Abstract
Introduction:
The purpose of this position paper is to establish the American Academy of Sleep Medicine's (AASM) position on the use of a home sleep apnea test (HSAT) for the diagnosis of obstructive sleep apnea (OSA) in children (birth to 18 years of age).
Methods:
The AASM commissioned a task force of 8 experts in sleep medicine to review the available literature on the use of an HSAT to diagnose OSA in children. The task force developed the position statement based on a thorough review of these studies and their clinical expertise. The AASM Board of Directors approved the final position statement.
Position Statement:
Use of a home sleep apnea test is not recommended for the diagnosis of obstructive sleep apnea in children. The ultimate judgment regarding propriety of any specific care must be made by the clinician, in light of the individual circumstances presented by the patient, available diagnostic tools, accessible treatment options, and resources.
Citation:
Kirk V, Baughn J, D'Andrea L, Friedman N, Galion A, Garetz S, Hassan F, Wrede J, Harrod CG, Malhotra RK. American Academy of Sleep Medicine position paper for the use of a home sleep apnea test for the diagnosis of OSA in children. J Clin Sleep Med. 2017;13(10):1199–1203.
Keywords: diagnosis, home sleep apnea test, obstructive sleep apnea, pediatric
INTRODUCTION
Two American Academy of Sleep Medicine (AASM) guidelines, the “Practice Parameters for the Respiratory Indications for Polysomnography in Children,”1 and “Practice Parameters for the Non-Respiratory Indications for Polysomnography and Multiple Sleep Latency Testing for Children”2 previously addressed the role of attended in-laboratory polysomnography (PSG) for the diagnosis of sleep disorders in children. There are also recently published AASM guidelines on the diagnostic testing for obstructive sleep apnea (OSA) which address the use of a home sleep apnea test (HSAT) in adults.3 The readily available HSAT devices require significantly fewer resources than PSG, and may provide clinical benefit; however, the existing AASM guidelines do not offer recommendations on the use of an HSAT in the pediatric population (birth to 18 years of age). The AASM commissioned a task force of experts in pediatric sleep medicine to develop a position paper on the utility of an HSAT in this population, based on a review of the available literature and their clinical expertise (see Methodology in the supplemental material). The clinical research questions addressed in this paper and the literature search terms employed are presented in the supplemental material, Table S1 and Table S2, respectively. This position paper provides guidance to all practitioners who care for pediatric patients with suspected OSA.
BACKGROUND
OSA in children is a disease characterized by recurrent episodes of partial or complete upper airway obstruction associated with arousals, awakenings, and/or oxyhemoglobin desaturations during sleep. It may also be associated with disruption of ventilation and normal sleep patterns.4
Current data indicate prevalence of OSA among children ranges between 1% to 4% and the typical treatment is adenotonsillectomy. Severe OSA is associated with higher perioperative complications, so accurate preoperative diagnosis is important for planning postoperative management. Certain pediatric populations are also at higher risk for residual OSA after surgery, including those with severe preoperative OSA. Lastly, untreated OSA in children is associated with significant medical, developmental, and psychosocial complications so accurate diagnostic testing is important for this population.5–10
The gold standard for diagnosis of OSA in children is PSG.11 Diagnosis of OSA in children is based, in part, on the apneahypopnea index (AHI) identified by PSG that indicates whether there are an abnormal number of respiratory events occurring per hour of sleep. The International Classification of Sleep Disorders, Third Edition (ICSD-3) defines pediatric OSA as an AHI ≥ 1 or a pattern of obstructive hypoventilation defined as at least 25% of total sleep time with hypercapnia (PaCO2 > 50 mm Hg) in association with snoring, flattening of the nasal V Kirk, J Baughn, L D'Andrea, et al. Use of HSAT for the Diagnosis of OSA in Children pressure waveform, or paradoxical respiratory efforts.12 Partial airway obstruction is more common, and oxygen desatu-ration is less common, in children with OSA in comparison with adults8; therefore, The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications (AASM Scoring Manual) includes associated arousals.13 The additional measurement of carbon dioxide, the use of video, and the scoring of arousals with respiratory events are also used in the interpretation of pediatric PSG.
Unfortunately, PSG is expensive and setup can be challenging, as the placement of numerous electrodes can be difficult in children of younger neurodevelopmental age or status. Additionally, access to PSG can be limited based on geographic location and proximity to tertiary care centers. In recent years there has been increased interest in the use of HSATs in children, which can be performed in the home and typically uses fewer sensors than PSG (see the AASM Scoring Manual13 for technical and digital specifications). However, because these devices measure fewer physiologic variables than PSG (eg, absence of carbon dioxide measurement and identification of arousals), use of HSATs may lead to underestimation of the presence or severity of disease. Therefore, the absence of any of these measures must be carefully considered when evaluating the validity of HSATs in children.
This position paper serves as guidance to practitioners in the diagnosis of pediatric OSA. The task force developed the position statement by consensus based on a thorough review of relevant evidence and their clinical expertise. The AASM Board of Directors approved the final position statement. The ultimate judgment regarding propriety of any specific care must be made by the clinician, in light of the individual circumstances presented by the patient, available diagnostic tools, accessible treatment options, and resources.
POSITION STATEMENT
The AASM supports the following position on the use of HSATs to diagnose OSA in children:
Use of a home sleep apnea test is not recommended for the diagnosis of obstructive sleep apnea in children.
Remarks: For the purposes of this position statement, children are defined as individuals < 18 years old.
The ultimate judgment regarding propriety of any specific care must be made by the clinician, in light of the individual circumstances presented by the patient, available diagnostic tools, accessible treatment options, and resources.
The clinical use of HSATs in pediatric populations is not recommended due to insufficient evidence. Specifically, there is limited literature comparing HSATs to PSG, the gold standard, in children. The task force was also unable to identify literature on the use of HSAT devices that monitor CO2 or have the ability to identify arousals, measurements that have been viewed as critical in pediatric populations. Additionally, the task force identified limited literature comparing HSATs to PSG in children with comorbidities or in young children.
Technical Feasibility of HSATs in Children
Overall, the task force identified 4 published articles focusing on the feasibility of using an HSAT in children.14–17 These studies are briefly summarized in the supplemental material (Table S3).
In the Tucson Children's Assessment of Sleep Apnea (Tu-CASA) study, Goodwin and colleagues reported the results of HSAT use in 157 children, age 5 to 12 years.14 This study was part of a larger research study designed to investigate the prevalence and correlates of objectively measured sleep-disordered breathing in children. Technically acceptable studies, defined as more than 5 hours of interpretable respiratory, electroencephalography (EEG), and oximetry signals, were obtained in 91% of children on the first night and 97% of children when an additional night of testing was performed. Of note, only slightly more than half of the studies had acceptable airflow signals for at least 6 hours. More recently, Marcus and colleagues conducted a large multisite study to examine the clinical feasibility of HSATs to evaluate OSA in children.15 This study included 201 children, ages 5 to 12 years, all with a history of prematurity. Technically acceptable studies were obtained on the first night in 91% of the children and 98% when an additional study was performed. Although in both of these studies the HSAT was performed in a home environment, the recording equipment was placed by trained technologists. Of note, these were the only 2 studies that included EEG monitoring.
Brockman et al. evaluated the feasibility of unattended sleep studies comparing an HSAT performed at home (n = 75) versus in the hospital (n = 26) in 101 children, age newborn to 15 years.16 The sensors were placed by a trained nurse for all subjects. Technically acceptable recordings were obtained in 93% of subjects; the likelihood of a study being technically adequate was not influenced by whether the study was performed in the hospital or at home. In contrast, Poels and colleagues performed an HSAT in 24 children, ages 2 to 7 years in the home, with the sensors placed by caregivers after careful instruction.17 Defining a technically successful HSAT as at least 6.5 hours of total sleep time with artifact-free recording in at least 3 traces simultaneously, only 29% of their studies were classified as successful.17
In aggregate, these data suggest that an HSAT may be technically feasible in the pediatric population under carefully controlled conditions (eg, electrodes placed by a trained clinician). However, the likelihood of success may be significantly reduced if sensors are placed by caregivers instead of trained professionals or when more stringent criteria are used to define acceptable studies. Additional data examining the use of an HSAT in real-life settings with standardized recording channels and criteria for success is required to accurately determine feasibility of HSATs in children.
Validity of HSATs in Children
There are limited published data comparing HSATs to the gold standard of PSG in children. In the aforementioned feasibility studies, only 9 of 457 children had undergone PSG for comparison. In the study by Goodwin and colleagues, 5 children had PSG performed within 7 weeks of their HSAT. In these children no statistical differences were noted in the respiratory disturbance index (RDI) between the PSG and home studies.14 A small pilot study was performed prior to the larger multisite study to assess validity of the data.15 Four children underwent both PSG and an HSAT on separate nights within a 7-month period. Similar respiratory parameters were seen with the PSG and HSAT.
In addition, our literature search identified 5 further studies that compared an HSAT to PSG in children. Two studies involving 71 children compared results from HSATs done in the home to PSG.18,19 Two studies compared results from in-laboratory HSATs to PSG.20,21 Finally, a single study performed PSG and then transformed the data to include only that which would be available during an HSAT and compared the results.22 These studies are summarized in the supplemental material (Table S4).
Jacob and colleagues performed both an HSAT and PSG within 1 week in 21 children, ages 2 to 12 years, with a suspected diagnosis of OSA.18 Good correlation was seen between the 2 types of studies with reported sensitivity and specificity of 100% in children with more severe OSA (defined by the authors as AHI > 3).18 Alonso-Alvarez and colleagues compared an HSAT to simultaneously performed PSG and in-laboratory respiratory polygraphy in 50 children, ages 2 to 12 years, with clinical suspicion for OSA.19 Sensors were placed by nurses in the patients' homes for the HSAT. All studies were deemed valid (ie, there were no recordings with > 60% of uninterpretable flow signal). No significant differences were seen in total number of apneas or hypopneas between the HSAT and the PSG or in-laboratory respiratory polygraphy studies; however, there were significant differences in the total number of flow limitation events between the 3 types of studies leading to significant differences in both the RDI and obstructive RDI. For the HSAT, a higher sensitivity and specificity were achieved only when a higher obstructive RDI diagnostic cutoff (> 5) was used.
Two studies evaluated PSG with an HSAT done in a laboratory setting.20,21 Zucconi and colleagues evaluated 12 children, ages 3 to 6 years, with a high clinical suspicion of OSA with consecutive PSG and an unattended HSAT performed in a sleep laboratory.21 Comparisons were made between the respiratory indices on PSG and the HSAT scored both automatically and re-scored by hand using the automated scoring as a base. The sensitivity improved when the studies were hand-scored and a higher RDI diagnostic cutoff (> 10) was used but the specificity remained low. Lesser and colleagues evaluated 25 obese adolescents, ages 9 to 18 years, with suspected OSA by performing simultaneous PSG and HSATs in a laboratory setting.20 Sensitivity had minimal variation at all levels of disease severity but specificity improved only with increasing disease severity.
Finally, Tan and colleagues conducted a head-to-head study of 100 children ages 2 to 16 years, transforming PSG data into HSAT data by deletion of the EEG, electrocardiogram, and electromyogram channels. The data sets were then compared, which revealed that AHI was understated with the HSAT data set; this disparity could have significantly affected clinical management decisions in 23% of patients in the study, including 27.5% of patients with an AHI of 1 to 5 and 60% of patients with an AHI of 5 to 10.22
In total these validation studies report data from 208 children in whom the gold standard of PSG was directly compared with HSATs for the diagnosis of OSA9,10,14–18; however, an HSAT was only performed at home in 2 of the studies.18,19 Overall, these validation studies reported a relatively wide range of sensitivities and specificities that varied to some extent with severity of OSA.
In addition, using oximetry alone is not adequate for the identification of OSA in otherwise healthy children.13,23 Combining oximetry with a clinical score only identified approximately half of the children with OSA.24
Identifying Arousals and Hypoventilation
The AASM Scoring Manual identifies separate respiratory rules for the scoring of pediatric sleep studies.13 This includes the option to score a hypopnea if the event is associated with an arousal, rather than just a 3% oxygen desaturation, which requires EEG monitoring. The pediatric respiratory rules also recommend monitoring hypoventilation in children during a diagnostic study, which requires CO2 monitoring. An ideal HSAT would capture all of these parameters (see Table 1).
Table 1.
Ideal HSAT parameters.
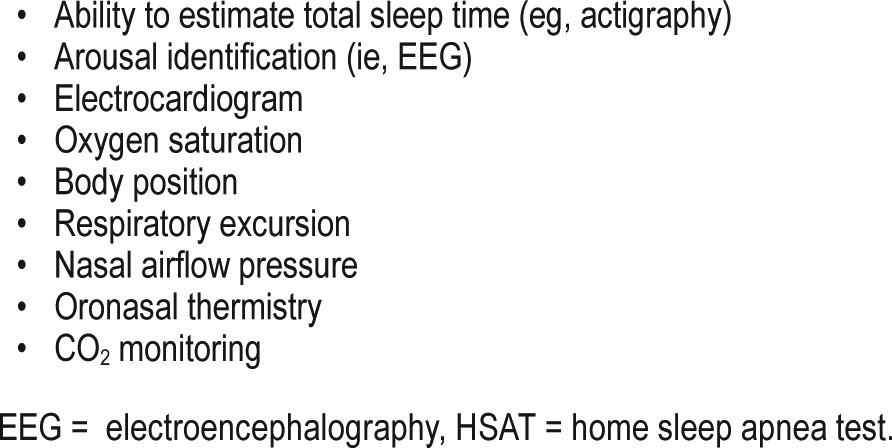
Only 2 of the studies described included EEG monitoring,14,15 and none of the studies included CO2 monitoring for the scoring of hypoventilation. In general, the devices used to perform an HSAT do not include EEG or end-tidal or transcutaneous CO2 monitoring and, therefore, are unable to score arousals or monitor hypoventilation. The lack of EEG and CO2 monitoring may result in significantly underestimating the presence and severity of disease in children, which may result in differing diagnoses and clinical management strategies in children using an HSAT, as compared to decisions based on PSG.22
Use of HSATs in Children With Comorbidities or Very Young Children
With the exception of Marcus and colleagues,15 none of the studies described previously to evaluate the feasibility or validity of HSATs included children with comorbid medical conditions. HSATs have been used in a few other small studies of children with comorbid conditions, but the validity and feasibility of the tests were not the focus of those reports.25–28 Finally, our review of the literature identified no validation studies for the use of HSATs in infants and young children (< 2 years old). These populations present unique challenges to diagnostic testing, and the consequences of misdiagnosing or underdiagnosing are potentially more severe. The lack of validation and feasibility testing in these populations contributed to the recommendation against using HSATs for the diagnosis of OSA in children.
Additional Challenges to HSATs
In addition to the paucity of literature supporting the use of HSATs in children, there are unique challenges associated with conducting HSATs in children that contributed to the position against its use. The body sizes of children can vary significantly, even within a narrow age range, and the cognitive and emotional maturity of children is less predictable than that of adult patients. This makes it difficult to identify patients who will be able to tolerate the numerous sensors that must be worn through the night.
In some situations, the caregiver's patience and motivation to complete the testing may be a limiting factor: a caregiver's aptitude to apply the sensors is a potential obstacle depending on the complexity of the HSAT. Without a sleep technologist monitoring the quality of the acquisition, the likelihood of inadequate test results is significantly higher, as demonstrated by Poels and colleagues.17
DISCUSSION AND FUTURE DIRECTIONS
In contrast to the recently published AASM clinical practice guideline on the diagnostic testing for adult OSA,3 an objective evaluation of the available literature does not support the use of HSATs for the diagnosis of OSA in children, due mostly to a lack of sufficient validation in the home, and insufficient monitoring available in most devices used to conduct an HSAT. The task force identified several areas for future research, including the need to define optimal physiologic parameters to be measured in individual patients, develop additional tools to assess sleep/wake status, validate an ideal HSAT device against PSG, create a diagnostic algorithm to identify ideal candidates for an HSAT, and establish appropriate alternatives to PSG. Each of these areas are briefly discussed in the following paragraphs.
Definition of Optimal Physiologic Parameters
The respiratory rules for the scoring of pediatric sleep studies identify multiple sensors that can be used for scoring apneas, hypopneas, and respiratory effort-related arousals. A primary focus of future research should be to better define the optimal physiologic parameters to be measured in individual patients for diagnosis. For example, more rigorous comparison of HSATs to PSG may identify which children are at risk of a falsely negative study due to isolated obstructive hypoventilation. If the prevalence of isolated obstructive hypoventilation is rare, and it is associated with identified predictive risk factors, CO2 monitoring would not be a priority for most children, making HSATs potentially more feasible.
Determining Total Sleep Time and Arousals
Because of the lower AHI used to diagnose pediatric OSA, sensors must be reliable for the entire night, as well as accurate in determining the percentage of time that a child is asleep. Most clinically used HSAT devices do not provide data regarding total sleep time. Future studies need to investigate the reliability of actigraphy or other testing so that there is an accurate denominator to calculate respiratory indices. Additionally, although arousals are currently measured by EEG, cardiac algorithms or peripheral arterial tonometry may potentially be a less invasive option to detect arousals, but this must be demonstrated.
Validation and Feasibility of an Ideal HSAT Device
The development of a device with the ideal HSAT parameters (described in Table 1) is not sufficient to warrant its use; any HSAT device must also be validated by direct comparison with PSG. If the comparison confirms that an HSAT device is equivalent to PSG, rigorous confirmation must be obtained in the home, under conditions that replicate how the device will be used in clinical practice. Future research should also identify any subpopulations where, despite the accuracy of the device, an HSAT is not feasible and should not be considered (eg, the caregiver is unwilling or incapable of successfully completing the test).
Development of a Diagnostic Algorithm
The development of an algorithm to predict the best candidates for a pediatric HSAT would significantly improve the reliability of the devices, and reduce the burden of false results in inappropriate candidates. There is currently no literature regarding how much HSAT data are sufficient for an accurate diagnosis. Therefore, future studies should monitor and report the percentage of time with poor signal quality, so that thresholds for acceptable test results can be determined. Publication of both positive and negative outcome studies is critical to facilitate the development of this algorithm, as a better understanding of factors associated with inadequate or failed HSAT will help optimize efficiency of care when choosing the most appropriate diagnostic method for a given patient and clinical situation.
Effect of HSAT Devices on Treatment Assessment and Patient-Important Outcomes
An accurate diagnosis is a prerequisite for successful treatment, but a diagnostic test should also be evaluated in conjunction with the effect that treatment has on clinical outcomes. Establishing an accurate diagnosis of OSA does not provide information about whether a child or group of children benefit from making treatment decisions based on the diagnosis. Therefore, any recommendations for using HSATs in children should be based on the diagnostic accuracy and feasibility of the device, and demonstration of improved patient-important outcomes when treatment decisions are based on HSAT results.29 Additionally, should future research demonstrate that diagnosis with an HSAT results in improved patient outcomes in children, its role may extend beyond the initial diagnosis of OSA if the aforementioned diagnostic criteria are met. For example, although most children treated surgically for OSA improve, many do not. Therefore, an easily accessed and administered HSAT device with proven accuracy could be used to identify those children requiring additional treatment and/or to assess the effectiveness of medical treatment.
Summary
In summary, data are currently insufficient to support using HSATs for the diagnosis of OSA in children. However, it is worthwhile to continue developing and validating HSAT devices for this population. Current barriers to undergoing PSG include factors related to (1) economics (eg, insurance deductible, parent time off of work), (2) access to care (eg, long wait, distance to facility, higher altitudes), and (3) social situations (eg, inconvenience, single parent). If an appropriate HSAT device could be shown to be a suitable alternative to PSG, it could potentially circumvent many of these barriers and improve the quality and efficiency of care for pediatric patients with OSA.
DISCLOSURE STATEMENT
The development of this position paper was funded by the American Academy of Sleep Medicine. The authors have indicated no financial conflicts of interest..
REFERENCES
- 1.Aurora RN, Zak RS, Karippot A, et al. Practice parameters for the respiratory indications for polysomnography in children. Sleep. 2011;34(3):379–388. doi: 10.1093/sleep/34.3.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aurora RN, Lamm CI, Zak RS, et al. Practice parameters for the non-respiratory indications for polysomnography and multiple sleep latency testing for children. Sleep. 2012;35(11):1467–1473. doi: 10.5665/sleep.2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi: 10.5664/jcsm.6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Standards and indications for cardiopulmonary sleep studies in children. American Thoracic Society. Am J Respir Crit Care Med. 1996;153(2):866–878. doi: 10.1164/ajrccm.153.2.8564147. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell RB, Kelly J. Outcome of adenotonsillectomy for severe obstructive sleep apnea in children. Int J Pediatr Otorhinolaryngol. 2004;68(11):1375–1379. doi: 10.1016/j.ijporl.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):576–584. doi: 10.1542/peds.2012-1671. [DOI] [PubMed] [Google Scholar]
- 7.Morton S, Rosen C, Larkin E, Tishler P, Aylor J, Redline S. Predictors of sleep-disordered breathing in children with a history of tonsillectomy and/or adenoidectomy. Sleep. 2001;24(7):823–829. doi: 10.1093/sleep/24.7.823. [DOI] [PubMed] [Google Scholar]
- 8.Gozal D, Capdevila OS, Kheirandish-Gozal L. Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med. 2008;177(10):1142–1149. doi: 10.1164/rccm.200711-1670OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gozal D, Kheirandish-Gozal L. Cardiovascular morbidity in obstructive sleep apnea: oxidative stress, inflammation, and much more. Am J Respir Crit Care Med. 2008;177(4):369–375. doi: 10.1164/rccm.200608-1190PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gozal D, Kheirandish-Gozal L, Bhattacharjee R, Spruyt K. Neurocognitive and endothelial dysfunction in children with obstructive sleep apnea. Pediatrics. 2010;126(5):e1161–e1167. doi: 10.1542/peds.2010-0688. [DOI] [PubMed] [Google Scholar]
- 11.Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714–e755. doi: 10.1542/peds.2012-1672. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 13.Berry RB, Brooks R, Gamaldo CE, et al. for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Darien, IL: American Academy of Sleep Medicine; 2016. Version 2.3. [Google Scholar]
- 14.Goodwin JL, Enright PL, Kaemingk KL, et al. Feasibility of using unattended polysomnography in children for research--report of the Tucson Children's Assessment of Sleep Apnea study (TuCASA) Sleep. 2001;24(8):937–944. doi: 10.1093/sleep/24.8.937. [DOI] [PubMed] [Google Scholar]
- 15.Marcus CL, Traylor J, Biggs SN, et al. Feasibility of comprehensive, unattended ambulatory polysomnography in school-aged children. J Clin Sleep Med. 2014;10(8):913–918. doi: 10.5664/jcsm.3970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brockmann PE, Perez JL, Moya A. Feasibility of unattended home polysomnography in children with sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2013;77(12):1960–1964. doi: 10.1016/j.ijporl.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Poels PJ, Schilder AG, van den Berg S, Hoes AW, Joosten KF. Evaluation of a new device for home cardiorespiratory recording in children. Arch Otolaryngol Head Neck Surg. 2003;129(12):1281–1284. doi: 10.1001/archotol.129.12.1281. [DOI] [PubMed] [Google Scholar]
- 18.Jacob SV, Morielli A, Mograss MA, Ducharme FM, Schloss MD, Brouillette RT. Home testing for pediatric obstructive sleep apnea syndrome secondary to adenotonsillar hypertrophy. Pediatr Pulmonol. 1995;20(4):241–252. doi: 10.1002/ppul.1950200407. [DOI] [PubMed] [Google Scholar]
- 19.Alonso-Alvarez ML, Teran-Santos J, Ordax Carbajo E, et al. Reliability of home respiratory polygraphy for the diagnosis of sleep apnea in children. Chest. 2015;147(4):1020–1028. doi: 10.1378/chest.14-1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lesser DJ, Haddad GG, Bush RA, Pian MS. The utility of a portable recording device for screening of obstructive sleep apnea in obese adolescents. J Clin Sleep Med. 2012;8(3):271–277. doi: 10.5664/jcsm.1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zucconi M, Calori G, Castronovo V, Ferini-Strambi L. Respiratory monitoring by means of an unattended device in children with suspected uncomplicated obstructive sleep apnea: a validation study. Chest. 2003;124(2):602–607. doi: 10.1378/chest.124.2.602. [DOI] [PubMed] [Google Scholar]
- 22.Tan HL, Gozal D, Ramirez HM, Bandla HP, Kheirandish-Gozal L. Overnight polysomnography versus respiratory polygraphy in the diagnosis of pediatric obstructive sleep apnea. Sleep. 2014;37(2):255–260. doi: 10.5665/sleep.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirk VG, Bohn SG, Flemons WW, Remmers JE. Comparison of home oximetry monitoring with laboratory polysomnography in children. Chest. 2003;124(5):1702–1708. doi: 10.1378/chest.124.5.1702. [DOI] [PubMed] [Google Scholar]
- 24.Villa MP, Pietropaoli N, Supino MC, et al. Diagnosis of pediatric obstructive sleep apnea syndrome in settings with limited resources. JAMA Otolaryngol Head Neck Surg. 2015;141(11):990–996. doi: 10.1001/jamaoto.2015.2354. [DOI] [PubMed] [Google Scholar]
- 25.Marcus CL, Moore RH, Rosen CL, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368(25):2366–2376. doi: 10.1056/NEJMoa1215881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kasapkara CS, Tumer L, Aslan AT, et al. Home sleep study characteristics in patients with mucopolysaccharidosis. Sleep Breath. 2014;18(1):143–149. doi: 10.1007/s11325-013-0862-z. [DOI] [PubMed] [Google Scholar]
- 27.Jheeta S, McGowan M, Hadjikoumi I. Is oximetry an effective screening tool for obstructive sleep apnoea in children with Down syndrome? Arch Dis Child. 2013;98(2):164. doi: 10.1136/archdischild-2012-302932. [DOI] [PubMed] [Google Scholar]
- 28.Bannink N, Mathijssen IM, Joosten KF. Use of ambulatory polysomnography in children with syndromic craniosynostosis. J Craniofac Surg. 2010;21(5):1365–1368. doi: 10.1097/SCS.0b013e3181ec69a5. [DOI] [PubMed] [Google Scholar]
- 29.Hsu J, Brożek JL, Terracciano L, et al. Application of GRADE: making evidence-based recommendations about diagnostic tests in clinical practice guidelines. Implement Sci. 2011;6:62. doi: 10.1186/1748-5908-6-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


