Abstract
Background
Depression and anxiety are common in stroke survivors as well as their family caregivers. However, it is not known whether each person’s emotional distress contributes to their partner’s quality of life (QOL).
Objective
This study aimed to examine the effect of depression and anxiety on QOL in stroke survivor-caregiver dyads using dyadic analysis technique - the Actor-Partner Interdependence Model (APIM).
Methods
This was a cross-sectional pilot study with a total of 30 participating dyads (30 stroke survivors and 30 family caregivers) from Hospital Rehabilitasi Cheras, Kuala Lumpur, Malaysia. This pilot study was conducted over a period of 3 months, between December 2014 and February 2015. Depression and anxiety were assessed using the Hospital Anxiety and Depression Scale (HADS). QOL was assessed using the Short Form-12 Health Survey (SF-12). All analyses were carried out using IBM SPSS version 22. Dyadic data were analysed using multilevel modelling (MLM).
Results
Depression was uniquely associated with an individual’s own QOL. Survivors and caregivers with higher depression had poorer physical component summary (PCS) scores and mental component summary (MCS) scores. Stroke survivor’s depression exerted a significant actor effect on their PCS (b=−1.42, p=0.001) and MCS (b=−1.52, p<0.001). Caregiver’s depression exerted a significant actor effect on their PCS (b=−2.53, p<0.001) and MCS (b=−1.51, p=0.004). Caregivers’ anxiety negatively influenced their own MCS (b=−0.58, p=0.031). Furthermore, depression exerted a significant partner effect on PCS in stroke survivors (b=−1.19, p=0.003). Caregivers’ depression was also related to their stroke survivors’ poorer QOL, particularly PCS.
Conclusion
The findings suggest that depression affects the QOL of both stroke survivors and caregivers, not only emotionally but also physically. This dyadic study also has evidence pointing to depression in caregivers and its association with stroke survivors’ physical QOL.
Keywords: Malaysia, Quality of life, Stroke, Anxiety, Depression, Caregivers
1. Introduction
Stroke is a leading cause of long-term disability and the majority of stroke survivors rely on family caregivers to assist with activities of daily living. Globally, approximately 16.9 million people suffer from stroke annually and 5.9 million are fatal (1). Among those who survive, almost 60% of patients remain disabled (2). In Malaysia, age-adjusted incidence rates of ischemic and hemorrhagic stroke were 96/100,000 and 21/100,000 in 2014 (3). It was estimated that Malaysia had 52,000 cases of hospitalization for strokes annually (4) and 8.4% of 48,091 deaths in government hospitals in 2009 (5). The resulting impairments after a stroke can affect both stroke survivors and caregivers, and reported elevated levels of depression and anxiety. Previous studies have shown prevalence of depression among stroke survivors were at rates of 33%–44% (6, 7); the results vary due to difference in time measured after stroke. Post-stroke anxiety was reported to range from 20% to 25% (8, 9). Depression and anxiety symptoms are associated with poorer quality of life (QOL), slower functional recovery and mortality (10). The prevalence of anxiety and depression are high in stroke survivors, mental health problems following stroke are an equal or even greater problem for their family caregivers (11). Up to 52% of stroke caregivers have been reported to experience depression during caregiving periods (12). Several studies have found that the stroke survivors and family caregivers mutually influenced each other’s depressive symptoms (11, 13, 14). Stroke survivors’ distress, negatively affect caregivers’ emotional state, while caregivers’ depressive symptoms influence post-stroke depression (13). Although stroke research has found that depression of survivors and caregivers is interdependent (14, 15), little attention has been given to the statistical analyses that control this interdependence within stroke dyads. QOL is an important outcome measure in patients with stroke. Stroke rehabilitation outcomes do not only aim to restore or promote optimal physical function, but also optimal QOL, as it covers patient’s perspectives on physical, mental, and social health (11, 15). The assessment of QOL in stroke survivors and caregivers can provide a better understanding of the subjective state of health which quantifies the impact of stroke on an individual’s life, such as impairment of physical health status, disruption of social participation, disruption in family relationships, and decreased psychological well-being (10). A longitudinal dyadic analysis study of stroke survivor and caregiver dyads have been reported as improving QOL in caregivers over one year of rehabilitation associated with increases in survivor physical functioning and QOL (15). On the other hand, caregivers QOL were significantly affected by the psychological distress of stroke survivors. Separate regression analyses for the stroke survivor and caregiver, found depression was associated with mental QOL for both caregivers and stroke survivors (16). Although the evidence suggests associations of QOL between survivors and caregivers (11), the analysis compared outcomes in separate patient and caregiver groups, implying that the researchers often consider and analyze the dyadic data as independent rather than interdependent.
Until now, not much attention has been paid, in the stroke literature to the dyadic effects of stroke survivors’ and caregivers’ anxiety and depression on stroke survivors’ and caregivers’ QOL. The Actor-Partner Interdependence Model (APIM) is most often used in dyadic data analysis, which uses dyad as the unit of analysis (17). This model suggests that a person’s predictor variable that affects his or her own outcome variable is called an actor effect. A partner effect occurs when a person’s score on a predictor variable affects his or her partner’s score on an outcome variable (17). The partner effect from the APIM, measure the interdependence that may occur between individuals in a dyadic relationship. Stroke survivors and their family caregivers have an interdependent relationship because they share their thoughts and feelings, give and receive support from each other after stroke. This is an important gap in our knowledge of the relation of one person’s depression or anxiety to a partner’s QOL. Because no studies have investigated whether stroke survivors’ and caregivers’ anxiety and depression contribute to the survivors’ own and their partners’ QOL, this study utilized small samples for the purpose of exploring the dyadic association as a pilot study. This current study aimed to examine the effect of depression and anxiety on QOL (i.e., physical component summary [PCS] and mental component summary [MCS]) in stroke survivor-caregiver dyads using dyadic analysis technique, APIM. In this study, actor effects refer to the extent to which the depression and anxiety of one member of survivor-caregiver dyads are associated with QOL of the same member of the dyads (i.e., relationship between anxiety and PCS among stroke survivors). Moreover, partner effects refer to the extent to which depression and anxiety of one member of survivor-caregiver dyads are associated with the QOL of the other member of the dyads (i.e., relationship between stroke survivors’ anxiety and their caregivers’ PCS).
2. Material and Methods
2.1. Research design and participants
The study used a descriptive and cross-sectional pilot study. Participants were recruited and assessed at the neurology outpatient clinic at Hospital Rehabilitasi Cheras, Kuala Lumpur, Malaysia. This pilot study was conducted over a period of three months, between December 2014 and February 2015. Hospital Rehabilitasi Cheras located at Kuala Lumpur, Malaysia, was chosen as it is the first comprehensive rehabilitation hospital in Malaysia. The inclusion criteria for the stroke survivors were: aged 18 years or older, stroke diagnosed by a neurologist, were medically stable, able to respond to study questions, and had an adult family caregiver. The exclusion criteria were as follows: had a severe psychiatric disorder, had an acute disorder such as cancer or tumors or surgical operation in the past four weeks, and having language deficit or severe cognitive deficit due to stroke as measured by Mini Mental State Examination (MMSE < 17) (18). Sampled caregivers were only those who provide structured care voluntarily and for free to the stroke survivor. Eligible caregivers included adults who met the following criteria: aged 18 years or older, living with a stroke survivor, being the partner, adult child, parent, or relative of stroke survivor, and not diagnosed with stroke. A total of 30 stroke survivor and caregiver dyads completed the survey and participated in this study. Participants were approached for enrollment into the study while they were waiting to see a doctor. The researcher met, explained, and invited patients to participate in this study. Stroke survivors were asked to identify an acquaintance who was considered his or her informal caregiver. Participants were requested to sign an informal consent form. Data were collected through face-to-face interview using a pre-tested questionnaire. The study was approved by the Universiti Putra Malaysia Ethics Committee for Research Involving Human Subjects (JKEUPM) and the Medical Research and Ethics Committee (MREC), Ministry of Health, Malaysia.
2.2. Measures
The Short Form-12 Health Survey (SF-12) was used to assess QOL for both stroke survivors and caregivers. The SF-12 components have been shown to be a valid, reliable and responsiveness measure of QOL in stroke patients and caregivers (19). It covers both physical and mental concepts, as well as social aspect. This 12-item instrument contains two summary scores: the physical component summary (PCS) and mental component summary (MCS) scores (20). Both PCS and MCS scores range from 0 to 100, representing worst to best health. The SF-12 has been translated into Malay language and validated in postpartum mothers. The Malay version of SF-12 has been reported as having good validity and reliability with Cronbach’s alpha estimates of 0.70 for MCS and 0.75 for PCS (21). The Hospital Anxiety and Depression Scale (HADS) is a screening tool for measuring the severity of emotional disorder. The HADS consists of 14 items and two subscales: anxiety and depression. This measure is widely used in stroke research, and Bjelland et al. (2002) reported good test-retest reliability (22). The measure uses a 4-point Likert scale, with higher scores indicating more distress. The HADS has been translated and validated in Malaysian caregiver samples (23). Socio-demographic and clinical characteristics of stroke survivors and caregivers were also collected, such as age, gender, ethnicity, marital status, educational level, employment status, monthly household income, and relationship between caregiver and stroke survivor. The information obtained on stroke survivors’ health conditions were type of stroke, years since diagnosis, stroke severity, and physical functional level. Stroke severity was measured by the modified Rankin Scale (mRS). The scale describes six grades of disability after a stroke, from 0 to 5, with 0 denoting no symptoms at all and 5 denoting severe disability or bedridden. The Barthel Index (BI) was used to assess daily function status and independency in 10 activities: bowel, bladder, grooming, toilet use, feeding, transfer, mobility, dressing, steps, and bathing. Each item was rated and overall score was calculated to determine functional independence. Scores ranged from 0 to 100, with higher scores indicating greater independence. The BI has been reported as good validity and reliability in stroke research (24).
2.3. Data analyses
All analyses were conducted using IBM SPSS version 22. An alpha level of 0.05 was used to determine statistical significance. Descriptive statistics were conducted to describe the characteristics of dyad members. Paired-sample t-test was used to compare the mean differences in variables between caregivers and survivors. Pearson correlation was used to test the bivariate associations among variables. To assess the proposed APIM model for the effect of survivors and caregivers on one another, the multi-level modeling (MLM) analysis technique was conducted. The survivor-caregiver dyads are considered distinguishable, in which dyad members are distinguishable by their roles after stroke (i.e., caregiver and care-recipient). The survivor-caregiver dyads were used as the unit of analysis. MLM treats members of a dyad as nested scores within the same group. A detailed description on how to conduct the APIM analyses using MLM has previously been outlined, and served as the guide for this analysis (17).
3. Results
3.1. Characteristics of survivor-caregiver dyad
A total of 30 dyads (30 stroke survivors and 30 caregivers) participated in this study (Table 1). The sample consisted of 46.7% men and 53.3% women with a mean age of 48.0±15.3 years. The mean age of stroke survivors (49.0±16.5 years) was slightly higher than that of caregivers (47.0±14.1 years). Most caregivers (96.7%) and stroke survivors (70.0%) had at least secondary education. There were 38 Malays (63.4%), 14 Chinese (23.3%) and 8 Indians (13.3%). Most caregivers were married (66.7%), employed (63.4%), and in low income groups (<RM 3000, 46.7%). Of caregivers, 40% were spouses. Stroke survivors were predominantly ischemic stroke (93.3%), more men (66.7%) than women and were retired or unemployed (86.7%). Around 43% of the stroke survivors were diagnosed with moderate disability, 26.7% moderate severe disability, 23.3% severe disability, while the remaining 6.7% slight disability. The average of post-stroke duration was almost 3 years.
Table 1.
Characteristics of Participants
| Variables | Total (n=60) | Caregivers (n=30) | Survivors (n=30) | |
|---|---|---|---|---|
| n (%)/Mean±SD | n (%)/Mean±SD | n (%)/Mean±SD | ||
| Age (years) | 47.98±15.25 | 47.00±14.09 | 48.97±16.52 | |
| Gender | Male | 28 (46.7) | 8 (26.7) | 20 (66.7) |
| Female | 32 (53.3) | 22 (73.3) | 10 (33.3) | |
| Education | Primary | 10 (16.7) | 1 (3.3) | 9 (30.0) |
| Secondary | 36 (60.0) | 22 (73.4) | 14 (46.7) | |
| Tertiary | 14 (23.3) | 7 (23.3) | 7 (23.3) | |
| Ethnicity | Malay | 38 (63.4) | 19 (63.4) | 19 (63.4) |
| Chinese | 14 (23.3) | 7 (23.3) | 7 (23.3) | |
| Indian | 8 (13.3) | 4 (13.3) | 4 (13.3) | |
| Marital status | Single | 16 (26.7) | 9 (30.0) | 7 (23.3) |
| Married | 40 (66.7) | 20 (66.7) | 20 (66.7) | |
| Others (widowed, divorced) | 4 (6.7) | 1 (3.3) | 3 (10.0) | |
| Employment status | Employed | 23 (38.3) | 19 (63.4) | 4 (13.3) |
| Unemployed | 37 (61.7) | 11 (36.6) | 26 (86.7) | |
| Monthly household income | <RM 3000 | 14 (46.7) | ||
| RM 3000–5000 | 11 (36.7) | |||
| >RM 5000 | 5 (16.7) | |||
| Relationship between caregiver and survivor | Spouses | 12 (40.0) | ||
| Daughter/son | 5 (16.7) | |||
| Brother/sister | 8 (26.7) | |||
| Parents | 5 (16.6) | |||
| Barthel index | 62.00±26.15 | |||
| Stroke severity (mRS) | 2-Slight disability | 2 (6.7) | ||
| 3-moderate disability | 13 (43.3) | |||
| 4-moderate severe disability | 8 (26.7) | |||
| 5-severe disability | 7 (23.3) | |||
| Type of Injury | Ischemic | 28 (93.3) | ||
| Hemorrhagic | 2 (6.7) | |||
| Years since diagnosis | 2.78±3.32 | |||
Abbreviations: RM, Ringgit Malaysia; SD, standard deviation
Notes: 1 RM = 0.23 USD
3.2. Comparing stroke survivors and caregivers in depression, anxiety and quality of life
Comparisons between stroke survivors and caregivers revealed significant differences in PCS and MCS (Table 2). The anxiety and depression were similar between dyad members. Stroke survivors reported worse PCS and MCS than caregivers. MCS score of stroke survivors and their caregivers were significantly positively correlated (r=0.424, p=0.019).
Table 2.
Comparisons of Study Variables between Caregivers and Survivors (N=60)
| Variables | Caregivers; Mean±SD | Survivors; Mean±SD | t | p* | r | p** |
|---|---|---|---|---|---|---|
| Anxiety | 5.03±3.85 | 6.40±3.84 | −1.63 | 0.113 | 0.289 | 0.122 |
| Depression | 5.67±4.46 | 6.83±4.19 | −1.29 | 0.208 | 0.344 | 0.063 |
| PCS | 41.57±6.09 | 32.11±6.71 | 6.45 | 0.0001 | 0.215 | 0.253 |
| MCS | 48.36±12.46 | 41.07±10.74 | 3.19 | 0.003 | 0.424 | 0.019 |
Abbreviations: MCS, mental component summary; PCS, physical component summary; SD, standard deviation; t, paired t-test value; r, Pearson correlation value. Notes: p*, significance level of t; p**, significance level of r
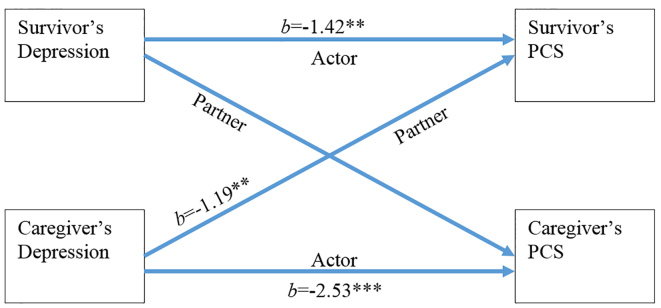
3.3. The effects of anxiety and depression on PCS
In the MLM analysis, the actor and partner effects of anxiety and depression on reported PCS and MCS scores were estimated. The predictor variables in the model include the actor and partner scores on both anxiety and depression, while PCS and MCS scores served as the dependent variables in this analysis. As an example, APIM was used to investigate the effect of depression on PCS (Figure 1), the actor effect of depression for the survivor was the degree to which the survivor’s depression predicted the survivor’s PCS. The partner effect for the survivor was the degree to which the caregiver’s depression predicted the survivor’s PCS. Similarly, the actor effect for the caregiver was the degree to which the caregiver’s depression predicted his or her own PCS, and the partner effect for caregiver was the degree to which the survivor’s depression predicted the caregiver’s PCS. The detailed results of MLM analyses are presented in Table 3, and only significant findings of APIM are shown in the Figures 1 and 2. Results indicated no significant effects for actor or partner anxiety on PCS score for both survivors and caregivers (all p>0.05). For stroke survivors, depression exerted a significant actor effect on PCS (b=−1.42, p=0.001). A one-unit increase in stroke survivor’s depression was associated with a 1.42-unit decrease in their PCS. There was a significant partner effect of depression on PCS by stroke survivors (b=−1.19, p=0.003), suggesting that stroke survivors whose caregivers had higher levels of depression were more likely to have lower PCS scores. Every one-unit increase in caregiver’s depression was associated with a 1.19-unit decrease in stroke survivors’ PCS score. The effects of actor depression were significantly related to PCS score (b=−2.53, p<0.001) in caregivers, showing that caregivers who had higher depression reported lower PCS scores. For caregivers, a one-unit increase in depression was associated with a 2.53-unit decrease in PCS score. A partner effect of depression on PCS in caregivers, however, did not exist (b=0.308, p=0.475). Thus, stroke survivors and caregivers with higher depression had poorer PCS. Only caregivers’ depression had a significant partner effect on survivors’ PCS. However, survivors’ depression did not predict caregivers’ PCS.
Figure 1.
The actor and partner effects of depression on PCS (PCS, physical component summary; *p<0.05, **p<0.01, ***p<0.001)
Table 3.
Actor and Partner Effects on QOL
| Predictors | Survivors | Caregivers | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | t | p | b | SE | t | p | ||
| Physical component summary | Anxiety | ||||||||
| Actor | −0.129 | 0.344 | −0.374 | 0.711 | −0.517 | 0.3.2 | −1.716 | 0.098 | |
| Partner | −0.287 | 0.344 | −0.834 | 0.412 | 0.050 | 0.302 | 0.166 | 0.870 | |
| Depression | |||||||||
| Actor | −1.421 | 0.371 | −3.830 | 0.001 | −2.527 | 0.425 | −5.953 | 0.0001 | |
| Partner | −1.193 | 0.370 | −3.222 | 0.003 | 0.308 | 0.425 | 0.725 | 0.475 | |
| Mental component summary | Anxiety | ||||||||
| Actor | −0.385 | 0.313 | −1.232 | 0.228 | −0.583 | 0.255 | −2.283 | 0.031 | |
| Partner | −0.171 | 0.294 | −0.580 | 0.567 | 0.097 | 0.271 | 0.359 | 0.722 | |
| Depression | |||||||||
| Actor | −1.518 | 0.372 | −4.077 | 0.0001 | −1.512 | 0.477 | −3.171 | 0.004 | |
| Partner | −0.551 | 0.350 | −1.574 | 0.127 | −0.096 | 0.507 | −0.190 | 0.851 | |
Abbreviations: b, unstandardized regression coefficient; SE, standard error
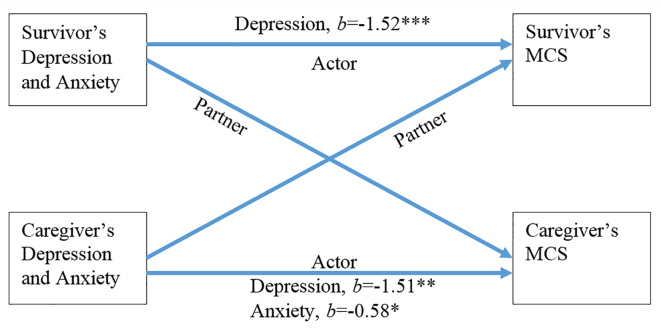
Figure 2.
The actor and partner effects of depression and anxiety on MCS (MCS, mental component summary; *p<0.05, **p<0.01, ***p<0.001)
3.4. The effects of anxiety and depression on MCS
In the survivors’ MCS dimension, survivors’ actor and partner effects of anxiety on MCS were not observed (all p>0.05). A significant anxiety actor effect emerged in stroke caregivers (b=−0.58, p=0.031), suggesting that greater anxiety in stroke caregivers was related to a decrease of their own MCS scores. Every one-unit increase in anxiety was associated with a 0.58-unit decrease in stroke caregivers’ MCS score. However, no significant relation between partner anxiety and MCS for caregivers were observed (b=0.097, p=0.722). Also, as predicted, depression exhibited only actor effects for survivors in MCS (b=−1.52, p<0.001). One-unit increase in stroke survivors’ depression was associated with a 1.52-unit decrease in their MCS. Although survivors exhibited significant actor effect for depression, partner effects of depression on MCS score was not significant (b=−0.55, p=0.127). For caregivers, a significant actor effect emerged for depression, showing that more depressive caregivers also reported lower MCS scores (b=−1.51, p=0.004). A one-unit increase in depression was associated with a 1.51-unit decrease in MCS score. Again, no significant partner effect for depression emerged on MCS for caregivers (b=−0.096, p=0.851).
4. Discussion
Both stroke survivors and their caregivers experienced depression and anxiety. The high levels of depression and anxiety were consistent with findings reported in previous studies (6, 13, 14, 16). Furthermore, anxiety and depression scores of stroke survivors and their caregivers were comparable (6). This suggests that the emotional aspects of dealing with stroke may affect caregivers as much as the patients with stroke. The results of the study were inconsistent with a prior report that stroke caregivers observed significantly higher mean anxiety and depression scores than stroke survivors (16) and a study suggesting stroke survivors had higher depressive symptoms and anxiety levels than those of their caregivers (6). The different anxiety and depression scores across studies could be due to different methods, particularly sampling and assessment in the previous studies, and the different social, cultural, and geographical aspects utilized in each study. Similar to those in a study of heart failure patients and spousal caregivers, Chung et al. (2009) observed both patients and caregivers had similar depressive and anxiety levels (25). A plausible explanation for the similarity levels of anxiety and depression among stroke survivors and caregivers is that the influences of distress may occur through the process of emotional contagion (26); in which people tend to catch others’ emotions and moods through unconscious interaction processes. It is possible that anxiety or depression are easily transmitted from one person of the dyad to another person of the dyad. The caregiver’s anxiety and depression levels can be shared by their close relationship partner and family members (27). The QOL scores for stroke survivors were significantly lower than caregivers. Similar to other studies, stroke caregivers reported higher QOL than survivors at 2.5 years post-stroke (28). However, Morimoto et al. have shown 63% of stroke survivors with good QOL while 42% of caregivers reported good QOL (12). In addition, comparing caregivers’ QOL population norms, several studies have reported that caregivers rated lower levels in all QOL domains (16). Caring for a stroke patient with more impaired functioning and finding caregiving burdensome adversely affect QOL of caregivers (15, 29, 30). In our study, we found MCS were correlated between stroke survivors and caregivers. The findings extend our current knowledge about the psychological impact that stroke can bring on, not only to patients but also to their family caregivers. Therefore, healthcare professionals caring for individuals following a stroke should be mindful of those caregivers likely to be most affected and implement strategies to support them in their role in order to reduce caregiver burden and improve psychosocial outcomes in stroke patients and their caregivers.
In this dyadic study, we have examined the effects of anxiety and depressive symptoms on QOL, particularly physical and mental health in family members dealing with stroke. The caregiver’s own anxiety symptoms (actor effect), was a significant predictor of their own MCS scores. Similarly, Chung et al. reported lower caregiver anxiety increase QOL for caregivers of heart failure (25). On the other hand, results of a study by Fatoye et al. (2006) indicated that, family caregivers of stroke were more likely to experience emotional problems and deterioration of QOL (16). However, they did not observe any relationship between caregivers’ anxiety and QOL. The inconsistent findings could be due to differences in QOL instruments; Fatoye and colleagues utilized the short version of the World Health Organization Quality of life instrument (WHOQOL-BREF) and four QOL domains were measured (physical health, psychological health, social relationship and environment), whereas SF-12 were used in this study. Anxiety is common in stroke caregivers and related to unpreparedness of caregiving tasks at home, concerns about the future, fear of recurrence, long term recovery process, and financial difficulties. Such distressed state can lead to caregiving burden and burnout of caregivers. These factors directly influence QOL in caregivers, especially decline of mental health scores (31). This study found that stroke survivors’ and caregivers’ depressive symptoms were associated with their own QOL, consistent with the results of previous studies (10, 31, 32). This implies that depressed individuals who rated lower QOL included physical and mental health. This is consistent with other studies that reported higher stress in stroke survivors were associated with poorer function, perceived that their health was poor, and felt that they were making a poor recovery from stroke, hence poorer physical and mental health (10). Caregivers’ depression was associated with their general health. The majority of caregivers reported their health as ‘poor or fair’ after engaging in caregiving duties (33). Additionally, caregivers with depressive symptoms may neglect their own health and increased risk of chronic diseases such as, diabetes mellitus, gynecological problems and backaches.
There was evidence of partner effects in this study. Caregivers’ greater depressive symptoms were significantly related to poorer physical health of their survivors’ QOL. It is noteworthy that the adverse effect of having a partner who is depressed is limited to the survivor’s physical health, but not vice versa. This finding is congruent with the literature on stroke caregivers’ depression and has been correlated with negative stroke survivor outcomes, especially functional recovery (34). However, other researchers found no correlation between caregiver’s strain and patient’s physical level (35). It is possible that the difference in the findings can be attributed to intervening variables such as the quality of the relationship between the patient and caregiver and the stroke survivor’s stress level (36). The results of this study highlight the impact of negative caregiving on stroke survivors’ physical health. This is possibly due to the fact that stroke survivors’ recovery depends on caregivers’ help in daily activities. Our findings add support to the literature on interdependence of the caregiving relationships and the interpersonal QOL of stroke survivors and their caregivers.
5. Limitations
The current study has a number of methodological limitations that should be noted. First, the cross-sectional study design, limits conclusions regarding the direction of relationship between depression and QOL. Second, all variables were self-reported and may not reflect objective depression and health status. Future studies should include behavioral and psychological indicators of depression and QOL. Third, the small sample size and only one study location could limit the generalization of study findings to stroke patients and caregivers or to Malaysian populations. Finally, the present study did not examine other important determinants of dyads’ stroke experience, such as characteristics of patients and caregivers, caregiving burden and appraisals, and social supports that may affect the QOL. Despite these limitations, the findings add important information related to the QOL of stroke patients and their family caregivers. Our findings suggest that when a family is dealing with a stroke, caregiver’s depressive symptoms play a key role not only in their own but their partners’ well-being. Thus, both stroke survivors and caregivers should be considered as a dyadic unit by health professionals and researchers, as they are interdependent in their relationship. Future interventions should include both stroke survivors and their caregivers that focus on support and care which can improve QOL for stroke survivors and family member dyads.
6. Conclusions
Results suggest that depression affects the QOL of both stroke survivors and caregivers, not only emotionally but also physically. This dyadic study also has evidence pointing to depression in caregivers and its association with stroke survivors’ physical QOL. It emphasizes the necessity for arranging interventions targeting both stroke survivors and family caregivers to enhance their QOL in the rehabilitation process. Dyad interventions focused on psycho-education and skill-building strategies are designed to reduce anxiety and depressive symptoms for both stroke survivors and caregivers.
Acknowledgments
This study is supported by Fundamental Research Grant Scheme (FRGS) of the Ministry of Higher Education Malaysia and Universiti Putra Malaysia (FRGS/1/2015/SKK06/UPM/01/1). Acknowledgement and gratitude are also accorded to directors, heads of departments and staff of Hospital Rehabilitasi Cheras, for their cooperation and assistance. To the participants, sincere thanks are recorded.
Footnotes
iThenticate screening: July 09, 2017, English editing: August 12, 2017, Quality control: August 14, 2017
This article has been reviewed/commented by four experts
Conflict of Interest:
There is no conflict of interest to be declared.
Authors’ contributions:
All authors contributed to this project and article equally. All authors read and approved the final manuscript.
References
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245–54. doi: 10.1016/S0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scherbakov N, Doehner W. Sarcopenia in stroke-facts and numbers on muscle loss accounting for disability after stroke. J Cachexia Sarcopenia Muscle. 2011;2(1):5–8. doi: 10.1007/s13539-011-0024-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aziz ZA, Lee YY, Ngah BA, Sidek NN, Looi I, Hanip MR, et al. Acute Stroke Registry Malaysia, 2010–2014: Results from the National Neurology Registry. J Stroke Cerebrovasc Dis. 2015;24(12):2701–9. doi: 10.1016/j.jstrokecerebrovasdis.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 4.Krishnamoorthy M. Killer stroke: Six Malaysians hit every hour. The Star. 2007. Nation. Available from: http://www.thestar.com.my/story/?file=%2F2007%2F4%2F24%2Fnation%2F17524877.
- 5.Ministry of Health M. Health Facts 2009. Malaysia: Health Information Centre, Planning and Development Division; 2010. [Google Scholar]
- 6.Balhara YP, Verma R, Sharma S, Mathur S. A study of predictors of anxiety and depression among stroke patient-caregivers. J Midlife Health. 2012;3(1):31–5. doi: 10.4103/0976-7800.98815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330–40. doi: 10.1161/01.str.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- 8.Campbell Burton CA, Murray J, Holmes J, Astin F, Greenwood D, Knapp P. Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int J Stroke. 2013;8(7):545–59. doi: 10.1111/j.1747-4949.2012.00906.x. [DOI] [PubMed] [Google Scholar]
- 9.Tang WK, Lau CG, Mok V, Ungvari GS, Wong KS. Impact of anxiety on health-related quality of life after stroke: a cross-sectional study. Arch Phys Med Rehabil. 2013;94(12):2535–41. doi: 10.1016/j.apmr.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis. 2009;27(Suppl 1):204–14. doi: 10.1159/000200461. [DOI] [PubMed] [Google Scholar]
- 11.Godwin KM, Ostwald SK, Cron SG, Wasserman J. Long-term health-related quality of life of stroke survivors and their spousal caregivers. J Neurosci Nurs. 2013;45(3):147–54. doi: 10.1097/JNN.0b013e31828a410b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morimoto T, Schreiner AS, Asano H. Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age Ageing. 2003;32(2):218–23. doi: 10.1093/ageing/32.2.218. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy MJ, Lyons KS, Powers LE. Expanding poststroke depression research: movement toward a dyadic perspective. Top Stroke Rehabil. 2011;18(5):450–60. doi: 10.1310/tsr1805-450. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy MJ, Lyons KS, Powers LE. Relational factors associated with depressive symptoms among stroke survivor-spouse dyads. J Fam Soc Work. 2012;15(4):303–20. doi: 10.1080/10522158.2012.696230. [DOI] [Google Scholar]
- 15.Pucciarelli G, Vellone E, Savini S, Simeone S, Ausili D, Alvaro R, et al. Roles of Changing Physical Function and Caregiver Burden on Quality of Life in Stroke: A Longitudinal Dyadic Analysis. Stroke. 2017;48(3):733–9. doi: 10.1161/strokeaha.116.014989. [DOI] [PubMed] [Google Scholar]
- 16.Fatoye FO, Komolafe MA, Adewuya AO, Fatoye GK. Emotional distress and self-reported quality of life among primary caregivers of stroke survivors in Nigeria. East Afr Med J. 2006;83(5):271–9. doi: 10.4314/eamj.v83i5.9433. [DOI] [PubMed] [Google Scholar]
- 17.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. p. 458. [Google Scholar]
- 18.Zarina Z, Zahiruddin O, AH CW. Validation of Malay mini mental state examination. Malaysian Journal of Psychiatry. 2007;16(1):16–9. [Google Scholar]
- 19.Pickard AS, Johnson JA, Penn A, Lau F, Noseworthy T. Replicability of SF-36 summary scores by the SF-12 in stroke patients. Stroke. 1999;30(6):1213–7. doi: 10.1161/01.STR.30.6.1213. [DOI] [PubMed] [Google Scholar]
- 20.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Noor NM, Aziz AA. Validity and reliability of the Malay version of 12-item short form health survey among postpartum mothers. Malaysian Journal of Public Health Medicine. 2014;14(2):56–66. [Google Scholar]
- 22.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 23.Yusoff N, Low WY, Yip CH. Psychometric properties of the Malay Version of the hospital anxiety and depression scale: a study of husbands of breast cancer patients in Kuala Lumpur, Malaysia. Asian Pac J Cancer Prev. 2011;12(4):915–7. [PubMed] [Google Scholar]
- 24.Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials: development, properties, and application. Stroke. 2011;42(4):1146–51. doi: 10.1161/strokeaha.110.598540. [DOI] [PubMed] [Google Scholar]
- 25.Chung ML, Moser DK, Lennie TA, Rayens MK. The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: testing dyadic dynamics using Actor-Partner Interdependence Model. J Psychosom Res. 2009;67(1):29–35. doi: 10.1016/j.jpsychores.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hatfield E, Cacioppo JT, Rapson RL. Emotional contagion. Current directions in psychological science. 1993;2(3):96–100. doi: 10.1111/1467-8721.ep10770953. [DOI] [Google Scholar]
- 27.Goodman CR, Shippy RA. Is it contagious? Affect similarity among spouses. Aging Ment Health. 2002;6(3):266–74. doi: 10.1080/13607860220142431. [DOI] [PubMed] [Google Scholar]
- 28.Bluvol A, Ford-Gilboe M. Hope, health work and quality of life in families of stroke survivors. J Adv Nurs. 2004;48(4):322–32. doi: 10.1111/j.1365-2648.2004.03004.x. [DOI] [PubMed] [Google Scholar]
- 29.Van Puymbroeck M, Rittman MR. Quality-of-life predictors for caregivers at 1 and 6 months poststroke: Results of path analyses. J Rehabil Res Dev. 2005;42(6):747–60. doi: 10.1682/JRRD.2005.01.0025. [DOI] [PubMed] [Google Scholar]
- 30.Saban KL, Sherwood PR, DeVon HA, Hynes DM. Measures of psychological stress and physical health in family caregivers of stroke survivors: a literature review. J Neurosci Nurs. 2010;42(3):128–38. doi: 10.1097/jnn.0b013e3181d4a3ee. [DOI] [PubMed] [Google Scholar]
- 31.McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36(10):2181–6. doi: 10.1161/01.STR.0000181755.23914.53. [DOI] [PubMed] [Google Scholar]
- 32.Haley WE, Roth DL, Hovater M, Clay OJ. Long-term impact of stroke on family caregiver well-being: a population-based case-control study. Neurology. 2015;84(13):1323–9. doi: 10.1212/wnl.0000000000001418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kamel AA, Bond AE, Froelicher ES. Depression and caregiver burden experienced by caregivers of Jordanian patients with stroke. Int J Nurs Pract. 2012;18(2):147–54. doi: 10.1111/j.1440-172X.2012.02011.x. [DOI] [PubMed] [Google Scholar]
- 34.Lau CG, Tang WK, Wong KS, Mok V, Ungvari GS. Predictors of the depressive symptomatology of the family caregivers of Chinese stroke patients in Hong Kong. J Psychiatr Ment Health Nurs. 2012;19(4):285–93. doi: 10.1111/j.1365-2850.2011.01782.x. [DOI] [PubMed] [Google Scholar]
- 35.Draper P, Brocklehurst H. The impact of stroke on the well-being of the patient’s spouse: an exploratory study. J Clin Nurs. 2007;16(2):264–71. doi: 10.1111/j.1365-2702.2006.01575.x. [DOI] [PubMed] [Google Scholar]
- 36.Godwin KM, Swank PR, Vaeth P, Ostwald SK. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging Ment Health. 2013;17(4):423–31. doi: 10.1080/13607863.2012.756457. [DOI] [PMC free article] [PubMed] [Google Scholar]