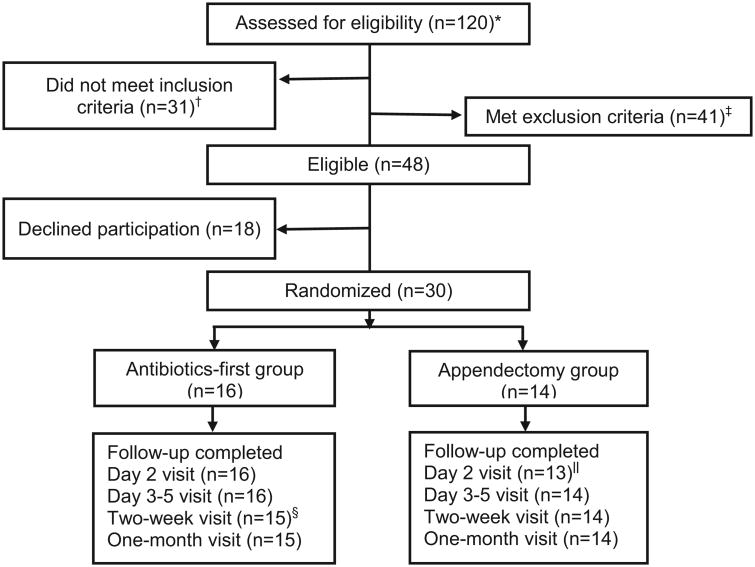
Figure 1.
Screening, randomization, and follow-up of patients with the ED diagnosis of appendicitis.
*All patients with a presumptive emergency department diagnosis of appendicitis by an emergency medicine attending physician.
†Of the 31 patients who did not meet inclusion criteria, 11 had imaging that was interpreted as equivocal for appendicitis, 5 had imaging that was interpreted as equivocal for distinguishing complicated from uncomplicated appendicitis, 10 had imaging that was interpreted as complicated appendicitis, 4 had imaging suggesting acute uncomplicated appendicitis but did not have clinical confirmation by a surgeon, and 1 did not speak English or Spanish.
‡Of the 41 patients who met exclusion criteria, 23 had an appendicolith, 11 had intravenous antibiotics >6 hours prior to enrollment, 2 were prisoners, 2 had ulcerative colitis, 1 had high-risk diabetes, 1 was immunocompromised, and 1 had another infection that required antibiotic treatment. Radiographic identification of an appendicolith was initially an exclusion criterion but was later allowed (after 11 of 30 participants were enrolled) because of lack of consistent evidence of this being a risk factor for antibiotic failure.
§One antibiotics-first participant was lost to follow-up at the day 10-18 visit.
‖One appendectomy participant was intubated at the day 2 visit, so the visit was not completed.