Highlights
-
•
Locally advanced pancreas cancer (LAPC) has minimal options for local control.
-
•
Irreversible electroporation (IRE) can potentially improve local control for LAPC.
-
•
We present a case of IRE with literature review and risks and benefits of IRE.
-
•
Future studies are needed to clarify which patients may benefit most from IRE.
Keywords: Pancreatic neoplasms, Ablation techniques, Electroporation
Abstract
Introduction
For patients with pancreatic adenocarcinoma who are not candidates for surgical resection, long-term survival is poor, even with currently available systemic and radiation therapy options. However, for those with locally advanced disease who do not have distant metastasis, locoregional control of the tumor has the potential to improve long-term outcomes. A newly developed technology, irreversible electroporation, has advantages over traditional thermal ablation with unresectable cancers in this location.
Presentation of case
In our case report, we describe the first patient treated with irreversible electroporation at our institution for locally advanced pancreatic cancer. The patient is a 63-year-old man who had a partial response to standard chemotherapy and radiation, but was found on operative assessment to have persistently unresectable disease. He therefore underwent irreversible electroporation to the pancreatic mass. His postoperative course was complicated by delayed gastric emptying and wound infection. Three months after surgery, he had no evidence of distant or recurrent disease.
Discussion
Irreversible electroporation for locally advanced pancreatic cancer is an emerging technique which attempts to improve local control of locally advanced, non-metastatic pancreatic cancer. Early data have demonstrated the potential for improved long-term survival in these patients, although further studies are needed to confirm safety and efficacy of this technique.
Conclusion
While there is a positive outlook for the use of irreversible electroporation for locally advanced pancreas cancer, there remain some uncertainties surrounding this therapy, which underscores the importance of future research in this area.
1. Introduction
Locally advanced pancreatic cancer represents 40%–50% of new pancreatic cancer diagnoses, although prognosis is dismal [1], [2]. In these patients, the 5-year survival rate is 5% and overall survival ranges from 8 to 16 months [2]. For unresectable patients, ablation is an alternative therapy for local control, which causes local destruction while ideally avoiding injury to surrounding healthy tissue [3]. However, the pancreas is adjacent to several vital structures, which are vulnerable to injury from ablation. In addition, the significant vasculature around the pancreas can limit the success of ablation through a “heat sink,” preventing the tumor from reaching the temperature needed for appropriate ablation [3]. Irreversible electroporation (IRE) is an emerging therapy that avoids these drawbacks and has shown promise in recent years for the treatment of locally advanced pancreatic cancer. IRE functions through electropermeabilization, by which electric pulses delivered through probes into the tissue create small holes in the cell membrane, known as nanopores. This ultimately results in cell death due to the inability to maintain homeostasis, though maintaining the cell structure. In contrast to thermal ablation, there is no heat sink or transitional zone of partially treated cells [3].
Here, we present a case report of the first patient treated at Moffitt Cancer Center with this technique to target non-metastatic, locally advanced pancreatic cancer that was otherwise unresectable. This case report is compliant with the SCARE guidelines [4].
2. Presentation of case
The patient, a 63-year-old healthy man, underwent a computed tomography (CT) scan for assessment of back pain, which identified a mass in the neck of the pancreas. In retrospect, the patient also noted a 10 pound weight loss over the prior month, but he was otherwise asymptomatic. He had no known risk factors for pancreatic cancer.
Pancreatic protocol CT identified a 5.4 × 4.5 cm mass in the neck of the pancreas with encasement of the common hepatic artery and narrowing of the confluence of the portal vein and superior mesenteric vein, confirmed on endoscopic ultrasound. CT chest showed indeterminate lung nodules, though not avid on positron emission tomography. Endoscopic retrograde cholangiopancreatography demonstrated a 1-cm stricture in the common bile duct, for which a covered metal stent was placed, and biopsy of the mass demonstrated pancreatic adenocarcinoma. CA 19-9 was elevated at 1079.
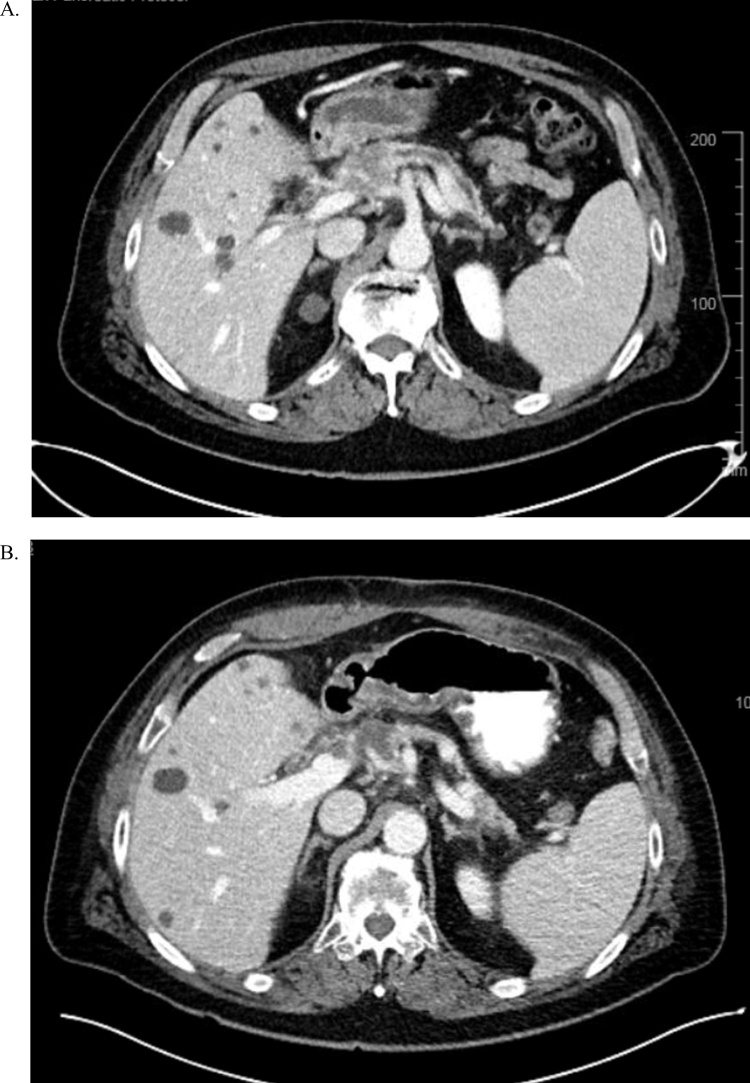
For his locally advanced pancreas cancer, he was started on systemic chemotherapy with FOLFIRINOX for 6 cycles, followed by stereotactic beam radiotherapy. He had a good response, with decrease in size of the tumor and no evidence of new lesions (Fig. 1). CA 19-9 decreased to 71. Multidisciplinary tumor board then recommended consideration of surgery due to his good therapeutic response, young age, and good performance status.
Fig. 1.
Computed tomography scans demonstrating the patient’s unresectable pancreatic cancer. A. Tumor after systemic chemotherapy and radiation therapy but prior to electroporation. B. Tumor after irreversible electroporation.
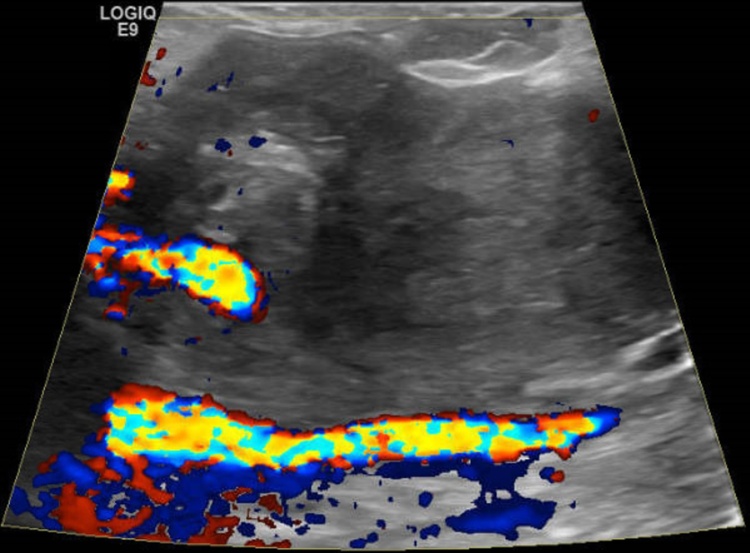
Staging laparoscopy identified no distant metastases. Laparotomy and intraoperative ultrasonography confirmed that the mass was still unresectable, as both the common hepatic artery and portal vein were involved by tumor (Fig. 2). IRE was then performed with NanoKnife® (Angiodynamics). As there is limited long-term follow-up in the use of IRE for locally advanced pancreatic cancer, a gastrojejunal bypass was performed to prevent potential future complications from disease progression. A hepaticojejunal bypass was attempted, but radiation therapy and inflammation from the bile duct stent had resulted in significant fibrosis, precluding safe dissection of the bile duct itself.
Fig. 2.
Ultrasonography image of unresectable pancreatic cancer encasing the hepatic artery and involving the portal vein.
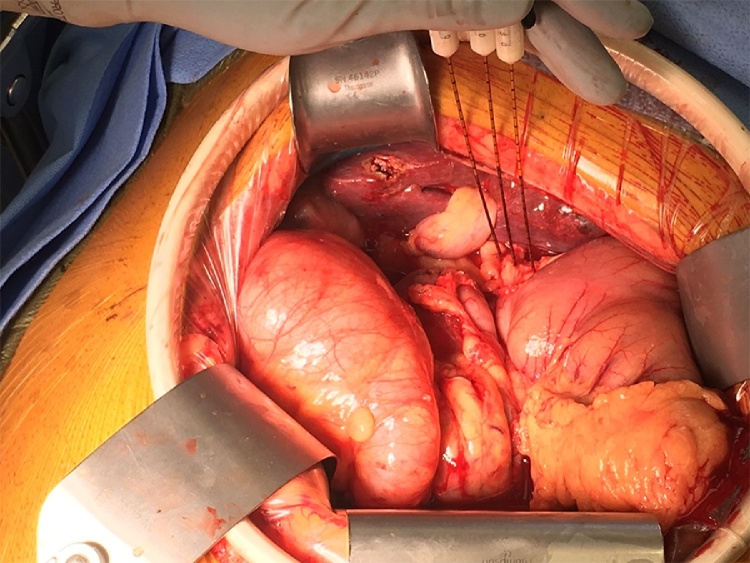
For IRE, manufacturer’s specifications and recommended parameters were followed. [3] Three monopolar electrodes, in linear or triangular configurations, were used to treat sequential parts of the tumor over 4 applications (Fig. 3). The probes were spaced from 0.7 to 1.4 cm apart, and 1.5 cm of the probe tip length was exposed. Eighty pulses were delivered between each probe for each application, and voltage ranged from 1050 to 2100 V/cm. The pulse length was maintained at 90 μs. Ultrasound was performed on the ass again, revealing post-ablation changes of increased echogenicity in the ablation zone and patent vessels (Fig. 4).
Fig. 3.
Intraoperative placement of probes for irreversible electroporation.
Fig. 4.
Ultrasonography image depicting post-ablation changes in the pancreatic mass.
The patient’s postoperative course was complicated by delayed gastric emptying, requiring a week of home supplemental total parenteral nutrition; migration of his biliary stent, requiring endoscopic removal; and a wound infection, requiring wound care. There was no long-term complication from the IRE procedure. At his postoperative visit 3 weeks after surgery, his CA 19-9 remained low at 67. Restaging CT scans at 2 months demonstrated no evidence of metastasis (Fig. 1). He has since recommenced systemic chemotherapy with gemcitabine, which he is tolerating. At 3 months after the procedure, he remains without evidence of disease.
3. Discussion
Beyond systemic therapy, patients with locally advanced pancreatic cancer have limited treatment options. However, if local tumor control can be achieved in patients without distant metastasis, there is potential for improvement in long-term outcomes, or, at a minimum, for disease progression to be slowed or halted [5]. Hence, radiation and ablative techniques have been utilized in an attempt to provide local control in these patients. Stereotactic beam radiotherapy delivers focused beams of radiation to tumors, although with minimal improvements in long-term survival and with significant toxicity [6]. The use of local thermal ablative therapies is limited in pancreatic cancer due to the significant surrounding vasculature, which prevents the ability to reach the high temperatures needed for ablation [6]. Therefore, palliation in these patients is often limited to techniques to provide symptomatic palliation, including surgical bypasses or nerve blocks [6].
IRE has gained popularity for the treatment of multiple solid organ malignancies, including liver, kidney, prostate, bone, and locally advanced pancreatic tumors [3], [7]. Its advantages over thermal modalities include an absence of a heat sink and less potential injury to adjacent vital structures. These factors informed the decision to use IRE to treat a patient with unresectable pancreatic cancer for the first time at Moffitt Cancer Center.
Recently, an international panel was convened to create recommendations for the standardization of pancreatic cancer patients to whom IRE may be offered [8]. Recommendations include preoperative work-up with pancreatic protocol CT or magnetic resonance imaging (MRI) and CA 19-9 levels. Systemic therapy (gemcitabine- or FOLFIRINOX-based) should be given to test the biology of the tumor and to ensure no metastases develop while on chemotherapy. Radiation may be considered after chemotherapy. After completion of therapy, open IRE is recommended, allowing for confirmation of resectability status and no evidence of metastases [9]. The open approach also allows for precise probe placement under ultrasound guidance, and limits injury to adjacent structures. IRE is not recommended when tumors measure over 4 cm after systemic therapy due to limitations of the equipment [8]. Following a tissue conductivity test, IRE can be performed [8]. Of note, metal present within the field of IRE is associated with a risk of thermal injury and incomplete ablation, and as such metal stents should be exchanged for plastic stents preoperatively, or hepaticojejunostomy should be performed with removal of the stent [8], [10], [11]. When IRE is administered in close proximity to the heart, it is important to synchronize the electrical pulsations of IRE with the R wave on an electrocardiogram to avoid cardiac arrhythmias [12], [13]. After IRE has been completed, surveillance of the tumor is recommended at 3-month intervals [8].
Data on short- and long-term results after use of IRE are favorable. In a 2014 systematic review of 4 studies reporting on the use of IRE to treat 74 patients with advanced pancreatic cancer [11], morbidity, including bile and pancreatic leak, portal vein thrombosis, bleeding, pancreatitis, and ileus, ranged from 0% to 33%. However, the causes of morbidity were unclear, as several patients had undergone multiple procedures, such as an intestinal bypass, at the time of the IRE. In a prospective, multi-institutional study examining long-term outcomes after IRE in patients with unresectable pancreatic cancer [2], propensity matching showed improved outcomes with IRE versus those shown without IRE. Progression-free survival (14 months versus 6 months) and overall survival (20 months versus 11 months) were both improved [2]. However, the survival curves converged at 20 months, likely due to the development of distant disease despite treatment. In a more recent multicenter registry study describing patients undergoing IRE alone or as a margin-enhancement where there was concern for a positive resection margin [14], morbidity rates were similarly elevated at 37%. There was a 2% 90-day mortality rate in patients who underwent IRE alone, and median overall survival was encouraging at 23 months – a substantial improvement over historical reports [1].
4. Conclusion
Irreversible electroporation is a relatively new technique that has shown promise in the treatment of well-selected patients with locally advanced pancreatic cancer. However, it is not yet clear whether the improvements in long-term outcomes are durable and due to the IRE or, instead, due to recent improvements in systemic therapy, which is critical to understand due to the significant risk of morbidity with IRE that could delay receipt of systemic therapy. As such, providers are advised to collaborate in prospective patient registries [15] or perform these procedures as parts of clinical trials [1]. In this vein, the Departments of Gastrointestinal Surgery and Interventional Radiology at Moffitt Cancer Center are currently collaborating to create a formal protocol to better clarify these questions in a prospective fashion, with the aim of offering more treatment options for patients with locally advanced pancreatic cancer.
Conflict of interest
The authors declare no conflict of interest and have no acknowledgements.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Our institution does not require institutional review board or other approval for small-volume case series which are deidentified and collected retrospectively (University of South Florida IRB policy #311 allows for the unique reporting of 3 patients or less without IRB approval).
Consent
Written informed consent was obtained from the patient for this study. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. Institutional review board approval or ethics committee approval was not required as per institutional policy, as this was a retrospective de-identified case report.
Authors contribution
Conception or design of work: Orcutt, Malafa.
Acquisition, analysis, or interpretation of data for the work: Orcutt, Kis, Malafa.
Drafting the work or revising it critically for important intellectual content: Orcutt, Kis, Malafa.
Final approval of the version to be published: Orcutt, Kis, Malafa.
Agreement to be accountable for all aspects of the work: Orcutt, Kis, Malafa.
Guarantor
Mokenge Malafa MD.
Acknowledgement
None.
Contributor Information
Sonia Orcutt, Email: Sonia.Orcutt@moffitt.org.
Bela Kis, Email: Bela.Kis@moffitt.org.
Mokenge Malafa, Email: Mokenge.Malafa@moffitt.org.
References
- 1.Jenks S. Shock therapy for late-stage pancreatic cancer gets closer look. J. Natl. Cancer Inst. 2016;108:djw159. doi: 10.1093/jnci/djw159. [DOI] [PubMed] [Google Scholar]
- 2.Martin R.C., 2nd, McFarland K., Ellis S., Velanovich V. Irreversible electroporation in locally advanced pancreatic cancer: potential improved overall survival. Ann. Surg. Oncol. 2013;20(Suppl. 3):S443–S449. doi: 10.1245/s10434-012-2736-1. [DOI] [PubMed] [Google Scholar]
- 3.Wagstaff P.G., Buijs M., van den Bos W., de Bruin D.M., Zondervan P.J., de la Rosette J.J. Irreversible electroporation: state of the art. OncoTargets Ther. 2016;9:2437–2446. doi: 10.2147/OTT.S88086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Paiella S., Salvia R., Ramera M., Girelli R., Frigerio I., Giardino A. Local ablative strategies for ductal pancreatic cancer (radiofrequency ablation, irreversible electroporation): a review. Gastroenterol. Res. Pract. 2016;2016:4508376. doi: 10.1155/2016/4508376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin R.C., 2nd Management of locally advanced pancreatic cancer. Surg. Clin. N. Am. 2016;96:1371–1389. doi: 10.1016/j.suc.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Steinbrecher K., Arslan B., Nassin M.L., Kent P. Irreversible electroporation in the curative treatment of Ewing’s sarcoma. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-216585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin R.C., 2nd, 2nd Durham A.N., Besselink M.G., Iannitti D., Weiss M.J., Wolfgang C.L. Irreversible electroporation in locally advanced pancreatic cancer: a call for standardization of energy delivery. J. Surg. Oncol. 2016;114:865–871. doi: 10.1002/jso.24404. [DOI] [PubMed] [Google Scholar]
- 9.Martin R.C., 2nd Irreversible electroporation of locally advanced pancreatic neck/body adenocarcinoma. J. Gastrointest. Oncol. 2015;6:329–335. doi: 10.3978/j.issn.2078-6891.2015.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheffer H.J., Vogel J.A., van den Bos W., Neal R.E., 2nd, van Lienden K.P., Besselink M.G. The influence of a metal stent on the distribution of thermal energy during irreversible electroporation. PLoS One. 2016;11:e0148457. doi: 10.1371/journal.pone.0148457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moir J., White S.A., French J.J., Littler P., Manas D.M. Systematic review of irreversible electroporation in the treatment of advanced pancreatic cancer. Eur. J. Surg. Oncol. 2014;40:1598–1604. doi: 10.1016/j.ejso.2014.08.480. [DOI] [PubMed] [Google Scholar]
- 12.Thomson K.R., Cheung W., Ellis S.J., Federman D., Kavnoudias H., Loader-Oliver D. Investigation of the safety of irreversible electroporation in humans. J. Vasc. Interv. Radiol. 2011;22:611–621. doi: 10.1016/j.jvir.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 13.Deodhar A., Dickfeld T., Single G.W., Hamilton W.C., Jr., Thornton R.H., Sofocleous C.T. Irreversible electroporation near the heart: ventricular arrhythmias can be prevented with ECG synchronization. Am. J. Roentgenol. 2011;196:W330–335. doi: 10.2214/AJR.10.4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin R.C., 2nd, Kwon D., Chalikonda S., Sellers M., Kotz E., Scoggins C. Treatment of 200 locally advanced (stage III) pancreatic adenocarcinoma patients with irreversible electroporation: safety and efficacy. Ann. Surg. 2015;262:486–494. doi: 10.1097/SLA.0000000000001441. discussion 492–484. [DOI] [PubMed] [Google Scholar]
- 15.Martin R.C. An update on the role of irreversible electroporation in locally advanced pancreatic adenocarcinoma. HPB (Oxford) 2016;18:791–792. doi: 10.1016/j.hpb.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]