Abstract
Tai Chi mind-body exercise is widely believed to improve mindfulness through incorporating meditative states into physical movements. A growing number of studies indicate that Tai Chi may improve health in knee osteoarthritis (OA), a chronic pain disease and a primary cause of global disability. However, little is known about the contribution of mindfulness to treatment effect of Tai Chi practice. Therefore, our purpose was to investigate the effect of Tai Chi mind-body practice compared to physical therapy (PT) on mindfulness in knee OA. Adults with radiographic-confirmed, symptomatic knee OA were randomized to either 12 weeks (twice weekly) of Tai Chi or PT. Participants completed the Five Facet Mindfulness Questionnaire (FFMQ) before and after intervention along with commonly-used patient-reported outcomes for pain, physical function, and other health-related outcomes. Among 86 participants (74% female, 48% white, mean age 60 years, 85% at least college educated), mean total FFMQ was 142±17. Despite substantial improvements in pain, function, and other health-related outcomes, each treatment group’s total FFMQ did not significantly change from baseline (Tai Chi= 0.76, 95% CI: −2.93, 4.45; PT= 1.80, 95% CI: −2.33, 5.93). The difference in total FFMQ between Tai Chi and PT was not significant (−1.04 points, 95% CI: −6.48, 4.39). Mindfulness did not change after Tai Chi or PT intervention in knee OA, which suggests that Tai Chi may not improve health in knee OA through cultivating mindfulness. Further study is needed to identify underlying mechanisms of effective mind-body interventions among people with knee OA.
Keywords: Tai Chi, Osteoarthritis, Mindfulness, Mind-body, Mechanism, Chronic Pain
INTRODUCTION
Mindfulness refers to both the ability to maintain a heightened awareness of one’s moment-to-moment experiences without judging or reacting as well as the approaches and practices used to learn and develop this skill (Kabat-zinn, Lipworth, & Burney, 1985). While mindfulness was historically cultivated through sitting meditation, standardized multi-modal methods of training mindfulness, such as Mindfulness-based Cognitive Therapy (MBCT) and Mindfulness-based Stress Reduction (MBSR) have since been developed to treat or alleviate a variety of mental and physical symptoms and conditions (Petersen & la Cour, 2016; Visted, Vollestad, Nielsen, & Nielsen, 2015). Both MBSR and MBCT are group-based therapies which teach mindfulness skills through a range of formal and informal mindfulness practices, including mindfulness of breath, thoughts, bodily sensations, sounds, and everyday activities (Gu, Strauss, Bond, & Cavanagh, 2015). Movement-based practices, such as Tai Chi, Yoga, and Qigong, are also widely believed to improve mindfulness through incorporating meditative states into physical movements (Chen, Hunt, Campbell, Peill, & Reid, 2015; Kelley & Kelley, 2015; Posadzki & Jacques, 2009; Wayne & Kaptchuk, 2008). Tai Chi is a traditional Chinese mind-body practice that involves slow movements (i.e. movement of the body trunk and upper and lower limbs so as to form various postures systematically following one another), deep breathing, and relaxation. Current research describes Tai Chi as being unique from traditional physical exercise in its mind-body or “mindful” components. One central concept of Tai Chi is concentration or focus, which can be directed internally or externally, and involves the mind becoming unified in its purpose over a period of time (Wayne & Kaptchuk, 2008).
Despite being referred to as a “moving meditation” or “mindful exercise” (National Center for Complementary and Integrative Health, 2015; Posadzki & Jacques, 2009), empirical evidence demonstrating increased mindfulness from Tai Chi practice is scarce. A study among college students found that a Tai Chi course increased mindfulness more than a course of physical recreation but was limited by its non-randomized study design (Caldwell, Emery, Harrison, & Greeson, 2011). A randomized clinical trial among healthy adults found that Tai Chi improved mindfulness compared to a wait-list control but was limited by the absence of an active comparison group (Nedeljkovic, Wirtz, & Ausfeld-Hafter, 2012). To date, no study has examined the effect of Tai Chi on mindfulness in a randomized design with an active comparator.
Osteoarthritis (OA), the most common form of arthritis, is a disorder characterized by structural changes in joints (e.g., cartilage loss, osteophyte formation) as well as patient-reported pain, psychosocial symptoms, and functional limitations (Kraus, Blanco, Englund, Karsdal, & Lohmander, 2015). Knee OA is one of the primary causes of global disability because of chronic pain, physical disability, and psychosocial morbidities (Ma, Chan, & Carruthers, 2014). Currently, with no accepted disease-modifying treatment existing, exercise is the mainstay of non-pharmacological therapy, regardless of disease stage or symptom severity (Fransen et al., 2015). A growing number of studies indicate that Tai Chi may improve health in knee OA and other chronic pain diseases (Wang, 2012; Yan et al., 2013; Ye, Cai, Zhong, Cai, & Zheng, 2014). For example, a 12-week randomized Tai Chi or physical therapy (PT) intervention effectively reduced pain and improved the health-related quality of life among 204 individuals with knee OA (Wang et al., 2016). However, the comparative effects of Tai Chi and PT on mindfulness remains unknown and has not been examined among people with knee OA or other chronic pain diseases (Visted et al., 2015). Because a number of studies found beneficial effects of mindfulness among those with chronic pain (Delgado et al., 2014; Sharon et al., 2016), examining the mindfulness-cultivating effects of Tai Chi, distinct from those of an active comparator like PT, could support mindfulness as an important therapeutic mechanism of Tai Chi mind-body practice.
A better understanding of the underlying therapeutic mechanism can help to inform how Tai Chi modulates pain and improves quality of life. This knowledge may eventually lead to non-pharmacological disease-modifying treatments and help physicians make evidenced-based decisions when considering mind-body practice as an option for treatment among knee OA patients (Holzel et al., 2011). Therefore, the purpose of this study was to investigate the effect of Tai Chi mind-body exercise compared to exercise-based PT on self-reported total mindfulness among people with symptomatic knee OA. We hypothesized that Tai Chi mind-body exercise would increase total mindfulness levels more than PT exercise.
METHOD
Participants
Participants were recruited from a large metropolitan area through advertisements using print media (e.g. Boston Metro, Boston Fifty Plus), social media (e.g. Craigslist, Facebook), and the rheumatology clinic patient database at the hosting academic hospital. Inclusion criteria included: 1) age ≥ 40 years, 2) fulfillment of the American College of Rheumatology criteria for knee OA, and 3) Western Ontario and McMaster Osteoarthritis Index (WOMAC) pain score ≥ 40. Exclusion criteria included: 1) prior experience with complementary medicine or physical therapy programs for knee OA within the past year, 2) severe medical limitations precluding full participation, 3) intra-articular steroid injections or surgery in the past three months, 4) intra-articular hyaluronic acid injections in the past six months, 5) Mini-Mental Status examination score <24, or 6) inability to walk without an assistive device (Wang et al., 2014). We excluded persons who had participated in Tai Chi or physical therapy in the past year; those with current serious medical conditions, such as dementia, symptomatic heart or vascular disease, or recent stroke, that would limit full participation; those with intra-articular steroid or intra-articular hyaluronic acid injections in the past 3 or 6 months or reconstructive surgery before baseline screening on the most severely affected knee; and those with a score less than 24 on the Mini-Mental State Examination.
Procedure
This study was conducted as part of a 12-week NIH-funded, randomized trial comparing Tai Chi vs. PT among adults meeting the American College of Rheumatology Criteria for symptomatic knee OA (Trial Registry #: NCT01258985). A detailed description of the methodology and primary study results for this trial has been previously published (Wang et al., 2014, 2016).
Eligible participants were randomly assigned in a 1:1 ratio to Tai Chi or physical therapy using the R statistical package (R Development Core Team, 2012) and sealed, opaque envelopes with date and signature labels. The staff conducting the physical function assessments and the statistician were blinded to treatment assignment. All participants signed an informed consent form before enrollment, and the study was approved by the Institutional Review Board (Wang et al., 2014). The Five Facet Mindfulness Questionnaire (FFMQ) was used to measure mindfulness, and was formally implemented in the study protocol after subject recruitment and data collection had already begun. Therefore this study only reports data from the portion of enrolled participants who completed the FFMQ at baseline. Among this participant subgroup, some participants inadvertently did not receive the FFMQ to complete while at their 12-week visit. Because this occurred due to an administrative error that was independent of the participants, their 12-week data were treated as missing completely at random (MCAR). Therefore, the 24-week data were used for these participants because it contained their first available FFMQ at follow-up.
Tai Chi intervention
In brief, 60-minute Tai Chi group classes occurred twice per week for 12 weeks, led by 1 of 3 experienced (>20 years combined) Tai Chi instructors (Wang et al., 2014). The instructor administered a standardized 10-form modified Yang style Tai Chi protocol for knee OA at each session (Wang, Collet, & Lau, 2004). These selected 10 representative postures either induced progressive degrees of stress to postural stability or emphasized increasing magnitude of truck/arm rotation with diminishing base of support so that physical function could improve without excessive stress on the joints (Wang et al., 2014). At the first session, the instructor explained mind–body exercise theory and procedures; and participants received handouts on Tai Chi principles, practice techniques, and safety precautions. Classes typically involved an initial warm-up and a review of Tai Chi principles and movement, breathing techniques, and relaxation methods. Participants were asked to practice at home ≥20 minutes daily and encouraged to maintain usual physical activities with no new additional strength training other than their Tai Chi exercises. No explicit mention of mindfulness as a concept was made during the intervention.
Physical Therapy intervention
The physical therapy protocol was administered by 1 of 3 licensed physical therapists and followed U.S. guidelines for knee osteoarthritis treatment (Deyle et al., 2005), which consisted of two 30-minute one-to-one sessions with the physical therapist per week, for the first 6 weeks, and transitioned to a home-exercise program, which consisted of four 30-minute sessions per week, for the last 6 weeks. Thus, the home program (4 times per week for 30 minutes over 6 weeks plus the initial 6-week, individual Physical Therapy) was equivalent in dose to the Tai Chi intervention (twice a week for 60 minutes over 12 weeks). After an initial musculoskeletal examination, which lasted an hour, a physical therapist tailored the physical rehabilitation regimen toward specific treatment goals with participants. Each session consisted of joint mobilizations, active and passive range-of-motion exercises, strengthening exercises, lower limb stretching, aerobic exercises, and balance exercises. Participants were assigned home practice ≥20 minutes daily and encouraged to maintain usual physical activities with no new additional training other than their PT exercises.
Measures
The FFMQ is a self-reported outcome which measures total mindfulness and five different facets of mindfulness (Baer et al., 2008). Derived from exploratory factor analysis of the combined item pool of five independently-developed mindfulness assessment tools (Baer et al., 2008), the FFMQ consists of 39 five-point Likert scale questions (1=never or very rarely true to 5=very often or always true). Ranging from 39–195, higher total mindfulness scores reflect higher mindfulness. Validated in both meditating and non-meditating samples, the FFMQ was the highest rated mindfulness patient-report assessment tool for construct validity and internal consistency (Park, Reilly-Spong, & Gross, 2013). Missing items on the FFMQ were imputed using mean imputation as described in a previous study (Yu & Clark, 2015).
FFMQ Facets
1) The Observing facet (8 items, range 8–40) measures the ability to attend to or notice internal and external stimuli, such as sensations, emotions, cognitions, sights, sounds, and smells occurring in the present moment. 2) The Describing facet (8 items, range 8–40) measures noting or mentally labeling observed stimuli with words. 3) The Acting-with-Awareness facet (8 items, range 8–40) measures attending to one’s current actions, as opposed to behaving or reacting automatically or absentmindedly. 4) The Non-judging of experience facet (8 items, range 8–40) measures refraining from evaluation of one’s sensations, cognitions, and emotions as negative, unacceptable, or intolerable. 5) The Non-reactivity to experience facet (7 items, range 7–35) measures the ability to allow thoughts and feelings to come and go, without getting caught up in or carried away by them.
The WOMAC (VAS, version 3.1) is a self-report questionnaire consisting of 3 subscales used to assess pain, stiffness, and physical function in adults with hip or knee osteoarthritis (Bellamy, Buchanan, Goldsmith, Campbell, & Stitt, 1988). In this study, the pain and physical function subscales were utilized. The pain subscale ranges from 0–500 and consists of 5 items asking about pain during rest or activity. The physical function subscale ranges from 0–1700 and consists of 17 items asking about ability to perform daily activities.
The Six-minute Walk Test (6MW) measures functional exercise capacity as distance covered when asking participants to walk as far as possible within a six-minute period (Olsson & Swedberg, 2005).
Quality of life was assessed using the Short Form-36 (SF-36), a generic measure of health status consisting of two aggregate scores: the Physical Component Summary (PCS) score and the Mental Component Summary (MCS) score with well-documented psychometric properties (Ware Jr & Sherbourne, 1992). The SF-36 consists of 36 questions related to eight dimensions of quality of life. The questions are transformed into a point scale ranging from 0 to 100, with higher scores indicating better perceived health status.
A 21-question, validated, self-report instrument, the Beck Depression Inventory, second edition, (BDI) measures the severity of depressive symptoms (Steer, Ball, Ranieri, & Beck, 1999). Total scores range from 0–63 with higher scores reflecting greater depressive symptoms. BDI scores ranging from 0–13 represent minimal depressive symptoms; scores from 14–19 are mild; scores from 20–28 are moderate; and scores from 29–63 represent severe depressive symptoms.
Widely-used, the Perceived Stress Scale (PSS) measures the level of experienced stress, defined as the degree to which situations in one’s life over the past month are appraised as unpredictable, uncontrollable, and overwhelming(Nordin & Nordin, 2013). It consists of 10 items, and higher scores reflect a greater degree of perceived stress.
Self-efficacy, the belief that one can successfully take action to produce a desired outcome, was assessed using the Arthritis Self-Efficacy Scale-8 (ASES-8). The ASES-8 is a modified version of the Arthritis Self-Efficacy Scale that has been validated for patients with chronic pain (Brady, 2011). Each belief is rated on a 10-point Likert scale, where 1 = very uncertain and 10 = very certain, to indicate the level of certainty that patients can perform a task with higher scores indicating higher self-efficacy. The total score averages all responses.
Data Analysis
An established clinically meaningful difference in total FFMQ has not yet been reported (Park et al., 2013). The only previous study that used the FFMQ to compare Tai Chi with an active exercise comparator found that, among college students, a Tai Chi course significantly improved total FFMQ score by 12 ± 17 standard deviation (SD) points more than a recreation course (Caldwell et al., 2011). Based on this, we estimated that a study of 35 participants per group would have 80% power, using a two-sided t-test at a 0.05 level of significance, to detect a comparable difference on the FFMQ total score between Tai Chi and an active exercise comparator.
All data were examined visually and statistically for normality of distribution and presented as means ± SD unless otherwise stated. Significance level was set at p ≤ 0.05. Descriptive statistics were calculated and independent sample t-tests were used to test for mean differences between baseline participant characteristics of the two treatment groups and the changes in mindfulness between treatment groups after intervention. Paired t-tests were used to test for within-group change. To examine whether our sub-sample differed from participants in the parent study, we used t-tests to compare their baseline characteristics. We also used t-tests or chi-square tests to compare changes in mindfulness and other relevant measures of health, including pain, physical function, and depression, between participants assessed at 12 weeks and participants assessed at 24 weeks. To examine whether higher baseline levels of mindfulness may have influenced our findings, participants were stratified into equally-distributed tertiles based on total baseline FFMQ, and t-tests were used to test if mindfulness changed over time. Data were analyzed using SAS statistical software (Version 9.4).
RESULTS
Among the 86 participants measured at baseline, 56 were assessed at the 12-week visit, 19 were assessed at the 24-week visit, and 11 were lost to follow-up (Figure 1). Among the 75 participants assessed at follow-up, 41 were randomized to Tai Chi while 34 were randomized to PT.
Figure 1. Sub-study flow diagram.
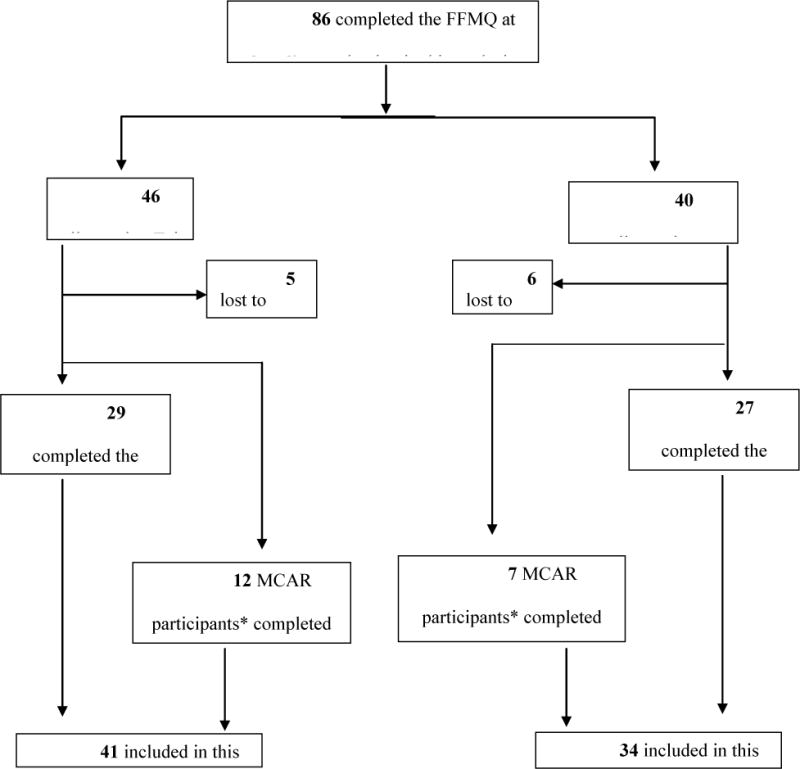
*Participants were confirmed to have attended the week 12 visit, but were inadvertently not given the FFMQ to complete. Therefore, these participants were confirmed to be Missing Completely at Random (MCAR).
Participant Characteristics
The 86 participants were predominantly female (74%), well-educated (85% with post-secondary education), and white (48%) with mean age of 60 years and body mass index of 33 kg/m2 (Table 1). Most (76%) had a Kellgren/Lawrence grade of 2 or 3, indicating definite osteophyte formation and possible joint space narrowing. Demographic variables were well-balanced between treatment groups at baseline, and demographic variables did not significantly differ between the participant sub-sample of this study and the other participants from the parent clinical trial (p = 0.08 to 0.94).
Table 1.
Demographic Characteristics of Participants by Treatment
| Characteristic | Tai Chi n=46 |
Physical Therapy n= 40 |
|---|---|---|
| Mean Age – yrs. | 59.9±10.1 | 60.9±10.8 |
| Female sex—no. of patients (%) | 35 (76) | 29 (73) |
| Race —no. of patients (%) | ||
| White | 18 (39) | 23 (58) |
| Black | 19 (41) | 11 (27) |
| Asian/Other | 9 (20) | 6 (15) |
| Body Mass Index, kg/m | 32.7±7.0 | 32.8±7.0 |
| Duration of knee pain - yrs. | 10.0±13.6 | 10.6±13.6 |
| Kellgren-Lawrence grade, no. (%)* | ||
| 0 | 1 (2) | 1 (3) |
| 1 | 4 (9) | 2 (5) |
| 2 | 18 (41) | 13 (33) |
| 3 | 17 (39) | 17 (43) |
| 4 | 4 (9) | 7 (18) |
| Highest Level of Education, n (%) | ||
| High school education | 6 (13) | 7 (18) |
| College/trade school | 17 (37) | 15 (37) |
| College Graduate | 12 (26) | 6 (15) |
| Graduate School | 11 (24) | 12 (30) |
All values are mean ± standard deviation, unless otherwise specified.
K/L grade for 2 participants in the Tai Chi group not recorded. Total Physical Therapy group percentage exceeds 100% due to rounding.
Table 2 summarizes the baseline levels and the mean change in health outcome measures by treatment group. After either intervention, participants reported reduced pain, depressive symptoms, and stress; and improved physical function, quality of life, self-efficacy, and walk distance. For the Tai Chi group, changes from baseline in all measures of health, except mental quality of life, reached significance. For the PT group, the changes from baseline in physical or mental quality of life, self-efficacy, depression, and stress did not reach significance. When compared with the PT group, the Tai Chi group had greater improvement in depressive symptoms (between group difference: −3.6 [95% CI: −6.9 to −0.3]) and physical quality of life 5.1 [95% CI: 1.1 to 9.1]). No significant difference in changes in pain, function, mental quality of life, perceived stress, self-efficacy, or walking distance was found between treatment groups (Table 2). These findings are consistent with those from the parent clinical trial (Wang et al., 2016).
Table 2.
Change in Health Outcomes Between Treatment Groups
| Variable, Score Range | Tai Chi (n=41) |
Physical Therapy (n=34) |
Between Groups Difference | P-value† |
|---|---|---|---|---|
| WOMAC Pain, 0–500mm | ||||
| Baseline Mean ± SD | 272.2 ± 93.4 | 258.0 ± 109.4 | 14.2 (−29.27, 57.68) ‡ | 0.52 |
| Mean Change, (95% CI) | −188.82 (−224.65, −152.99) | −138.68 (−179.02, −98.35) | −50.13 (−103.11, 2.85) | 0.06 |
| WOMAC Physical Function, 0–1700mm | ||||
| Baseline Mean ± SD | 964.0 ± 329.4 | 896.9 ± 389.0 | 67.05 (−87.00, 221.09)‡ | 0.39 |
| Mean Change, (95% CI) | −620.81 (−767.09, −474.53) | −443.13 (−604.63, −281.63) | −177.68 (− 392.13, 36.76) | 0.10 |
| SF-36 Physical Component¶, 0–100 | ||||
| Baseline Mean ± SD | 35.2± 7.4 | 37.9 ± 10.6 | −2.73 (−6.63, 1.15)‡ | 0.17 |
| Mean Change, (95% CI) | 6.92 (4.34, 9.51) | 1.80 (-1.43, 5.02) | 5.12 (1.12, 9.14) | 0.01 |
| SF-36 Mental Component¶, 0–100 | ||||
| Baseline Mean ± SD | 52.1 ± 9.6 | 53.6 ± 8.2 | −1.56 (−5.42, 2.30)‡ | 0.42 |
| Mean Change, (95% CI) | 1.68 (−0.73, 4.09) | −0.64 (−2.97, 1.69) | 2.31 (−1.03, 5.66) | 0.17 |
| Beck II Depression Inventory, 0–63 | ||||
| Baseline Mean ± SD | 8.8 ± 9.0 | 6.4± 8.3 | 2.33 (−1.41, 6.07)‡ | 0.21 |
| Mean Change, (95% CI) | −3.00 (−4.55, −1.44) | 0.62 (−2.55, 3.79) | −3.62 (−6.93, −0.31) | 0.03 |
| Arthritis Self-Efficacy Scale¶, 1–10 | ||||
| Baseline Mean ± SD | 6.0 ± 1.9 | 6.6 ± 2.1 | −0.61 (−1.47, 0.25)‡ | 0.16 |
| Mean Change, (95% CI) | 1.28 (0.51, 2.05) | 0.51 (−0.42, 1.44) | 0.77 (−0.41, 1.95) | 0.20 |
| Perceived Stress Scale, 0–40 | ||||
| Baseline Mean ± SD | 13.3 ± 6.9 | 12.9 ± 6.7 | 0.45 (−2.48, 3.38)‡ | 0.76 |
| Mean Change, (95% CI) | −1.80 (−3.27, −0.34) | −0.41 (−2.11, 1.29) | −1.39 (−3.58, 0.80) | 0.21 |
| 6 minute walk¶ | ||||
| Baseline Mean ± SD | 386.5 ± 93.6 | 409.6 ± 87.4 | −23.12 (−62.93, 16.68)‡ | 0.25 |
| Mean Change, (95% CI) | 30.81 (14.43, 47.18) | 18.08 (0.69, 35.46) | 12.73 (−10.82, 36.28) | 0.28 |
Abbreviations: WOMAC = Western Ontario and McMasters Arthritis Index; SF-36= Short Form-36, CI = Confidence Intervals; SD = standard deviation. Mean ± SD unless noted otherwise.
T-tests were performed to assess difference in change between groups.
(95% CI).
Higher score indicates better health. Note: Follow-up measures occurred at 12 or 24 weeks post-baseline, depending on when the follow-up Five Facet Mindfulness Questionnaire was completed.
Changes in Mindfulness
Table 3 summarizes the baseline levels and mean changes of mindfulness by treatment group. Participants had a high mean total FFMQ score (142 ± 17) at baseline. The treatment groups did not significantly differ in mindfulness levels at baseline (p = 0.21 to 0.78). Total or facet mindfulness scores did not significantly change more after Tai Chi than PT (p value= 0.07–0.84). Further, there were no significant changes between baseline and 12-week follow-up in total or facet mindfulness after PT. Among the mindfulness facets after Tai Chi intervention, only Non-judging (mean change: 1.80, 95% CI: 0.46 to 3.15) significantly increased between baseline and follow-up. However, the amount of change was 0.31 of the baseline SD, which is a relatively small effect size. No significant change from baseline was observed after Tai Chi for total mindfulness or the Describing, Observing, Acting-with-Awareness, and Non-reacting facets.
Table 3.
Change in Mindfulness Between Treatment Groups
| FFMQ Variable*, Score Range | Tai Chi (n=41) |
Physical Therapy (n=34) |
Between Groups Difference | P-value† |
|---|---|---|---|---|
| Total Mindfulness 39–195 | ||||
| Baseline Mean ± SD | 141.4± 17.3 | 142.4± 16.9 | −1.02 (−8.38, 6.34)‡ | 0.78 |
| Mean Change, (95% CI) | 0.76 (−2.93,4.45) | 1.80 (−2.33, 5.93) | −1.04 (−6.48, 4.39) | 0.70 |
| Observing 8–40 | ||||
| Baseline Mean ± SD | 27.7± 5.9 | 29.1± 6.6 | −1.36 (−4.04, 1.31)‡ | 0.31 |
| Mean Change, (95% CI) | −1.00 (−2.17, 0.17) | 0.73 (−0.92, 0.76) | −1.72 (−3.67, 0.21) | 0.08 |
| Describing 8–40 | ||||
| Baseline Mean ± SD | 30.5± 5.7 | 30.9± 6.1 | −0.41 (−2.94, 2.12)‡ | 0.75 |
| Mean Change, (95% CI) | −0.18 (−1.64, 1.27) | 0.00 (−1.08, 1.08) | −0.18 (−2.03, 1.66) | 0.84 |
| Acting-with-Awareness 8–40 | ||||
| Baseline Mean ± SD | 30.9± 6.0 | 29.7± 7.0 | 1.28 (−1.52, 4.09)‡ | 0.36 |
| Mean Change, (95% CI) | 0.66 (−0.96, 2.28) | −0.50 (−2.32, 1.32) | 1.16 (−1.23, 3.55) | 0.34 |
| Non-Judging 8–40 | ||||
| Baseline Mean ± SD | 30.3± 5.9 | 29.5± 5.9 | 0.80 (−1.73, 3.33)‡ | 0.53 |
| Mean Change, (95% CI) | 1.80 (0.46, 3.15) | 0.41 (−1.05, 1.88) | 1.39 (−0.57, 3.35) | 0.16 |
| Non-Reacting 7–35 | ||||
| Baseline Mean ± SD | 22.0± 4.8 | 23.3± 4.9 | −1.33 (−3.43, 0.76)‡ | 0.21 |
| Mean Change, (95% CI) | −0.52 (−1.48, 0.45) | 1.16 (−0.52, 2.84) | −1.68 (−3.51, 0.15) | 0.07 |
Abbreviations: CI = Confidence Intervals; SD = standard deviation.
FFMQ = Five Facet Mindfulness Questionnaire; higher scores indicate higher levels of mindfulness.
T-tests were performed to assess difference in change between groups.
(95% CI). Note: Follow-up measures occurred at 12 or 24 weeks post-baseline, depending on when the follow-up FFMQ was completed.
From our sensitivity analysis, we found small, non-significant between-group difference in change in mindfulness (mean change at week 12: −0.03±10.9; at week 24: 4.97±13.4; (week-12 – week-24) mean difference: −5.0, p=0.11) and pain, function, or depression (p = 0.53 to 0.98) between participants assessed at 12 weeks and participants assessed at 24 weeks. Notably, the change in mindfulness was actually larger in the group measured at 24 weeks. In addition, participants stratified to the lower (n=24; baseline FFMQ: 124 ±8.4; change: 2.5 ±12, p= 0.11), medium (n=25; baseline FFMQ: 141 ±3.6; change: 2.1 ±12, p= 0.45), or higher (n=26; baseline FFMQ: 161 ±9.5; change: −0.9 ±−11, p= 0.74) baseline mindfulness tertiles had small and non-significant changes in mindfulness at follow-up. Although the average change in mindfulness among the lower tertile was larger than that among the higher tertile, the amount of change among participants from the lower tertile assigned to Tai Chi (n=14; mean=2.0) was smaller than the change among participants from the lower tertile assigned to PT (n=10; mean=3.2).
Missing items
At baseline, 5 people had 1 missing item and 1 person had 2 missing items from the FFMQ. At 12 weeks, 1 person had 1 missing item and 2 people had 18 missing items. At 24 weeks, 2 people had 1 missing item. In each case missing items were imputed and the total FFMQ scores were included in the study participant sample.
DISCUSSION
This study examined the effect of Tai Chi mind-body exercise versus standard PT on mindfulness among people with symptomatic knee OA. We found that the Non-judging facet increased after Tai Chi intervention but only modestly. Despite our initial hypothesis, we found that Tai Chi did not improve total or facet mindfulness significantly more than PT. We also found that total or facet mindfulness did not significantly change after PT from baseline. Similarly, total or Non-reacting, Describing, Acting-with-Awareness, and Observing facets did not significantly change after Tai Chi intervention from baseline. Our findings are inconsistent with previously-reported studies of Tai Chi mind-body interventions among healthy volunteers and with the widely-held notion that Tai Chi mind-body exercise cultivates mindfulness. Our findings also generate important follow-up questions that future studies can address.
Concordant with our findings, though, previous studies using mindfulness-based interventions, such as MBSR or sitting meditation, also found no change in mindfulness (measured using the Freiburg Mindfulness Inventory or FFMQ) among chronic pain participants despite substantial improvements in both pain and pain-related symptoms (Morone, Rollman, Moore, Li, & Weiner, 2009; Schmidt et al., 2011). Further, a recent meta-analysis of mindfulness interventions among people with chronic pain did not find significant improvements in mindfulness (Bawa et al., 2015). Suggested explanations for these negative findings have included concerns about the inadequacy of the various self-reported measures of mindfulness (Bergomi, Tschacher, & Kupper, 2013; Park et al., 2013; Tsafou, Lacroix, Ee, Vinkers, & Ridder, 2016), the heterogeneity of the types interventions employed (Christopher et al., 2015), and conceptual disagreements on whether mindfulness as a process differs from mindfulness as an outcome (Kabat-Zinn, 2015). Our findings that FFMQ-measured mindfulness did not change after Tai Chi mind-body exercise despite beneficial effects on health contribute to this debate, and highlight the need for further investigations to identify mechanisms of mind-body practice.
In contrast to our findings, two prior studies found that mindfulness significantly increased after Tai Chi intervention (Caldwell et al., 2011; Nedeljkovic et al., 2012). Because these studies included participants of healthy volunteers, mindfulness may not have increased among our participants due to negative modulation from the underlying chronic pain of their OA. Chronic pain from OA and other diseases is known to have complex effects via somatic, cognitive, and limbic pathways of perceptions (Lange, Gorbunova, & Christ, 2012; Phillips & Clauw, 2011; Woolf, 2012), but whether pain can directly affect change in mindfulness is unknown. The simplest interpretation of our findings is that, for people with knee OA, Tai Chi practice does not appear to change mindfulness, or that change in mindfulness may not be relevant to the way Tai Chi mind-body exercise improves health among those with knee OA.
Although the role of mindfulness in clinical interventions is a rapidly growing topic of research, the body of evidence identifying it as a therapeutic mechanism remains limited. Accordingly, the relative degree to which various mind-body or mindfulness-based interventions change mindfulness is not yet clear. Mindfulness is a commonly-assumed component of mind-body exercise such as Tai Chi, but mind-body exercise may utilize a distinct type of meditation as an underlying component (Gould et al., 2014; Kelley & Kelley, 2015; Larkey, Jahnke, Etnier, & Gonzalez, 2009). Also, particular instructors and the degree of emphasis they place on development of non-judgmental present-moment awareness as part of their instruction may also impact the degree to which mindfulness is developed among participants of particular mind-body exercise group. Mind-body interventions could play an important role by improving the physical aspects of knee OA without the harmful side effects associated with current pharmacological treatments, such as opioids or non-steroidal anti-inflammatory medications. Mind-body interventions could also benefit the psycho-social difficulties of knee OA, which may not be effectively treated by exercise-based PT, the current non-pharmacological standard of care (Fransen et al., 2015). As mind-body interventions continue to demonstrate beneficial effects among people with knee OA and other chronic pain diseases, a better understanding of its meditative component is warranted(Lee, Crawford, & Hickey, 2014; Morone & Greco, 2007).
There are several possible explanations that may have accounted for our findings. First, we emphasized the physical aspects of the Tai Chi regimen in order to match the intervention with the natural underlying disease process of knee OA. For example, we selected 10 representative Tai Chi postures based on their characteristics of physical motion. In addition, the Tai Chi instructors did not verbally introduce and periodically refer to the concept of ‘mindfulness’ during this Tai Chi program. The effects of these elements from the interventional design may have inadvertently attenuated the detectable amount of change in mindfulness. Nevertheless, our modified regimen of Tai Chi was ultimately effective in significantly reducing pain and improving physical function among our participants (Wang et al., 2016), and therefore, the pragmatic relevance for cultivating mindfulness through Tai Chi among this patient group remains unproven. Second, our participants had an unusually high amount of total mindfulness at baseline, which could imply that, if change in mindfulness is influenced by the initial levels found at baseline, higher levels versus lower levels of mindfulness may be less susceptible to change due to ceiling effects. However, the small amount of change in mindfulness (≈2 points) among participants with baseline levels that were similar to those from previous studies (Baer et al., 2008) is unlikely to be clinically meaningful. Furthermore, among this subgroup, average change in mindfulness was smaller among those who received Tai Chi than among those who received PT. This suggests that the influence of a ‘ceiling effect’ that could have limited our ability to detect change in mindfulness was not substantial. Indeed, because mindfulness was not commonly measured as an outcome of interest in prior trials of mindfulness-based interventions in chronic pain, there is a dearth of evidence from which to compare, and a clear rationale for our findings is not readily apparent (Bawa et al., 2015).
Limitations
The results of this study should be interpreted within the context of its limitations. First, without finding change in mindfulness after either intervention, we were precluded from examining associations between change in mindfulness and change in health outcomes. In addition, the primary purpose of the parent clinical trial was distinct from the purpose of this study. Therefore, our results require confirmation in a clinical study primarily designed to examine the effect of Tai Chi versus PT on mindfulness. In addition, our study sample was not an epidemiological representative of all people with knee OA because our participants were actively symptomatic and knowingly participated in a Tai Chi vs. PT study in an academic clinical setting, which may influence the generalizability of our results. Other limitations may include our sample size, our imputing missing 12-week data with 24-week data, and the administrative error that precipitated the missing data. Despite the administrative error, in which the FFMQ was erroneously excluded from survey packets, the study staff was able to appropriately identify and correct it in a timely manner. Furthermore, our sensitivity analysis, which did not find substantial difference between mindfulness change at 12 and 24 weeks, supports the internal validity of our results and that the effects of the error were not complex. While we cannot rule out a lack of power as a confounder of our results, our sample size is similar to those reported from comparable studies (Morone, Greco, & Weiner, 2008; Nedeljkovic et al., 2012). Importantly, the amount of average change in total mindfulness or mindfulness facets from Tai Chi was small (ranged from worsening by 1 point to improving by 1.8 points). Furthermore, our actual sample sizes for each treatment group at follow-up (41 for Tai Chi and 34 for PT) were very close to the estimated size requirement (35 participants per group) that was generated from our a priori power analysis. Taken together, this information does not support sampling power as the explanation of our findings. Similarly, we cannot rule out that the high baseline levels of mindfulness among participants may have introduced a ceiling effect, our sensitivity analysis, which showed a small, non-significant change among participants with representative levels of baseline mindfulness, do not support a ceiling effect as the primary explanation for our findings. Finally, although it has been used in multiple studies and has the highest construct validity and internal consistency among patient-report assessment tools for mindfulness (Park et al. 2013), the FFMQ may lack sufficient sensitivity for detecting mindfulness changes related to Tai Chi and PT in individuals with knee OA.
Further study is required to explore the underlying mechanisms of mind-body interventions such as Tai Chi. Comparative studies among people with or without chronic pain can help substantiate whether pain plays a role to impede the cultivation of mindfulness through Tai Chi practice. Future studies examining mindfulness among people with knee OA should also explore associations between changes in mindfulness with changes in health outcomes, or whether explicit mindfulness training in addition to Tai Chi practice confers any additional benefit. Lastly, further knowledge is needed to better understand how adjustments in the design of a Tai Chi intervention can affect its underlying effect on mindfulness.
Acknowledgments
The authors gratefully appreciate Ramel Rones, Dorri Li and Brian Muccio for their expertise in teaching the Tai Chi groups; Maura Iversen, Megan Whitmore, Marie Boneparth, and Jane Lucas for their expert physical therapy instruction; Stephanie Hyon and Sun Yu for feedback on the written manuscript; and the study participants, whose cooperation, encouragement, and enthusiasm are an inspiration.
Funding: This study is supported by the National Center for Complementary and Integrative Health (R01AT005521 and K24AT007323), and National Center for Advancing Translational Sciences (UL1TR001064) at the National Institutes of Health. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. The investigators are solely responsible for the content of the manuscript and the decision to submit for publication. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of Interests: The authors declare that they have no conflict of interest.
Author contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Lee had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design: Lee, Price, Harvey, Wong, Chung, Han, Driban, Morgan L, Morgan N, Wang
Acquisition of data: Lee, Price, Harvey, Wong, Chung, Han, Driban, Morgan L, Morgan N, Wang
Analysis and interpretation of data: Lee, Price, Harvey, Wong, Chung, Han, Driban, Morgan L, Morgan N, Wang
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Author contributions
AL: designed and executed the study, assisted with the data acquisition and analyses, interpreted the data, and wrote the paper. WF: collaborated with the design, data acquisition and interpretation, writing, and editing of the study. JW: collaborated with the design, data interpretation, writing, and editing of the study. LLP: acquired and analyzed the data, and collaborated with the design, data interpretation, and editing of the study. XH: assisted with the acquisition and analysis of data, design, and editing of the study. MC: collaborated on the analysis and interpretation of the data, and assisted with the design and editing of the study. JD: collaborated with the design, data interpretation, and the writing and editing of the study. LM: wrote portions of the methods and discussion, and collaborated with the design, data interpretation, and editing of the study. NM: wrote portions of the methods, assisted with data acquisition, and collaborated with the design and editing of the study. CW: collaborated with the design, data acquisition and interpretation, writing, and editing of the study.
References
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JMG. Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. http://doi.org/10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bawa FLM, Mercer SW, Atherton RJ, Clague F, Keen A, Scott NW, Bond CM. Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. The British Journal of General Practice. 2015;65(635):e387–400. doi: 10.3399/bjgp15X685297. http://doi.org/10.3399/bjgp15X685297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of Rheumatology. 1988;15(12):1833–1840. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3068365. [PubMed] [Google Scholar]
- Bergomi C, Tschacher W, Kupper Z. The Assessment of Mindfulness with Self-Report Measures: Existing Scales and Open Issues. Mindfulness. 2013;4(3):191–202. http://doi.org/10.1007/s12671-012-0110-9. [Google Scholar]
- Brady TJ. Measures of self-efficacy: Arthritis Self-Efficacy Scale (ASES), Arthritis Self-Efficacy Scale-8 Item (ASES-8), Children’s Arthritis Self-Efficacy Scale (CASE), Chronic Disease Self-Efficacy Scale (CDSES), Parent’s Arthritis Self-Efficacy Scale (PASE), an. Arthritis Care & Research. 2011 Nov;63(Suppl 1):S473–85. doi: 10.1002/acr.20567. http://doi.org/10.1002/acr.20567. [DOI] [PubMed] [Google Scholar]
- Caldwell K, Emery L, Harrison M, Greeson J. Changes in mindfulness, well-being, and sleep quality in college students through taijiquan courses: a cohort control study. Journal of Alternative and Complementary Medicine (New York, NY) 2011;17(10):931–938. doi: 10.1089/acm.2010.0645. http://doi.org/10.1089/acm.2010.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YW, Hunt MA, Campbell KL, Peill K, Reid WD. The effect of Tai Chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses. British Journal of Sports Medicine. 2015 doi: 10.1136/bjsports-2014-094388. http://doi.org/10.1136/bjsports-2014-094388. [DOI] [PubMed]
- Christopher MS, Rogers B, Hunsinger M, Colgan D, Reiss AL, Farwood HB. Distinguishing Mindful Process from Outcome in the Prediction of Global Health and Perceived Stress in a Mindfulness-Based Stress Reduction Program. Mindfulness. 2015;6(4):693–699. http://doi.org/10.1007/s12671-014-0305-3. [Google Scholar]
- Delgado R, York A, Lee C, Crawford C, Buckenmaier C, 3rd, Schoomaker E, Crawford P. Assessing the quality, efficacy, and effectiveness of the current evidence base of active self-care complementary and integrative medicine therapies for the management of chronic pain: a rapid evidence assessment of the literature. Pain Medicine (Malden, Mass) 2014;15(Suppl 1):S9–20. doi: 10.1111/pme.12412. http://doi.org/10.1111/pme.12412. [DOI] [PubMed] [Google Scholar]
- Deyle GD, Allison SC, Matekel RL, Ryder MG, Stang JM, Gohdes DD, Garber MB. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Physical Therapy. 2005;85(12):1301–1317. [PubMed] [Google Scholar]
- Fransen M, Mcconnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. The Cochrane Database of Systematic Reviews. 2015;(1):CD004376. doi: 10.1002/14651858.CD004376.pub3. http://doi.org/10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed]
- Gould LF, Mendelson T, Dariotis JK, Ancona M, Smith ASR, Gonzalez AA, Greenberg MT. Assessing fidelity of core components in a mindfulness and yoga intervention for urban youth: Applying the CORE Process. New Directions for Youth Development. 2014;2014(142):59–81. doi: 10.1002/yd.20097. http://doi.org/10.1002/yd.20097. [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. http://doi.org/10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Holzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. http://doi.org/10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Meditation-It’s Not What You Think. Mindfulness. 2015;6(2):393–395. http://doi.org/10.1007/s12671-015-0393-8. [Google Scholar]
- Kabat-zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8(2):163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Kelley GA, Kelley KS. Meditative Movement Therapies and Health-Related Quality-of-Life in Adults: A Systematic Review of Meta-Analyses. Plos One. 2015;10(6):e0129181. doi: 10.1371/journal.pone.0129181. http://doi.org/10.1371/journal.pone.0129181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus VB, Blanco FJ, Englund M, Karsdal MA, Lohmander LS. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthritis and Cartilage. 2015;23(8):1233–41. doi: 10.1016/j.joca.2015.03.036. http://doi.org/10.1016/j.joca.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange K, Gorbunova A, Christ O. The Influence of Mindfulness on Different Aspects of Pain Perception and Affective Reactivity to Pain - Feasibility of a Multimethodical Approach. Mindfulness. 2012;3:209–217. http://doi.org/10.1007/s12671-012-0113-6. [Google Scholar]
- Larkey L, Jahnke R, Etnier J, Gonzalez J. Meditative movement as a category of exercise: implications for research. Journal of Physical Activity & Health. 2009;6(2):230–238. doi: 10.1123/jpah.6.2.230. [DOI] [PubMed] [Google Scholar]
- Lee C, Crawford C, Hickey A. Mind–Body Therapies for the Self-Management of Chronic Pain Symptoms and Active Self-Care Therapies for Pain (PACT) Working Group. Pain Medicine. 2014;15:S21–39. doi: 10.1111/pme.12383. [DOI] [PubMed] [Google Scholar]
- Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the united states: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pa. Archives of Physical Medicine and Rehabilitation. 2014;95(5):986–995e1. doi: 10.1016/j.apmr.2013.10.032. http://doi.org/10.1016/j.apmr.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morone NE, Greco CM. Mind–Body Interventions for Chronic Pain in Older Adults: A Structured Review. Pain Medicine. 2007;8(4):359–375. doi: 10.1111/j.1526-4637.2007.00312.x. http://doi.org/10.1111/j.1526-4637.2007.00312.x. [DOI] [PubMed] [Google Scholar]
- Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134(3):310–319. doi: 10.1016/j.pain.2007.04.038. http://doi.org/10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morone NE, Rollman BL, Moore CG, Li Q, Weiner DK. A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain Medicine (Malden, Mass) 2009;10(8):1395–1407. doi: 10.1111/j.1526-4637.2009.00746.x. http://doi.org/10.1111/j.1526-4637.2009.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Complementary and Integrative Health. Spotlight on a Modality: Tai Chi. 2015 Retrieved July 1 2016, from https://nccih.nih.gov/health/providers/digest/taichi.
- Nedeljkovic M, Wirtz P, Ausfeld-Hafter B. Effects of Taiji Practice on Mindfulness and Self-Compassion in Healthy Participants—A Randomized Controlled Trial. Mindfulness. 2012;3(3):200–208. http://doi.org/10.1007/s12671-012-0092-7. [Google Scholar]
- Nordin M, Nordin S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scandinavian Journal of Psychology. 2013;54(1996):502–507. doi: 10.1111/sjop.12071. http://doi.org/10.1111/sjop.12071. [DOI] [PubMed] [Google Scholar]
- Olsson L, Swedberg K. Six minute walk test. European Heart Journal. 2005;26(20):2209–2209. doi: 10.1093/eurheartj/ehi452. http://doi.org/10.1093/eurheartj/ehi452. [DOI] [PubMed] [Google Scholar]
- Park T, Reilly-Spong M, Gross CR. Mindfulness: A systematic review of instruments to measure an emergent patient-reported outcome (PRO) Quality of Life Research. 2013;22(10):2639–2659. doi: 10.1007/s11136-013-0395-8. http://doi.org/10.1007/s11136-013-0395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen M, la Cour P. Mindfulness-What Works for Whom? Referral, Feasibility, and User Perspectives Regarding Patients with Mixed Chronic Pain. Journal of Alternative and Complementary Medicine (New York, NY) 2016;22(4):298–305. doi: 10.1089/acm.2015.0310. http://doi.org/10.1089/acm.2015.0310. [DOI] [PubMed] [Google Scholar]
- Phillips K, Clauw DJ. Central pain mechanisms in chronic pain states–maybe it is all in their head. Best Practice & Research Clinical Rheumatology. 2011;25(2):141–154. doi: 10.1016/j.berh.2011.02.005. http://doi.org/10.1016/j.berh.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posadzki P, Jacques S. Tai Chi and Meditation. Journal of Holistic Nursing. 2009;27(2):103–114. doi: 10.1177/0898010108330807. http://doi.org/10.1177/0898010108330807. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain. 2011;152(2):361–369. doi: 10.1016/j.pain.2010.10.043. http://doi.org/10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- Sharon H, Maron-Katz A, Ben Simon E, Flusser Y, Hendler T, Tarrasch R, Brill S. Mindfulness Meditation Modulates Pain through Endogenous Opioids. The American Journal of Medicine. 2016 doi: 10.1016/j.amjmed.2016.03.002. http://doi.org/10.1016/j.amjmed.2016.03.002. [DOI] [PubMed]
- Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. Journal of Clinical Psychology. 1999;55(1):117–128. doi: 10.1002/(sici)1097-4679(199901)55:1<117::aid-jclp12>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- Tsafou K, Lacroix JPW, Van Ee R, Vinkers CDW, De Ridder DTD. The relation of trait and state mindfulness with satisfaction and physical activity : A cross-sectional study in 305 Dutch participants. Journal of Health Psychology. 2016 doi: 10.1177/1359105315624748. http://doi.org/10.1177/1359105315624748. [DOI] [PubMed]
- Visted E, Vollestad J, Nielsen MB, Nielsen GH. The Impact of Group-Based Mindfulness Training on Self-Reported Mindfulness: a Systematic Review and Meta-analysis. Mindfulness. 2015;6(3):501–522. http://doi.org/10.1007/s12671-014-0283-5. [Google Scholar]
- Wang C. Role of Tai Chi in the treatment of rheumatologic diseases. Current Rheumatology Reports. 2012;14(6):598–603. doi: 10.1007/s11926-012-0294-y. http://doi.org/10.1007/s11926-012-0294-y. [DOI] [PubMed] [Google Scholar]
- Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Archives of Internal Medicine. 2004;164(5):493–501. doi: 10.1001/archinte.164.5.493. http://doi.org/10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- Wang C, Iversen MD, McAlindon T, Harvey WF, Wong JB, Fielding RA, Schmid CH. Assessing the comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: design and rationale for a randomized trial. BMC Complementary and Alternative Medicine. 2014;14(1):333. doi: 10.1186/1472-6882-14-333. http://doi.org/10.1186/1472-6882-14-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Schmid CH, Iversen MD, Harvey WF, Fielding RA, Driban JB, McAlindon T. Comparative Effectiveness of Tai Chi Versus Physical Therapy for Knee Osteoarthritis: A Randomized Trial. Annals of Internal Medicine. 2016 doi: 10.7326/M15-2143. http://doi.org/10.7326/M15-2143. [DOI] [PMC free article] [PubMed]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wayne PM, Kaptchuk TJ. Challenges Inherent to T’ai Chi Research: Part I— T’ai Chi as a Complex Multicomponent Intervention. The Journal of Alternative and Complementary Medicine. 2008;14(1):95–102. doi: 10.1089/acm.2007.7170a. http://doi.org/10.1089/acm.2007.7170A. [DOI] [PubMed] [Google Scholar]
- Woolf CJ. Central Sensitization: Implications for the diagnosis and treatment of pain. Pain. 2012;152(3 Supplemental):1–31. doi: 10.1016/j.pain.2010.09.030. http://doi.org/10.1016/j.pain.2010.09.030.Central. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan JH, Gu WJ, Sun J, Zhang WX, Li BW, Pan L. Efficacy of Tai Chi on Pain, Stiffness and Function in Patients with Osteoarthritis: A Meta-Analysis. PLoS ONE. 2013;8(4):e61672. doi: 10.1371/journal.pone.0061672. http://doi.org/10.1371/journal.pone.0061672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J, Cai S, Zhong W, Cai S, Zheng Q. Effects of Tai Chi for Patients with Knee Osteoarthritis: A Systematic Review. Journal of Physical Therapy Science. 2014;26(7):1133–1137. doi: 10.1589/jpts.26.1133. http://doi.org/10.1589/jpts.26.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M, Clark M. Investigating Mindfulness, Borderline Personality Traits, and Well-Being in a Nonclinical Population. Psychology. 2015;6(6):1232–1248. http://doi.org/10.4236/psych.2015.610121. [Google Scholar]


