Abstract
Background
The current standard of care for newly diagnosed glioblastoma (GBM) is surgical resection, followed by radiation therapy (RT) with concurrent and adjuvant temozolomide chemotherapy (TMZ-CHT). The patients outcome is still poor. In this study we evaluated hypofractionated radiation therapy (HFRT), instead of standard fractionated radiation therapy, with concomitant and adjuvant TMZ chemotherapy, in terms of safety and effectiveness.
Methods
Patients with newly diagnosed GBM, Karnofsky performance scale (KPS) ≥70, and tumor up to 10 cm underwent maximal feasible surgical resection were treated. HFRT consisted of 60 Gy, in daily fractions of 4 Gy given 5 days per week for 3 weeks. The primary endpoints were overall survival (OS), progression free survival (PFS), and incidence of radiation induced brain toxicity. Secondary endpoint was the evaluation of neurocognitive function.
Results
A total of 97 patients were included in this phase II study. The median age was 60.5 years (range 23-77 years). Debulking surgery was performed in 83.5% of patients, HFRT was completed in all 97 patients, concurrent and adjuvant TMZ in 93 (95.9%). The median number of TMZ cycles was six (range 1-12 cycles). No severe toxicity occurred and the neuropsychological evaluation remained stable. At a median follow up time of 15.2 months the median OS time, 1,2-year OS rate were 15.9 months (95% CI 14-18), 72.2% (95% CI 62.1-80) and 30.4% (95% CI 20.8-40.6). Age, KPS, MGMT methylation status, and extent of surgical resection were significant factors influencing the outcome.
Conclusion
HFRT with concomitant and adjuvant TMZ chemotherapy is an effective and safe treatment.
Keywords: glioblastoma, hypofractionated radiation therapy, temozolomide, phase II, surgery
INTRODUCTION
The standard of care for newly diagnosed glioblastoma multiforme (GBM) consists of surgical resection, followed by radiation therapy (RT) with concurrent and adjuvant temozolomide chemotherapy (TMZ-CHT). This approach affords a median overall survival (OS) time and a two years OS rate of 14.6 months and 26.5%, respectively [1, 2]. Although, the addition of CHT to RT has led to a survival advantage of two months on the average, the results are still unsatisfactory, and any improvement in this field is mandatory. Increasing evidence indicates that more extensive surgical resection, at least ≥80%, is associated with a longer life expectancy, which become more prominent when the extent of resection (EOR) reaches 95%–100% of the tumor contrast enhancement area [3, 4]. To date, all the attempts to enhance the efficacy of RT were unsuccessful. Dose escalation up to 90 Gy using conventional fractionation or stereotactic radiosurgery boost did not lead to any improvement in outcome, and in most series local recurrence occurred within the high-dose regions [5–10]. The impact of hypofractionated radiation therapy (HFRT) has been investigated as well. The delivery of a higher dose per fraction over a shorter time frame has the advantages to achieve an increase in cells killing and a reduction in accelerated tumor cell repopulation. The initial experiences were carried out in elderly and frail patients with the aim to reduce the overall treatment time in this poor-prognosis subgroup [11–13]. The patients outcome were equivalent to conventional fractionation, although a lower total doses were used. More recently, HFRT has been employed in newly diagnosed GBM patients with a curative aim [14–18]. Retrospective and prospective studies showed that this approach shares similar feasibility and safety results as standard RT schemes, without a growing incidence of neurological toxicity. Nowadays, the impact of HFRT should be investigated in the setting of a multimodality approach which combines concurrent CHT and RT. Consequently, we designed a prospective phase II trial consisting of postoperative HFRT with concurrent and adjuvant TMZ-CHT, following surgical resection, to explore the impact of HFRT on GBM outcome in the modern era. Primary endpoints of the study were overall survival (OS), progression free survival (PFS), and incidence of radiation induced brain toxicity. Secondary endpoint was the evaluation of neurocognitive function.
RESULTS
Patients and treatments
From August 2013 to December 2015, out of 125 HGG patients enrolled into the trial, 97 were newly diagnosed GBM. Patients and tumor characteristics are shown in Table 1. Debulking surgery was performed in 80 (82.5%) patients and biopsy in 17 (17.5%). HFRT was carried out in all 97 patients. Concurrent and adjuvant TMZ was performed in 93 (95.9%) patients and omitted in 4 (4.1%) for liver disorders, pulmonary distress, or hematologic toxicity. Characteristics and intensity of treatments are detailed in Table 2. The median follow up time for the whole cohort was 15.2 months (range 3.2-36.8) and 20.2 months (13.1-36.8) for the alive patients.
Table 1. Patients and tumor characteristics.
| n | % | |
|---|---|---|
| Patients | 97 | 100 |
| Gender | ||
| Female | 36 | 37 |
| Male | 61 | 63 |
| Age (years) | ||
| Median (range years) | 61 (23-74) | |
| ≤60 | 49 | 51 |
| 61-70 | 34 | 35 |
| >70 | 14 | 14 |
| KPS | ||
| 70 | 6 | 6 |
| 80 | 25 | 26 |
| 90 | 35 | 36 |
| 100 | 31 | 32 |
| RPA | ||
| III | 8 | 8 |
| IV | 13 | 14 |
| V | 76 | 78 |
| Tumor molecular profile | ||
| IDH wild type | 97 | 100 |
| MGMT methylated | 61 | 63 |
| MGMT unmethylated | 36 | 37 |
| Number of cerebral lobes involved | ||
| 1 lobe | 56 | 58 |
| 2 lobes | 30 | 31 |
| 3 lobes | 5 | 5 |
| Multifocal tumor | 6 | 6 |
| Median Volumes treated cm3 (range cm3) | ||
| CTV1 | 79 (11-197) | |
| PTV1 | 166 (34-401) | |
| CTV2 | 127 (11-321) | |
| PTV2 | 241 (34-510) | |
| Median max SUV [11C]METPET before HFRT | 3·6 (0-8·1) | |
KPS=Karnofsky performance scale; RPA=recursive partitioning analysis; IDH1=isocitrate dehydrogenase; MGMT=O-6-methylguanine-DNA methyltransferase; CTV=clinical target volume; PTV=planning target volume; HFRT= hypofractionated radiation therapy; SUV [11C]METPET= 11 carbonione Methionine-Positron Emission Tomography
Table 2. Characteristics and intensity of treatments.
| Variables | n. | % |
|---|---|---|
| Surgery: | 97 | 100 |
| GTR | 53 | 55 |
| STR | 15 | 15 |
| PR | 12 | 12 |
| Biopsy | 17 | 17 |
| HFRT: | 97 | 100 |
| Total doses/dose per fraction Gy | ||
| PTV1 | 60/4 | 100 |
| PTV2 | 42/2·8 | 100 |
| Number of fractions | 15 | 100 |
| Interruption | 0 | 0 |
| Median duration weeks (range weeks) | 3 (2.6-4.1) | |
| Chemotheraphy: | ||
| Concomitant temozolomide | 93 | 96 |
| Never started concomitant temozolomide | 4 | 4 |
| Reasons | ||
| Liver disfunction | 2 | 2 |
| Pulmonary distress | 1 | 1 |
| Hematologic disorder | 1 | 1 |
| Adjuvant temozolomide | 93 | 96 |
| Never started adjuvant temozolomide | 4 | 4 |
| Reasons | ||
| Hematologic toxicity | 2 | 2 |
| Liver disfunction | 2 | 2 |
| Median number of cycles (range) | 6 (0-12) |
GTR=gross total resection:<1 cm3 of residual tumor volume; STR=subtotal resection:1-10cm3 of residual tumor volume; PR=partial resection:>10 cm3 of residual tumor volume; HFRT= hypofractionated radiation therapy; PTV=planning target volume
Progression free survival (PFS) and overall survival analyses
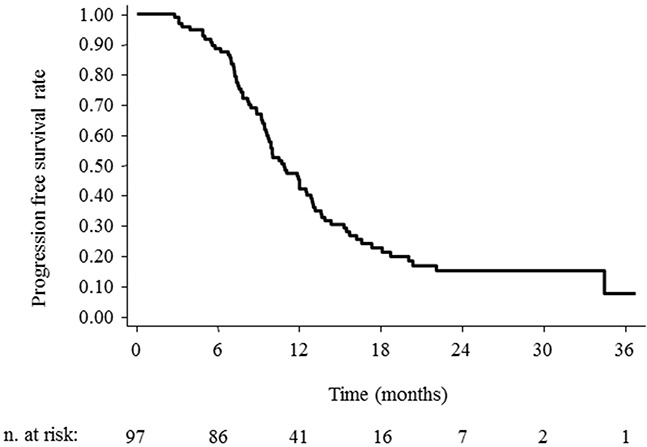
The median OS time, and the 1, 2-year OS rate were 15.9 months (95% CI 14.8-18.2), 72.2% (95%CI 62.1-80) and 30.4% (95%CI 20.8-40.6) as shown in Figure 1. At the last observation time, 29 (29.9%) patients are alive and 68 (70.1%) dead. The median PFS time, and the 1, 2-year PFS rate were 10.9 months (95% CI 9.6-12.5), 42.3% (95%CI 32.4-51.8), and 15.2% (95% CI 8.2-24.0), respectively as shown in Figure 2.
Figure 1. Overall survival for GBM cases treated with hypofractionated radiotherapy with concurrent and adjuvant temozolomide chemotherapy following any entity of surgical resection.
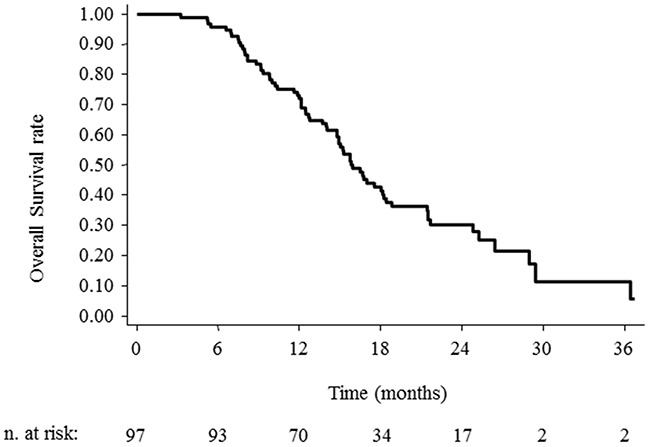
Figure 2. Progression Free Survival (PFS) for GBM cases treated with hypofractionated radiotherapy followed any entity of surgical resection.
Prognostic factors analyses
Survival according to prognostic factors, including age, gender, KPS, MGMT status, EOR, target volume, and number of adjuvant TMZ cycles, was analyzed as well. The highest benefit was observed in treated patients with age ≤60 years, KPS 100, and RPA class 3. Details are shown in Table 3.
Table 3. Kaplan-Meyer overall survival according to subgroup analyses.
| Patients | MedianOS months(months 95%CI) | 1-year OS(95%CI) | 2-year OS(95%CI) | p valueunivariate | HRmultivariate(95%CI) | p valuemultivariate | |
|---|---|---|---|---|---|---|---|
| Overall survival | 97 | 15.9 (14.8-18.2) | 72.2 (62.1-80) | 30.4 (20.8-40.6) | |||
| Gender | |||||||
| Female | 36 | 15.2 (10-18.2) | 58.3 (40.7-72.4) | 23.2 (10.5-38.8) | 0.24 | 0.78 | 0.36 |
| Male | 61 | 16.7 (14.8-21.7) | 80.3 (68-88.3) | 34.5 (21.6-47.7) | |||
| Age | |||||||
| ≤60 | 49 | 18.4 (14.9-24.8) | 79.6 (65.4-88.5) | 37.3 (23-51.7) | 0.03 | 1.39 | 0.28 |
| >60 | 48 | 14.9 (12-16.7) | 64.6 (49.4-76.3) | 23.2 (11.5-37.2) | |||
| KPS | |||||||
| 70 | 6 | 9.1 (7.9-ne) | 33.3 (4.6-67.6) | 0 | <<0.01 | 0.95 | <0.01 |
| 80 | 25 | 12.7 (10-15.8) | 68 (46.1-82.5) | 13 (2.7-31.8) | |||
| 90 | 35 | 14.9 (12-16.5) | 65.7 (47.6-78.9) | 24 (11.1-39.7) | |||
| 100 | 31 | 25.2 (18.4-ne) | 90.3 (72.9-96.8) | 56.9 (35.2-73.7) | |||
| RPA | |||||||
| III | 8 | nr | 100 | 68.6 (21.3-91.2) | 0.02 | 1.35 | 0.30 |
| IV | 13 | 15.2 (9.1-ne) | 76.9 (44.2-91.9) | 26 (6.3-51.7) | |||
| V | 76 | 15.7 (12.7-18) | 69.3 (57.6-78.4) | 27.5 (17-38.9) | |||
| EOR | |||||||
| GTR | 53 | 17 (15.2-21.4) | 81.1 (67.8-89.4) | 31.4 (18.1-45.6) | 0.13 | 1.27 | 0.04 |
| STR | 15 | 15.9 (9.8-26.4) | 73.3 (43.6-89.1) | 35.6 (12.1-60.3) | |||
| PR | 12 | 14.8 (8.8-21.5) | 75 (40.9-91.2) | 13.9 (0.9-44.1) | |||
| Biopsy | 17 | 9.3 (7-ne) | 41.2 (18.6-62.6) | 29.4 (10.7-51.2) | |||
| MGMT | |||||||
| Methylated | 61 | 18 (14.8-21.7) | 75.4 (62.6-84.4) | 35.4 (22.7-48.4) | 0.07 | 0.58 | 0.04 |
| Unmethylated | 36 | 14.9 (11.8-16.7) | 66.7 (48.8-79.5) | 21.8 (9.1-38.1) |
KPS= Karnofsky performance scale; RPA=recursive partitioning analysis; EOR=extent of resection;
GTR=gross total resection:<1 cm3 of residual tumor volume; STR=subtotal resection:1-10cm3 of residual tumor volume;
PR=partial resection:>10 cm3 of residual tumor volume; MGMT=O-6-methylguanine-DNA methyltransferase; nr=not reached; ne=not evaluable.
Postoperative assessment
No mortality or major peri-operative morbidity occurred. Postoperative new neurological deficits were observed in eight (8.2%) patients, in two cases recovered during RT treatment; they consisted in motor deficit in three, hemianopsia in two, aphasia in two, and motor deficit plus hemianopsia in one patient.
CHT-HFRT side effects
All patients completed the scheduled HFRT plan; a transient neurological deterioration was recorded in two patients, consisting of partial seizure and aphasia. Grade I-II radionecrosis (RN) occurred in 22 (22.7%) patients. No Grade III- IV radionecrosis were observed. Fatigue was observed in 55 (56.7%) patients during concurrent CHT-HFRT. Grade 2-4 hematologic toxicity was recorded in 12 (12.9%) patients, in three during concomitant treatment and in nine patients during adjuvant TMZ. No thromboembolic events or cerebral hemorrhage occurred.
Neuropsychological evaluation
lNeuropsychological scores before and after HFRT remained unchanged. The analysis showed no detrimental effect of HFRT on cognitive functions (language, short and long term verbal and visuo-spatial memory, working memory, attentive and executive functions). Particularly, a significant performance improvement was detected: between T0 and T1 in the copy of the figure test (p value<<0.01), in the recall of the complex figure tests (p value <<0.01), in the ideomotor apraxia test (p=0.03), and in the trail making test part A (p value=0.04); between T1 and T2 in the ideomotor apraxia test (p value=0.02) and in the trail making test part B-A (p value=0.01) (Table 4).
Table 4. Neuropsychological outcome.
| Cognitive domains | Test | T0 | T1 | T2 | T3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before HFRT | 1 month after HFRT | 6 months after HFRT | 12 months after HFRT | |||||||||
| n. | mean | n. | mean | p value(T0-T1) | n. | mean | p value(T0-T2) | n. | mean | p value(T0-T3) | ||
| Language | Token | 85 | 29.1 | 80 | 29.7 | 0.1 | 33 | 28.5 | 0.2 | 12 | 28.5 | 0.50 |
| Picture Naming | 85 | 42.2 | 85 | 43.7 | 0.07 | 33 | 43.5 | 0.43 | 12 | 42.9 | 0.71 | |
| Fonological fluency | 75 | 20.5 | 73 | 22.6 | 0.12 | 31 | 20.3 | 1.0 | 11 | 20.2 | 0.95 | |
| Semantic Fluency | 74 | 29.7 | 73 | 32.6 | 0.05* | 31 | 32.1 | 0.13 | 11 | 32.7 | 0.21 | |
| Memory | Digit span forward | 85 | 5.0 | 79 | 5.1 | 0.31 | 32 | 4.9 | 0.68 | 11 | 4.8 | 1.00 |
| Corsi span forward | 85 | 4.0 | 80 | 4.1 | 0.22 | 34 | 4.3 | 0.18 | 11 | 4.0 | 0.75 | |
| Digit span backward | 85 | 3.2 | 79 | 3.4 | 0.14 | 33 | 3.5 | 0.93 | 11 | 3.4 | 0.63 | |
| Corsi span backward | 84 | 3.5 | 80 | 3.7 | 0.11 | 32 | 3.7 | 0.80 | 12 | 3.4 | 0.45 | |
| Rey's 15 words test - immediate | 72 | 29.7 | 67 | 30.4 | 0.42 | 29 | 29.8 | 0.32 | 11 | 31.8 | 0.29 | |
| Rey's 15 words test - delayed | 72 | 5.0 | 66 | 5.1 | 0.96 | 28 | 5.1 | 0.53 | 11 | 5.5 | 0.55 | |
| Recall complex figure | 78 | 9.8 | 78 | 12.0 | <<0.01* | 32 | 13.4 | 0.01 | 12 | 12.9 | 0.20 | |
| Visuo-constuctional abilities | Copy of the figure | 78 | 25.7 | 78 | 28.1 | <<0.01* | 31 | 27.7 | 0.49 | 12 | 29.3 | 0.24 |
| Apraxia | Ideomotor apraxia | 85 | 66.0 | 79 | 66.2 | 0.03* | 31 | 67.4 | 0.02* | 12 | 56.2 | 0.33 |
| Orofacial apraxia | 84 | 19.2 | 78 | 19.4 | 0.16 | 31 | 19.3 | 0.30 | 12 | 19.2 | 0.32 | |
| Attention and executive functions | Trail Making test - a | 34 | 54.9 | 38 | 50.1 | 0.04* | 23 | 52.7 | 0.78 | 8 | 44.6 | 0.32 |
| Trail Making test - b | 31 | 169.8 | 37 | 168.8 | 0.08 | 21 | 157.8 | 0.06 | 6 | 150.2 | 0.18 | |
| Trail Making test - b-a | 31 | 114.8 | 37 | 123.5 | 0.26 | 21 | 105.9 | 0.01* | 6 | 108.1 | 0.18 | |
| Attentive matrices | 84 | 41.3 | 80 | 41.6 | 0.37 | 33 | 40.7 | 0.70 | 12 | 37.4 | 0.08 | |
| Stroop Test - error | 70 | 2.0 | 72 | 1.2 | 0.30 | 28 | 1.8 | 0.62 | 10 | 2.9 | 0.95 | |
| Stroop Test - time | 70 | 28.7 | 72 | 28.9 | 0.56 | 28 | 35.1 | 0.71 | 10 | 52.3 | 0.41 | |
| Raven coulored progressive matrices | 80 | 26.3 | 74 | 27.2 | 0.24 | 31 | 27.6 | 0.22 | 10 | 29.1 | 0.47 | |
HFRT=hypofractionated radiation therapy; N=number of patients; mean= age-education-adjusted score for each test and for each time point;
T0: before HFRT; T1:1 month after HFRT; T2:6 months after HFRT; T3:12 months after HFRT; * significant p values (p ≤ 0·05)
Treatment at progression
Brain progression occurred in 77 (79.4%) patients and a salvage treatment was performed in 34 (44.2%). It consisted in surgery alone in one, radiation therapy alone in one, surgery with sequential chemo-radiotherapy in five and second line chemotherapy alone in 26. The chemotherapeutic agents more frequently used were fotemustine and temozolomide. The median survival time from progression was 8.5 months (95% CI 5.4-11.4).
DISCUSSION
Based on the results of the phase III EORTC-NCIC trial, the current standard treatment for newly diagnosed GBM patients consists of radiotherapy with concomitant and adjuvant TMZ-CHT [1]. Fractionated conformal three-dimensional radiotherapy (3DCRT) to a total dose of 60 Gy in 30 daily fractions of 2 Gy each is employed based on the results from previous dose exploratory studies [19]. The use of protracted RT schedules harbors the theoretical drawback of allowing a cell repopulation, which could be of relevance in tumors with a rapid doubling time such as GBM [20]. This effect may be seen in routine clinical practice as well, where a widely rate of patients, up to 10%, discontinues RT for disease progression [1]. Hypofractionated radiation therapy (HFRT) offers the advantages of achieving an increased cells killing action, by the delivery of a higher dose per fraction over a shorter time frame, and of reducing the effect of accelerated tumor cell repopulation by shrinking the RT treatment time. Based on these observations, we designed this phase II study to assess the feasibility and the effectiveness of HFRT schedule within a multimodal therapeutic approach, including concurrent and adjuvant TMZ-CHT, following surgical resection. Although the initial study design included all grade of HGG, we report here the analysis of the newly diagnosed IDH wild type GBM patients only, to deal with a highly homogeneous population. To now, few data are available in GBM patients on the impact of HFRT used to radical doses into a multimodal strategy including surgery, concomitant and adjuvant chemotherapy [14–18]. The published studies are often phase I investigation, with a limited number of cases treated, quite heterogeneous for patients and tumors characteristics. However, the preliminary results were promising, with a median OS up to 20 months in some series, and with a low incidence of symptomatic radionecrosis or severe neurologic side effects. Table 5 showed some of the most relevant phase I-II studies about this issue. There is no agreement about the optimal HFRT doses to deliver and the schedule to employ. With the aim to improve the impact on outcome, a therapeutic effective dose greater than that of conventional radiotherapy (BED10 84Gy vs 72Gy) was applied. Our results compare favorably with previous reports regarding standard RT treatment [1], with a median OS time, 1, 2-year OS rate of 15.8 months, 72.2% and 28.5%, and a median PFS time, 1, 2-year PFS rate of 10.8 months, 42.3% and 16%, respectively, as shown in Table 6. Employing this approach, notwithstanding a higher dose on large tumor volume was delivered, all patients completed HFRT treatment, no neurological deterioration was observed and neurocognitive functions remained stable or in some cases improved, as shown by neuropsychological evaluation. Published data suggest an increased incidence of grade III-IV radionecrosis when a high dose per fraction and therapeutic effective doses are used, ranging from 3% to 20% according to the various scheme utilized [21, 22]. In our analysis only grade I-II toxicity was recorded and in no patients grade III-IV was detected. Several prognostic factors were investigated. As in many other published studies, in our series age was a factor strongly influencing survival (p=0.01). The greater benefit of treatment was observed in patients younger than 60 years, with a percentage of 40% alive at two years. Along with age, KPS was found to significantly affect outcome as well, with more than 50% of patients with KPS 100 surviving beyond two years (p=<<0.01). The extent of surgical resection has been commonly considered as a factor affecting outcome in GBM patients [3, 4, 23]. Different methodologies to define the amount of tumor removal have been used. In our study, we defined three groups of patients in relation to the RTV. A favorable trend was observed in case of RTV <10 cm3 that was obtained in about 70% of patients (p=0.03). Although an extensive surgical resection was performed in the largest number of patients treated, no major perioperative morbidity occurred and adjuvant treatments was started without delays. Literature data proved that postoperative neurological functions are crucial elements for patient quality of life (QoL) and OS. As reported by McGirt et al, new motor or language deficits are associated with significant decreases in the median survival of patients with GBM supporting the need of coupling maximal tumor resection with preservation of neurological integrity [24]. Considering the small size of RTV and the absence of major neurological deficit, no increase in corticosteroid drugs or AED dosage was needed during concomitant chemo-radiotherapy, and the HFRT was well tolerated along all treatment period. One might speculate that a radiotherapy intensification jeopardizes the patient ability of completing an adequate adjuvant chemotherapy treatment. In our cohort, TMZ was successfully administered to 96% of patients, and more than 50% of them received more than 6 cycles. In addition, salvage treatment at progression was done in about 45% of patients and the median survival of patients was 8.5 months, clearly higher respect to other series [1, 2]. We are aware that our study does not reach the power of a randomized trial in terms of sample size and longer follow up time. Nevertheless, the results shown indicates that HFRT is a feasible and safe approach, affording good survival rates, and considerable decrease in the treatment time (from 6 to 3 weeks), which could be relevant in a group with short life expectancy, such as GBM patients. Subjects who had the greatest benefit are those with young age, good performance status, maximal safe resection, and a MGMT methylated tumor. Open questions remain the optimal radiation total doses to deliver and the schedule to utilize, but HFRT within a multimodal therapeutic approach, seems a way forward to improve the outcome of patients with glioblastoma.
Table 5. Published studies regarding hypofractionated radiation therapy.
| Authors | N pts | Study design | Concurrent and adjuvant TMZ | Total dose | N frs | RN | Median OS | 1 yearOS % | 2 yearsOS % |
|---|---|---|---|---|---|---|---|---|---|
| Chen (14) | 16 | Phase I | yes | 60 Gy | 20151210 | 1 G43 G3 | 16.3 months | nr | nr |
| Terasaky (16) | 26 | Pilot | yes | 45 Gy | 15 | no | 15.6 months | nr | nr |
| Reddy (15) | 24 | Phase II | yes | 60 Gy30 Gy | 1010 | no | 16.6 months | nr | nr |
| Jastaniyah (17) | 25 | Phase I | yes | 60 Gy | 22 | no | 15.7 months | 62 | 9 |
| Iuchi (18) | 46 | Phase II | yes | 68 Gy40 Gy32 Gy | 888 | 20 G3 | 20 months | 50 | 41 |
Pts=patients; TMZ=temozolomide; frs=fractions; RN=radionecrosis; OS=overall survival; no=not observed; nr=not reported
Table 6. comparison between standard (6 weeks) radiation therapy (Stupp et al. [1]) and hypofractionated (3 weeks) radiation therapy within multimodal approach.
| Variables | Concurrent and adjuvant TMZ CHTwith standard RT(60 Gy in 30 fractions) | Concurrent and adjuvant TMZ CHTwith hypofractionated RT(60 Gy in 15 fractions) | ||
|---|---|---|---|---|
| Extent of surgery | ||||
| Biopsy | 17% | 17.5% | ||
| Debulking | 83% | 82.5% | ||
| Radiotherapy | ||||
| Never started | 1% | 0% | ||
| Early discontinuation* | 10% | 0% | ||
| Concurrent TMZ CHT | ||||
| Never started | 2% | 4.1% | ||
| Adjuvant TMZ CHT | ||||
| Never started | 22% | 4% | ||
| Number of median cycles (range) | 3 (0-7) | 6 (0-12) | ||
| PFS | (95%CI) | (95%CI) | ||
| Median | 6.9 months | (5.8-8.2) | 10.9 months | (9.6-12.5) |
| 1year | 26.9% | (21.8-32.1) | 42.3% | (32.4-51.8) |
| 2 year | 10.7% | (7.0-14.3) | 15.2% | (8.2-24.0) |
| OS | ||||
| Median | 14.6 months | (13.2-16-8) | 15.9 months | (14.8-18.2) |
| 1 year | 61.1% | (55.4-66.7) | 72.2% | (62.1-80) |
| 2 year | 26.5% | (21.2-31.7) | 30.4% | (20.8-40.6) |
* for disease progression
TMZ=temozolomide; CHT=chemotherapy; PFS=progression free survival; OS= overall survival
MATERIALS AND METHODS
Study design and patients
The present trial was a prospective single arm phase II study approved by our institutional review board. The trial was registered at ClinicalTrials.gov site with number NCT00006353. All patients provided a written informed consent to the treatment and the use of their data for scientific purposes. Eligible patients had: 1) an age of 18-70 years and a Karnofsky performance scale (KPS) ≥60; 2) a newly diagnosed high grade gliomas (HGG); 3) a residual tumor or surgical cavity with a maximum diameter of 10 cm; 4) a normal liver, kidney and bone marrow functions. A limited number of patients older than 70 years with KPS ≥80 were included as well. We report here the analysis of GBM patient population group only.
Procedures
Surgery
Surgery was performed in all patients with the aim to maximally remove the tumor according to functional boundaries. Tumor removal was achieved with the aid of brain mapping techniques and imaging neuro-navigation (post contrast T1 weighted images, MET-PET, FLAIR, functional MRI, DTI) coupled with intraoperative ultrasounds, to afford maximal resection and maintenance of full patient functional integrity. Extent of resection (EOR) was determined by comparing preoperative post-contrast T1 weighted MRI with postoperative MRI study, acquired within 48 hours after surgery, and calculated as follows: preoperative tumor volume – postoperative tumour volume/preoperative tumor volume. Gross total resection (GTR) was defined as residual tumor volume (RTV) lower than 1 cm3, subtotal resection (STR) when RTV was among 1 and 10 cm3, and partial resection (PR) when it was greater than 10 cm3 [25]. Patients who received biopsy only were also enrolled. Tumor molecular profile was available in all cases. Immunohistochemical staining for Isocitrate dehydrogenase (IDH1/2) was performed on BenchMark XT automated tissue staining systems (Ventana Medical Systems, Inc., Tucson, AZ) using validated protocols. O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status was determined by pyrosequencing (Diatech Pharmacogenetics, MGMT plus, valid CE/IVD) [26].
Hypofractionated radiation therapy (HFRT)
CT scan, T1-weighted FLAIR (fluid-attenuated inversion recovery images) and T2-weighted 3D-FLAIR followed by T1-weighted MPRAGE MRI and [11C]-Methionine-PET (11CMETPET) were acquired for radiation therapy planning and images were co-registered each other. Pre and post-operative MRI acquired within 48 hours from surgery were used too to better define the target RT volume. Two different clinical target volume (CTV) were outlined: CTV1 corresponded to the entire surgical cavity plus eventual residual tumor after surgery or, to the abnormality on the T1-weighted post-contrast MPRAGE and 11CMETPET in case of biopsy; CTV2 corresponded to the abnormality on FLAIR MRI images before surgery. Planning target volume 1-2 (PTV1/PTV2) was generated adding an isotropic margin of 5 mm from CTV1 and CTV2 respectively. Intensity modulated radiation therapy was performed within 4-6 weeks after surgery using volumetric modulated arc therapy (VMAT). The dose prescribed was 60 Gy with daily fraction of 4 Gy on PTV1, and 42 Gy with daily fraction of 2.8 Gy on PTV2 for 15 consecutive days, using a simultaneous integrated boost (SIB). Organs at risk (OARs) outlined were optic nerves and chiasm, lens, brainstem and cochlea without additional margins, and the recommended maximal doses were ≤40 Gy, ≤10 Gy, ≤30 Gy, and ≤30 Gy, respectively. Dose was prescribed to an isodose line that ensured that more than 98% of PTV1-2 receives 95% of prescribed dose. In each session, patients position check was performed using ExacTrac (Brain Lab) system and cone beam computer tomography (CBCT).
Chemotherapy
All patients received TMZ concurrently with HFRT. TMZ was administered orally, once daily, at 75 mg/m2, starting on the first day of HFRT and continuing for the whole treatment. After a 4-week break adjuvant TMZ was administered at 150 to 200 mg/m2 orally, once daily, for 5 consecutive days every 28 days up to 12 cycles, or until disease progression occurred.
Supportive care
Corticosteroids were administered during the whole HFRT treatment and progressively reduced at the end of RT. Antiepileptic drugs (AEDs) were prescribed only in patients with a history of at least one seizure. The most frequently used AEDs were levetiracetam as first line instance followed by topiramate, lamotrigine or lacosamide.
Evaluation of clinical outcome
Clinical outcome was evaluated by neurological examination and MRI imaging 1 months after concurrent CHT-HFRT and every four months thereafter. [11C]MET-PET was performed at four and 12 months during maintenance CHT or to rule out pseudo-progression. When needed tumor progression was defined according to Response Assessment in Neuro-Oncology (RANO) working group [27]. Thirty-days postoperative morbidity and mortality were assessed. Major complications were defined as the appearance of new neurological deficits persisting for more than 30 days after surgery and requiring a prolonged hospitalization or rehabilitation. All other complications were defined as minor. The appearance of new deficits or the worsening of preoperative deficits were considered as complications. Hematologic and non-hematologic toxicities, including radionecrosis, were graded according to Common Terminology Criteria for Adverse Events version 3.0. Neuropsychological assessment was performed through a shortened version of the “Milano Bicocca Battery”, evaluating language, memory, apraxia, visuo-constructional abilities, attentive and executive functions [28]. The total time of administration was one hour on average. Patients were evaluated one week before the start of HFRT (T0), 1 (T1), 6 (T2) and 12 months (T3) thereafter or until disease progression.
Statistical analysis
The study was designed to demonstrate, with 90% power and 1 sided α error of 5%, a significant difference between a reference value of 1 year survival of 55.2% in standard treatments compared to a figure of 71.4% for the new one. Variables considered were: gender, age, KPS status, RPA class, EOR and MGMT methylated status. Age of patients was divided into two groups, respectively, ≤ 60 and >60 years. Survival and recurrence time observations were evaluated according to the method of Kaplan and Meier, starting from the date of diagnosis. The median survival time is evaluated obtained from Ŝ(t), the Kaplan –Meier product-limit estimate of the survivor function. Confidence bounds of the survivor function are calculated based on the asymptotic variance of ln[−ln Ŝ(t), as described in Kalbfleisch and Prentice. The upper (lower) confidence limits for the median survival times are defined as the first time at which the upper (lower) confidence limit for Ŝ(t) is less than or equal to 0.5. A not reached indicator (nr) was specified if the survival estimate resulted above the 50% level in the considered observation time. Upper confidence bound of median survival time was labeled as ne if not evaluable with the above method for a specific group of patients in the considered time of observation. In order to assess the prognostic role of the different individual variables, the log-rank test was used for dichotomous variables gender, MGMT and age (grouped). Univariate cox model was applied for the remaining variables. Multivariate Cox regression model was used as a method to estimate the independent association of our variable set with overall survival. Neurophysiological assessment parameters were preliminarily evaluated for a difference before and after RT. In order to assess the effect of the HFRT on neurocognitive functions a series of nonparametric analyses (Wilcoxon signed-rank test) was performed. P value and the mean of the age- and education-adjusted score for each test and for each time point (T0;T1;T2;T3) was reported. Statistical analysis was performed by the use of the Stata software, version 13.1 (Stata Corp LP, College Station TX USA). Methods and calculation details can also be found in the software refence manual in the stata website (http://www.stata.com/).
Abbreviations
- GBM
glioblastoma multiforme
- RT
radiotherapy
- CHT
chemotherapy
- EOR
estent of resection
- TMS
temozolomide
- HFRT
hypofractionated radiaton therapy
- KPS
Karnofsky performance scale
- OS
overall survival
- PFS
progression free survival
- GTR
gross total resection
- RTV
residual tumor volume
- STR
subtotal resection
- PR
partial resection
- MET-PET
methionine PET
- FLAIR
Fluid-attenuated inversion recovery
- MRI
magnetic resonance imaging
- DTI
diffusion tensor imaging
- IDH
isocitrate dehydrogenase
- MPRAGE
magnetization-prepared rapid gradient-echo
- 11CMETPET
[11C]-Methionine-PET
- MGMT
O-6-methylguanine-DNA methyltransferase
- CTV
clinical target volume
- PTV
planning target volume
- VMAT
volumetric modulated arc therapy
- SIB
simultaneous integrated boost
- OAR
organ at risk
- CBCT
cone beam computed tomography
- AED
antiepileptic drugs
- RANO
Response Assessment in Neuro-Oncology
- RPA
recursive partiotioning analysis
Footnotes
Author contributions
P. Navarria, F. Pessina coordinated the study and processed the data and supervised the analysis
S. Tomatis, L. Cozzi coordinated the data analysis
A. Chiti, A. Santoro, L. Bello, M. Scorsetti conceived the study and participated to the protocol steering
P. Navarria, F. Pessina, R. Soffietti, M. Grimaldi, E. Lopci, A. Leonetti, A. Casarotti, M. Rossi, A. Ascolese, M. simonelli. S. Marcheselli, E. Clerici contributed to the data collection, patients management and clinical activities
CONFLICTS OF INTEREST
L. Cozzi acts as Scientific Advisor to Varian Medical Systems and is Clinical Research Scientist at Humanitas Cancer Center. All other co-authors have no conflicts of interest
FUNDING
None.
REFERENCES
- 1.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoon M, Belanger K, Brandes A, Marosi C, Bogdahn U, Curschmann J, Janzer R, Ludwin S, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005(352):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 2.Stupp R, Hegi ME, Mason WP, van den Bent M, Taphoon M, Janzer R, Ludwin S, Allgeier A, Fisher B, Belanger K, Hau P, Brandes A, Gijtenbeek J, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009(10):459–466. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 3.Keles GE, Anderson B, Berger MS. The effect of extent of resection on time to tumor progression and survival in patients with glioblastoma multiforme of the cerebral hemisphere. Surg Neurol. 1999(52):371–379. doi: 10.1016/s0090-3019(99)00103-2. [DOI] [PubMed] [Google Scholar]
- 4.Sanai N, Polley MY, McDermott MW, Parsa A, Berger M. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011(115):3–8. doi: 10.3171/2011.2.jns10998. [DOI] [PubMed] [Google Scholar]
- 5.Tsien C, Moughan J, Michalski JM, Gilbert M, Purdy J, Simpson J, Kresel J, Curran W, Diaz A, Mehta M. Phase I three-dimensional conformal radiation dose escalation study in newly diagnosed glioblastoma: radiation therapy oncology group trial 98-03. Int J Radiat Oncol Biol Phys. 2009(73):699–708. doi: 10.1016/j.ijrobp.2008.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan JL, Lee SW, Fraass BA, Normolle DP, Greenberg HS, Junck LR, Gebarski SS, Sandler HM. Survival and failure patterns of high-grade gliomas after three-dimensional conformal radiotherapy. J Clin Oncol. 2002(20):1635–1642. doi: 10.1200/JCO.2002.20.6.1635. [DOI] [PubMed] [Google Scholar]
- 7.Nakagawa K, Aoki Y, Fujimaki T, Tago M, Terahara A, Karasawa K, Sakata K, Sasaki Y, Matsutani M, Akanuma A. High-dose conformal radiotherapy influenced the pattern of failure but did not improve survival in glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 1998(40):1141–1149. doi: 10.1016/s0360-3016(97)00911-5. [DOI] [PubMed] [Google Scholar]
- 8.Nieder C, Mehta MP. Advances in translational research provide a rationale for clinical re-evaluation of high-dose radiotherapy for glioblastoma. Med Hypotheses. 2011(76):410–413. doi: 10.1016/j.mehy.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka M, Ino Y, Nakagawa K, Tago M, Todo T. High-dose conformal radiotherapy for supratentorial malignant glioma: a historical comparison. Lancet Oncol. 2005(6):953–960. doi: 10.1016/S1470-2045(05)70395-8. [DOI] [PubMed] [Google Scholar]
- 10.Watkins JM, Marshall DT, Patel S, Giglio P, Herrin A, Garrett-Mayer E, Jenrette J. High-dose radiotherapy to 78 Gy with or without temozolomide for high grade gliomas. J Neurooncol. 2009(93):343–348. doi: 10.1007/s11060-008-9779-y. [DOI] [PubMed] [Google Scholar]
- 11.Malmström A, Grønberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, Abacioglu U, Tavelin B, Lhermitte B, Hegi M, Rosell J, Henriksson R. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012(13):916–926. doi: 10.1016/S1470-2045(12)70265-6. [DOI] [PubMed] [Google Scholar]
- 12.Roa W, Brasher PM, Bauman G, Anthes M, Bruera E, Chan A, Fisher B, Fulton D, Gulavita S, Hao C, Husain S, Murtha A, Petru K, et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004(22):1583–1588. doi: 10.1200/JCO.2004.06.082. [DOI] [PubMed] [Google Scholar]
- 13.Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, Mikkhah G, Papsdorf K, Steinbach J, Sabel M, Combs S, Vesper J, Braun C, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012(13):707–715. doi: 10.1016/S1470-2045(12)70164-X. [DOI] [PubMed] [Google Scholar]
- 14.Chen C, Damek D, Gaspar LE, Waziri K, Kleinschmidt-DeMasters B, Robischorn M, Stuhr K, Rusthoven K, Kavanagh B. Phase I trial of hypofractionated intensity-modulated radiotherapy with temozolomide chemotherapy for patients with newly diagnosed glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2011(81):1066–1074. doi: 10.1016/j.ijrobp.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Reddy K, Damek D, Gaspar LE, Ney D, WAziri A, Lillehei K, Stuhr K, Kavanagh B, Chen C. Phase II trial of hypofractionated IMRT with temozolomide for patients with newly diagnosed glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2012(84):655–660. doi: 10.1016/j.ijrobp.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 16.Terasaki M, Eto T, Nakashima S, Okada Y, Ogo E, Sugita Y, Tokutomi T, Shigemori M. A pilot study of hypofractionated radiation therapy with temozolomide for adults with glioblastoma multiforme. J Neurooncol. 2011(102):247–253. doi: 10.1007/s11060-010-0306-6. [DOI] [PubMed] [Google Scholar]
- 17.Jastaniyah N, Murtha A, Pervez N, Le D, Roa W, Patel S, Mackenzie M, Fulton D, Field C, Ghosh S, Fallone G, Abdulkarim B. Phase I study of hypofractionated intensity modulated radiation therapy with concurrent and adjuvant temozolomide in patients with glioblastoma multiforme. Radiat Oncol. 2013;8:38. doi: 10.1186/1748-717X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iuchi T, Hatano K, Kodama T, Sakaida T, Yokoi S, Kawasaki K, Hasegawa Y, Hara R. Phase 2 trial of hypofractionated high-dose intensity modulated radiation therapy with concurrent and adjuvant temozolomide for newly diagnosed glioblastoma. Int J Radiation Oncol Biol Phys. 2014;88:793–800. doi: 10.1016/j.ijrobp.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Walker MD, Strike TA, Sheline GE. An analysis of dose– effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979(5):1725–1731. doi: 10.1016/0360-3016(79)90553-4. [DOI] [PubMed] [Google Scholar]
- 20.Budach W, Gioioso D, Taghian A, Stuschke M, Suit M. Repopulation capacity during fractionated irradiation of squamous cell carcinomas and glioblastomas in vitro. Int J Radiat Oncol Biol Phys. 1997(39):743–750. doi: 10.1016/s0360-3016(97)00362-3. [DOI] [PubMed] [Google Scholar]
- 21.Ruben JD, Dally M, Bailey M, Smith R, McLean C, Fedele P. Cerebral radiation necrosis: incidence, outcomes, and risk factors with emphasis on radiation parameters and chemotherapy. Int J Radiat Oncol Biol Phys. 2006(65):499–508. doi: 10.1016/j.ijrobp.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Rusthoven KE, Olsen C, Franklin W, Kleinschmidt-DeMasters B, Kavanagh B, Gaspar L, Lillehei K, Waziri A, Damek D, Chen Cl. Favorable prognosis in patients with high-grade glioma with radiation necrosis: the University of Colorado reoperation series. Int J Radiat Oncol Biol Phys. 2011(81):211–217. doi: 10.1016/j.ijrobp.2010.04.069. [DOI] [PubMed] [Google Scholar]
- 23.Chaichana KL, Jusue-Torres L, Navarro-Ramirez R, Raza S, Pascual-Gallego M, Ibrahim A, Hernandez-Hermann M, Gomez L, Ye X, Weingart J, Olivi A, Blakely J, Gallia G, et al. Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 2014(16):113–122. doi: 10.1093/neuonc/not137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quiñones-Hinojosa AR. Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg. 2009(110):156–162. doi: 10.3171/2008.4.17536. [DOI] [PubMed] [Google Scholar]
- 25.Castellano A, Bello L, Michelozzi C, Gallucci M, Fava E, Iadanza A, Riva M, Casaceli G, Falini A. Role of diffusion tensor magnetic resonance tractography in predicting the extent of resection in glioma surgery. Neuro Oncol. 2012(14):192–202. doi: 10.1093/neuonc/nor188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, Plass C, Hegi M, Platten M, Reifenberger G. MGMT testing--the challenges for biomarker-based glioma treatment. Nat Rev Neurol. 2014(10):372–385. doi: 10.1038/nrneurol.2014.100. [DOI] [PubMed] [Google Scholar]
- 27.Wen PY, Macdonald DR, Reardon DA, Cloughesy T, Sorensen A, Galanis E, Degroot J, Wick W, Gilbert M, Lassman A, Tsien C, Mikkelsen T, Wong E, et al. Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol. 2010(28):1963–1972. doi: 10.1200/JCO.2009.26.3541. [DOI] [PubMed] [Google Scholar]
- 28.Papagno C, Casarotti A, Comi A, Gallucci M, Riva M, Bello L. Measuring clinical outcomes in neuro-oncology. A battery of evaluate low-grade glioma (LGG) J Neurooncol. 2012(108):269–275. doi: 10.1007/s11060-012-0824-5. [DOI] [PubMed] [Google Scholar]


