ (7.8%) and their perception that its inclusion would ‘decrease the model’s sensitivity to other covariates’.
In Scotland, more than a quarter of ICU admissions are alcohol-related.13 However, our study shows that the PRE-DELIRIC model retains its utility, both in terms of predicting the development of delirium and also as a more generalised severity score that is positively associated with both ICU length of stay and mortality. Previous analyses11 have cautioned that the PRE-DELIRIC model may overestimate ICU delirium in patient populations with a high probability of delirium, such as might be associated with prevalent alcohol misuse. This did not appear to be the case among our patients with a predicted risk of delirium ≥80%, all of whom developed ICU delirium.
Where our findings did concur with previous data2 was in the 100% mortality among patients unable to be assessed for delirium due to persistent coma. Hence, while ICU delirium negatively impacts patient outcomes, inability to assess for delirium is associated with a worse prognosis, likely conferred by clinical scenarios in which pathology and/or pharmacology sustains coma.
Clinical relevance
The PRE-DELIRIC model may confer clinical benefit in permitting targeted deployment of prophylactic measures in patients found to be at high risk of ICU delirium. Non-pharmacologic interventions shown to prevent delirium include early mobilisation,14 sleep enhancement15 and avoidance of deliriogenic medications.16,17 The risk:benefit ratio of drug interventions is less clearly defined. Several studies suggest that haloperidol may prevent delirium in elderly post-operative patients7,18 but there is currently no evidence for prophylactic administration of any antipsychotic in the broader population of critically ill patients.19
One possible explanation for previous studies failing to demonstrate a benefit of prophylactic antipsychotics is that wholesale administration of these agents exposes patients at low likelihood of developing delirium (and thus benefitting from treatment) to drug toxicity. Using the PRE-DELIRIC model to identify patients at high risk of developing delirium may allow efficient use of research resources and better reveal the effects of preventive measures.
A pre- and post-intervention study has shown some promise in this regard.20 Prophylactic treatment with haloperidol in ICU patients with a high risk for delirium (PRE-DELIRIC score >50%) yielded lower delirium incidence, more delirium free days and improved survival when compared with the historical control group. Patients at higher risk of delirium had greater benefit with haloperidol prophylaxis. Clearly, better quality evidence is required and a multicentre randomised controlled trial of prophylactic haloperidol in ICU patients (with post hoc analysis based on the PRE-DELIRIC score) is planned.21
Limitations
The major limitations of our study are the small cohort and lack of statistical analyses to quantify the likelihood of the observed results being due to chance alone. We also accept that the incidence of ICU delirium may be underestimated by once daily CAM-ICU screening, given its fluctuating course. However, we sought to preserve the generalisability of this study by altering neither attitudes to nor monitoring of delirium. Moreover, our diagnosis of delirium was based on daily CAM-ICU performance (with insufficiently frequent assessment being grounds for exclusion), thereby increasing the sensitivity of this test. Another confounder may be the prevention or treatment of alcohol withdrawal modifying delirium rates in our cohort.
Like any model, PRE-DELIRIC has its shortfalls. In the initial analysis,8 the negative likelihood ratio for patients with a PREDELIRIC score ≤20% was moderate at 0.26. This means that some patients predicted to be at low risk of ICU delirium will develop the condition, as can be seen from our results. However, routine screening for ICU delirium, in accordance with current guidelines,22 will identify these patients.
Moving forward, the PRE-DELIRIC model will likely require revalidation (and potentially recalibration) as intensive care evolves. For example, changes in analgosedation practice may impact the incidence of delirium and thus the performance of the model. Van den Boogaard et al.8 have also highlighted that PRE-DELIRIC scores are calculated at a single point in time early in the ICU admission and fail to account for changes in illness severity during the ICU stay. They postulate that a dynamic delirium prediction model, akin to the Sequential Organ Failure Assessment (SOFA) score,23 would offer superior performance and clinical utility.
Conclusions
The PRE-DELIRIC model can be usefully applied to a Scottish cohort with a high prevalence of substance misuse. It predicts the development of delirium, length of ICU stay and mortality at an early stage, allowing preventive measures to be targeted.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Ely EW, Inouye SK, Benard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA 2001; 286: 2703–2710. [DOI] [PubMed] [Google Scholar]
- 2.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 2004; 291: 1753–1762. [DOI] [PubMed] [Google Scholar]
- 3.Milbrandt EB, Deppen S, Harrison PL, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care 2004; 32: 955–962. [DOI] [PubMed] [Google Scholar]
- 4.Pandharipande PP, Girard TD, Jackson JC, et al. for the BRAIN-ICU Study investigators: long-term cognitive impairment after critical illness. N Engl J Med 2013; 369: 1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luetz A, Heymann A, Radtke FM, et al. Different assessment tools for intensive care unit delirium: which score to use? Crit Care Med 2010; 38: 409–418. [DOI] [PubMed] [Google Scholar]
- 6.Inouye SK, Bogardus ST, Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999; 340: 669–676. [DOI] [PubMed] [Google Scholar]
- 7.Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc 2005; 53: 1658–1666. [DOI] [PubMed] [Google Scholar]
- 8.van den Boogaard M, Pickkers P, Slooter AJC, et al. Development and validation of PRE-DELIRIC delirium prediction model for intensive care patients. BMJ 2012; 344: e420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ouimet S, Kavanagh BP, Gottfried SB, et al. Incidence, risk factors and consequences of ICU delirium. Intens Care Med 2007; 33: 66–73. [DOI] [PubMed] [Google Scholar]
- 10.Sessler CN, Gosnell M, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care patients. Am J Respir Crit Care Med 2002; 166: 1338–1344. [DOI] [PubMed] [Google Scholar]
- 11.Van den Boogaard M, Schoonhoven L, Maseda E, et al. Recalibration of the delirium prediction model for ICU patients (PRE-DELIRIC): a multinational observational study. Intens Care Med 2014; 40: 361–369. [DOI] [PubMed] [Google Scholar]
- 12.Prabhakaran S. Re: Development and validation of PRE-DELIRIC delirium prediction model for intensive care patients. BMJ. www.bmj.com/content/344/bmj.e420/rr/570168. (2012, accessed 29 May 2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geary T, O’Brien P, Ramsay S, et al. A national service evaluation of the impact of alcohol on admission to Scottish intensive care units. Anaesthesia 2012; 67: 1132–1137. [DOI] [PubMed] [Google Scholar]
- 14.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009; 373: 1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Rompaey B, Elseviers MM, Van Drom W, et al. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care 2012; 16: R73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pandharipande PP, Pun BT, Herr DL, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 2007; 298: 2644–2653. [DOI] [PubMed] [Google Scholar]
- 17.Riker RR, Shehabi Y, Bokesch PM, et al. for the SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009; 301: 489–499. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Li HL, Wang DX, et al. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial. Crit Care Med 2012; 40: 731–739. [DOI] [PubMed] [Google Scholar]
- 19.Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med 2013; 1: 515–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van den Boogaard M, Schoonhoven L, van Achterberg, et al. Haloperidol prophylaxis in critically ill patients with a high risk of delirium. Crit Care 2013; 17: R9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van den Boogaard M, Slooter AJ, Bruggemann RJ, et al. Prevention of ICU delirium and delirium-related outcome with haloperidol: a study protocol for a multicenter randomized controlled trial. Trials 2013; 14: 400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation and delirium in adult patients in the Intensive Care Unit. Crit Care Med 2013; 41: 263–306. [DOI] [PubMed] [Google Scholar]
- 23.Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 1998; 26: 1793–1800. [DOI] [PubMed] [Google Scholar]